Introduction
Rochette in 1973 proposed adhesively bonded splints with macromechanical retention through perforated retainers.[1] Later, Howe and Denehy[2] used this technique for an anterior fixed partial denture, and Livaditis[3] described this technique for posterior tooth replacement.
The main advantages of the RBFPDs are reduced pulpal morbidity caused by minimal tooth preparation, as well as less gingival inflammation resulting from supragingival placement of the margins.[4] In addition, chairside time and laboratory costs are reduced compared to conventional prostheses.[5]
Introducing a minimally invasive preparation design with large surface areas for bonding and vertical grooves improved the survival rates of RBFPDs.[5],[6] In addition, several retentive systems for bonding composite resin to metal were developed. However, clinical results showed unsatisfactory retention rates for RBFPDs. Several studies evaluated the biomechanics of tooth preparation and framework design in relation to the success rate of RBFPDs and considered retention and resistance form essential for increasing the clinical retention of RBFPDs.[7],[8] Consequently, the original design of RBFPDs which involved no tooth preparation gradually went through a number of changes such as preparation of proximal grooves, occlusal rest seats, and lingual wings.[7] Other modifications like incorporation of pins (pin-retained RBFPDs)[9], retentive slots and inlay preparations[10] were also proved to be effective.
These new modified designs, however, are less conservative than the designs that have been previously used. Therefore, prior to prescribing these designs for the replacement of the posterior teeth in the partially edentulous patients, it is prudent to evaluate their retention in an in vitro study. The purpose of this in vitro study was, therefore, to compare the retention of the two modified designs of the RBFPDs with that of the conventional RBFPDs and to assess their suitability for use as an alternative to partial or full coverage retainers, wherever, indicated.
Material and Method
Ninety freshly extracted human teeth (forty five 2nd premolars and 2nd molars) were employed in the study. Each selected tooth received two grooves on the mesial and distal surfaces of its root prior to being embedded in the resin. The grooves were placed in the roots in order to secure them in place in the resin base [self-cure acrylic resin (DPI-RR Cold cure, DPI, Mumbai, India)] during the tensile test. Specimens were then prepared by mounting one premolar and one molar with a space equivalent to 1st molar tooth between them in the resin base, with the long axis of the tooth perpendicular to the horizontal plane, at dough stage. All the specimens were preserved in distilled water until further use.
The specimens were then assigned at random to three different preparation designs, consisting of 15 specimens each. The division was made in such a way that there was a similar distribution of teeth (small, medium, large) and type (maxillary and mandibular) in each group.
Group 1- Specimens in group 1 were prepared with proximal grooves, occlusal rest seats, and lingual wings to receive conventional RBFPDs. (Figure 1).
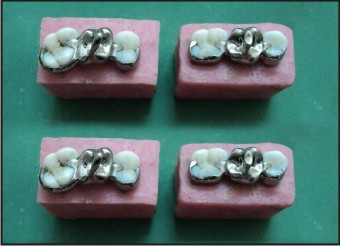 | Figure 1 : Group 1 Specimens
 |
Group 2- Specimens in group 2 were prepared with proximal slots, occlusal rest seats and lingual wings to receive modified RBFPDs. (Figure 2).
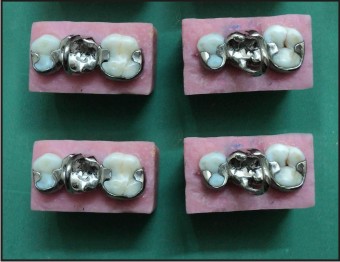 | Figure 2 : Group 2 Specimens
 |
Group 3- Specimens in group 3 were prepared with Class II inlay cavities to receive modified RBFPDs. (Figure 3).
 | Figure 3 : Group 3 Specimens
 |
Tooth preparation
Putty index was made using addition silicone impression material (3M ESPE, ExpressTM STD, vinyl polysiloxane impression material, Germany, Lot no. 153490) for each specimen before starting the preparation.
Group 1 specimens consisted ofproximal grooves, lingual wings and occlusal rest seats on the abutment teeth. The lingual reduction was done using micromotor handpiece attached to the Jelenko surveyor. The margins were placed 1mm above the cemento-enamel junction with a wing preparation of 0.6mm depth. The lingual reduction was extended further onto the other proximal surface to ensure a total circumferential coverage of more than 1800. The proximal grooves were placed in the center of the mesial surface of the premolar and in the center of the distal surface of the molar, 0.5mm above the finish line. Occlusal rest seats were prepared in the distal fossa of the premolar and in the mesial fossa of the molar. Occlusal rest seat was roughly rounded triangular in shape with apex towards the center of the occlusal surface. The depth of the rest seat was 1.5mm in the central fossa and 0.5mm at the marginal ridge with buccolingual width of 1/3rd the intercuspal distance and mesiodistal width 1/3rd the mesiodistal width of the concerned tooth.
Group 2 specimens consisted of proximal slots, lingual wings and occlusal rest seats on the abutment teeth. Occlusal rest seats were prepared in the mesial fossa of the premolar and the distal fossa of the molar. The preparation of occlusal rest and lingual wing preparation was done in the same way as it was done for specimens in group 1. The proximal slots, 3mm deep, 2mm wide bucco-lingually and 1.5mm wide mesio-distally, were prepared on the disto-occlusal surface of the premolar and the mesio-occlusal surface of the molar.
Group 3 specimensconsisted of class II inlay cavity on the distal side of the premolar and mesial side of the molar. Inlays were 2mm deep occlusally extending till the central fossa with an occlusal dovetail (0.5mm) and buccolingual width of 1/3rd the intercuspal distance; proximal box was made 3mm deep with straight parallel walls, beveled axio-pulpal line angle, flat pulpal and gingival floors.
