Introduction
The World Health Organization (WHO) reported oral cancer as having one of the highest mortality ratios amongst all malignancies,[1] as often its diagnosis is made only in advanced stages. The global increase in frequency and mortality of oral cancer has intensified current research efforts in the field of early detection and prevention.
Oral premalignant/precancerous lesions are defined as altered epithelium with an increased likelihood for progression to squamous cell carcinoma (SCC)[2]. The principal oral premalignant lesions which may be precursor to Oral squamous cell carcinoma are white patches (leukoplakia) and red patches (erythroplasia/erythroplakia) or mixed red and white lesions. In WHO(2005) workshop, the term potentially malignant was preferred above ‘premalignant’ or ‘precancerous’ as it conveys that not all lesions and conditions described under this term may transform to cancer, rather that there is a family of morphological alterations amongst which some may have an increased potential for malignant transformation. Furthermore, it was recommended to abandon the traditional distinction between potentially malignant lesions and potentially malignant conditions and to use the term “potentially malignant disorders” instead[3],[4]. Histologically these disorders may show varying grades of dysplasia that can be ascertained by histopathological examination using various criteria the most commonly followed being those given by Banoczy and Csiba[5] and WHO(2005)[3]. Although scalpel biopsy is the gold standard in confirmation of diagnosis, it is a technique with surgical and psychological implication for some patients.
Certain factors make scalpel biopsy a problematic procedure. As it is an invasive technique, patient often refuses to repeat the procedure during follow up period. Since scalpel biopsy is taken from one site or limited number of sites, it represents only small areas, which may not be sufficient in larger lesions. When multiple lesions are present, the one with malignant transformation would be overlooked. Thus, there is need for a more accurate, less invasive diagnostic tool that can detect early lesions and represent larger areas.
A technique of microbiopsies employing the use of a dermatological ring curette for scraping the mucosal surface of the lesion has been used in early detection of cervical cancer. A study by Mravunac M et al in 1998 on microbiopsies in non cervical smears concluded that the application of the microbiopsy technique in routine cytology smears containing microbiopsies is helpful, particularly in those cases in which the diagnosis is not clear on the basis of the cytology smear[6]. Another study by Mravunac M et al in 2000 on interpreting microbiopsies in cervical smears concluded that the processing of microbiopsies in smears with an inconclusive cytologic diagnosis or a diagnosis of atypical squamous cells of undetermined significance (ASCUS) allowed correct diagnosis in 50% of cases in this study[7].
To overcome the drawbacks of scalpel biopsies, attempts have been made to use Microbiopsies in early detection of Oral potentially malignant lesions (OPMLs) and oral squamous cell carcinoma. Thus, this study was undertaken to assess the accuracy of oral microbiopsies in the diagnosis of oral potentially malignant lesions.
Materials and Methods
The study was performed in the Department of Oral and Maxillofacial Pathology, MMCDSR, Mullana (Haryana, India). Forty patients with clinical diagnoses of OPMLs were selected for the study.
The micro-biopsies were carried out from more than one site, by scraping the surface of lesion using dermatological ring curette (Figure 1). Care was taken to cause slight bleeding so as to ensure that basal layer of epithelium had been sampled (Figure 2). The microbiopsied small tissue fragments were placed in alcoholic formalin. The curette sampling was immediately followed by scalpel biopsy. Both the curettage specimens and scalpel biopsy specimens were processed routinely and sections stained with hematoxylin and eosin. The slides were coded to prevent any bias during histopathological examination. The microbiopsies with only superficial layers of epithelium were considered inadequate.
 | Figure 1. Photograph Showing Sampling The Surface Of Lesion Using Dermatological Ring Curette
 |
 | Figure 2. Photograph Showing Bleeding Points Obtained During Scraping Procedure Which Ensured The Inclusion Of Basal Layer Of Epithelium
 |
Dysplasia was recorded as either positive or negative using Banoczy and Csibacriteria[5] (Table 1). Grading of epithelial dysplasia was graded as positive when 2 or more of the listed histological changes were present and as negative when 0 or less than 2 changes were present. Diagnoses other than dysplasias were specified. The histological diagnoses obtained by microbiopsies were compared to confirmatory diagnosis by scalpel biopsy (Figure 3) for evaluating the accuracy of diagnosis by microbiopsy procedure. The same were also statistically analysed for specificity and sensitivity.
![Table 1: Criteria for diagnosis of epithelial dysplasia[5]](article-image-4502-TABLE_1_CRITERIA_FOR_DIAGNOSIS_OF_EPITHELIAL_DYSPL.jpg) | Table 1: Criteria for diagnosis of epithelial dysplasia[5]
![Table 1: Criteria for diagnosis of epithelial dysplasia[5]](images/article-image-enlarge.jpg) |
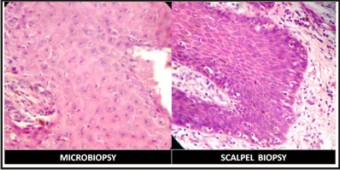 | Figure 3. Photomicrograph Showing Epithelial Dysplasia Diagnosed By Two Procedures (H & E, 40 X)
 |
Results
Out of the forty cases taken, the curette samples were inadequate for microbiopsy assessment in three cases, which were excluded from the study. For two cases, no result of scalpel biopsy was available for comparison as patient refused the procedure. Thus a total of 35 cases with adequate microbiopsy specimen were available for comparison. Dysplasia was accurately diagnosed in all 21 cases of dysplasia diagnosed by scalpel biopsy. Three cases that were diagnosed as oral submucous fibrosis (Figure 4) and seven as hyperkeratotic lesion (Figure 5) by microbiopsy were also in agreement with the diagnoses obtained by scalpel biopsy. Four cases were diagnosed positive for dysplasia with micro-biopsy but did not show any dysplasia in the scalpel biopsy (Table 2). Accuracy of diagnosis by microbiopsy was calculated in percentage as follows:-
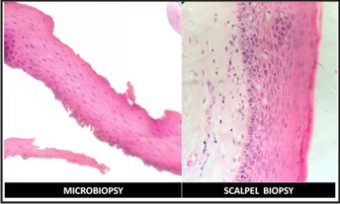 | Figure 4. Photomicrograph Showing Oral Submucous Fibrosis Diagnosed By Two Procedures (H & E, 40 X)
 |
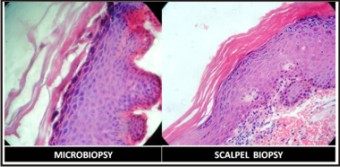 | Figure 5. Photomicrograph Showing Hyperkeratotic Lesion Diagnosed By Two Procedures
 |
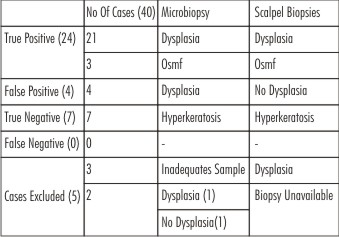 | Table 2: Distribution Of 40 Cases Diagnosed By Microbiopsy And/Or Scalpel Biopsy
 |
Accuracy (%) = Number of cases in agreement with scalpel biopsy X 100
Total number of cases available for comparison
31 out of 35 cases were found to be in agreement with the diagnoses by scalpel biopsy, giving an accuracy of 88.57%. Percentage of Inadequate sample was calculated as follows:-
Inadequate Samples(%) = Number of inadequate samples X 100
Total number of cases sampled
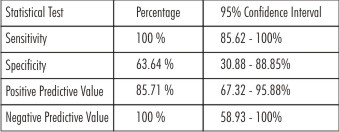
In the present study, three out of forty cases were inadequate for evaluation (7.5 %). The sensitivity of microbiopsy procedure was 100% and specificity was 63.64% (Table 3).
 | Table 3: Table Showing Statistical Analysis Of 35 Adequate Samples
 |
Discussion
The histopathological diagnosis of OPMLs by biopsied material (incisional biopsy) is the classical and the most accepted diagnostic method. While conventional oral examination may be useful in the diagnosis of some oral lesions, it does not identify all OPMLs. Furthermore, microscopic investigation of the progressive cancer is often conducted too late for successful intervention.[8] Although brush biopsy and other cytology techniques have proven to be an adjunct in histopathological diagnosis of oral lesions, many studies have also suggested that they produce conflicting results. This further confirms the need for a universally accepted early diagnostic tool aid for oral oncologists.
A dermatological ring curette was used to obtain small tissue fragments from the oral lesions in the same manner as it is used in dermatology for skin and mucosal lesions.[9] The sharp edges of curette help in easy scraping from the whole surface of the lesion without applying much pressure and minimal trauma.
As in our research work, curette sampling is more acceptable than scalpel biopsy procedure thus reducing patient stress. Two out of forty subjects refused a scalpel biopsy while they had no qualms about a curettage procedure. This further allows the diagnostic procedure to be carried out from larger surface of lesion. Also, the samples can be obtained from multiple sites, including also those with low index of suspicion. This is also of major importance in follow up of OPMLs and in lesions involving multiple areas, such as oral lichen planus or proliferative verrucous leukoplakia, as these lesions require repeated evaluation to check for any malignant transformation.
The criteria for grading of epithelial dysplasia give by Banoczy and Csiba was used in this study as this is a simple and efficient method for grading dysplasia and could be easily used on curetted tissues.[5]
The oral microbiopsy technique used in the present study gave promising results as obtained by the standard scalpel biopsy procedure with an accuracy of 88.57%. Navone Ret al in 2007, in a similar study regardingimpact of liquid-based oral cytology on the diagnosis of oral squamous dysplasia and carcinomas using a dermatological curette to allow for the collection of 'accidental' tissue fragments, utilized as microbiopsies, found that there were 8.8% of inadequate specimens in the liquid-based cytology group; sensitivity was 95.1% and specificity was 99.0%.[10] Comparable results were seen in the present study with a sensitivity of 100% and a positive predictive value of 85.71%. The specificity of 63.64% with a negative predictive value of 100% was seen.
In a study done by Poilehero et al (2003) an under diagnosis of dysplasia / carcinoma cases ranging from 28.3% to 4.4 % has been reported by scalpel biopsy procedure,[11] which could be attributed to limited sample area or non-representative site. In our study, out of forty cases, four showed the presence of dysplasia in microbiopsy but was negative in scalpel biopsy, which could be due to the scalpel biopsy not being from the representative area.
Another favorable point is that microbiopsy sampling involved a limited loss of tissue and did not interfere with evaluation by scalpel biopsy procedure. But at the same time, it may yield inadequate samples, so no diagnosis can be made. In the present study, 4 cases were inadequate for evaluation (7.5%). Thus, the reduced thickness of tissue and lack of proper orientation may become the limitations of this procedure.
Conclusions
Based on above facts we conclude that microbiopsy may prove to be a practicable first level diagnostic aid for OPMLs. Microbiopsies can help in screening of oral lesions to identify representative areas for further procedures and also early detection of dysplastic/ carcinomatous changes. Oral microbiopsy being a simple, minimally invasive procedure can also be used for examining multiple lesions in individuals and also screening of large populations with great accuracy. It can be used in follow up of cases of OPMLs with less psychological distress to patients. However, further investigations with more number of study samples will be needed to establish this technique as a routine diagnostic aid.
Thus microbiopsies could help in overall improvement in sensitivity for diagnosing of oral dysplasias/carcinomas of oral cavity.
References
1. Parkin DM, Bray F, Ferlay J, Pisani P. Estimating the world cancer burden: Globocan. Int J Cancer 2001;94:153–6.
2. Warnakulasuriya S, Johnson NW, van der Waal I. Nomenclature and classification of potentially malignant disorders of the oral mucosa. J Oral Pathol Med 2007;36:575–80.
3. Barnes L, Eveson JW, Reichart PA, Sidransky D. World Health Organization classification of tumours. Pathology and genetics. Head and neck tumours. World Health Organization; 2005.
4. Van der Waal I. Potentially malignant disorders of the oral and oropharyngeal mucosa; terminology, classification and present concepts of management.Oral Oncol 2009;45:317–323
5. Bancoczy J, Csiba A. Occurrence of epithelial dysplasia in oral leukoplakia – Analysis and follow-up study of 120 cases. Oral Surg Oral Med Oral Pathol 1976; 42(6):766-74.
6. Mravunac M, Verbeek D, van Heusden C, Reuterink A, Hop G, Smedts F. Applications of the microbiopsy technique in non-cervical cytology: where cytology and histology meet.Histopathology 1998 Aug;33(2):174-82
7. Mravunac M, Smedts F, Philippi A, Remerij D, Krul A, Schrik M, van't Hof B, van Heusden C, Vooijs GP. Interpreting microbiopsies in cervical smears. A cytohistologic approach.Acta Cytol.2000 Sep-Oct;44(5):752-9.
8. Just T, Stave J, Kreutzer HJ, et al Confocal microscopic evaluation of epithelia of the larynx. Laryngorhinootologie 2007;86:644–8.
9. Lawrence, Clifford M. Introduction to Dermatological Surgery. 2nd ed. Churchill Livingstone; 2002.
10. Navone R, Burlo P, Pich A, Pentenero M, Broccoletti R, Marsico A, Gandolfo S. The impact of liquid-based oral cytology on the diagnosis of oral squamous dysplasia and carcinoma.Cytopathology 2007 Dec;18(6):356-60.
11. Poilehero M Carrozzo M, Pagano M, et al. Oral mucosal dysplastic lesions and early squamous cell carcinoma:underdiagnosis from incisional biopsy. Oral Dis 2003;9:68-72.
|