Putty index was used to verify the amount of lingual reduction. William’s graduated periodontal probe was used to measure the depth, width and height of the proximal slots and class II inlay preparations. All the preparations were done by single set of burs for the particular group to standardize the preparations.
The putty wash impression technique was employed for making the impression of all the specimens using addition silicone- putty (3M ESPE, Express TM STD, vinyl polysiloxane impression material, Germany, Lot no. 153490) and light body (3M ESPE, vinyl polysiloxane impression material, Germany, Lot no. 128670) material. Impressions were poured using type IV die stone (Gyprock, Rajkot (Gujarat), India).
Wax patterns were fabricated using casting wax. A round sprue wax (Bilkim Polywax, Duron, Turkey) was shaped as a loop and attached to the center of the occlusal surface of the pontic buccolingually, parallel to the long axis of the tooth to allow tensile testing. Castings were made using Ni-Cr alloy, trimmed and polished.
Castings were cemented using self-adhesive resin cement (Smart cemTM2, Dentsply Caulk, USA, Lot no. 1105181). The specimens were then subjected to tensile pull out test using universal testing machine (Llyod LR 50K, FIE, India) after 24h of water storage (Figure 4). The force required to dislodge each RBFPD from teeth was recorded. The data were analyzed using one-way ANOVA and Bonferroni test.
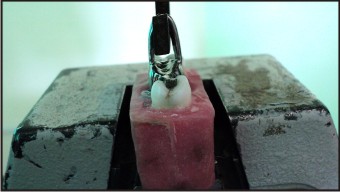 | Figure 4 : RBFPD Dislodged From The Mounted Specimen
 |
Results
Mean values and standard deviations were calculated for each group. The highest mean tensile bond strength was obtained for group 2 (382.30 N) and the lowest was obtained for group 1 (Figure 5). One way Analysis of Variance (ANOVA) was done using Statistical Package for Social Scientist (SPSS) at a level of significance of 0.05 and at a confidence interval of 95%. From the results of the analysis it was found that there was a highly significant difference between the three groups with respect to the mean load (F = 512.870, p < 0.01).
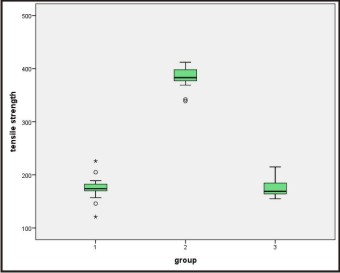 | Figure 5 : Box Plot Of Tensile Bond Strength
 |
In order to find out among which groups there exists a significant difference, multiple comparisons using Bonferroni test was done. (Table I) shows the pair wise comparisons of groups. There was significant difference in the mean load of group 1 when compared with group 2 (p < 0.01). However, the difference in mean load between groups 1 and 3 was not statistically significant (p > 0.05). There was statistically significant difference between the mean loads of group 2 when compared to both groups 1 and 3 (p < 0.01). The difference in mean load between group 3 & group 2 was found to be statistically significant (p < 0.01). No statistically significant difference was observed between groups 3 and 1 with respect to the mean load (p > 0.05).
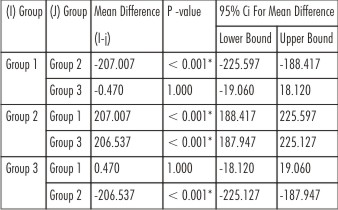 | Table I : Pair-wise Comparisons: Bonferroni Test
 |
Discussion
Teeth extracted for orthodontic treatment and periodontal treatment were chosen for the study as this would increase the chances of finding tooth with intact clinical crown and root. Human teeth were used for the study in an effort to simulate clinical conditions so that the results would be comparable and applicable in clinical situations.
An RBFPD is subjected to repeated tension, compression and torquing forces in the mouth. Until now, it has not been possible to simulate these forces in vitro. Although the tensile test does not directly reflect the intraoral dislodging forces, it does estimate the retentive properties of the RBFPDs. Hence, in the present study tensile force test was used as it is a widely accepted estimate for retention of RBFPDs.
In the present study, group 2 showed highest mean tensile bond strength and the difference was statistically significant as compared to the other two groups. The results were consistent with the study done by El-Mowafy O and Rubo MH.[10] They concluded that the addition of the slot cavities resulted in an increase in the preparation area, thereby increasing the surface area for bonding. Lankford and Christensen stated that modifications in teeth, such as grooves or slots, were required to provide adequate resistance form.[16] Eshelman JR et al stated that an increase in the resistance form can be obtained by incorporation of proximal slots which would interfere with the rotational movement of the prosthesis.[17] Crispin BJ from his longitudinal study concluded that the proximal segments act as connectors for the pontic and contribute to the buccolingual bracing of the abutments, while the lingual segments increase the surface area available for bonding and add to dissipation of laterally directed forces.[18]
Group 3 showed higher tensile bond strength than group 1 but the difference was not statistically significant. The results were consistent with the study done by Cotert SH and Ozturk B, where after 3 years follow up no significant difference in survival rate was found between the inlay design and the conventional design. They concluded that a layer of enamel should be retained on the pulpal walls and floor to maintain the enamel-resin-metal bond.[19] Isidor F and Stockholm R conducted a 4 year longitudinal study that used inlay preparation on abutments with twenty three RBFPDs reported no failures.[20]
Kiremitci A et al also found in their in vitro study that self-adhesive resin cement showed higher bond strength to enamel than dentin.[21] In this study group 3 preparation was in dentin so this might be a reason for less bond strength as compared to group 2.
Maximizing the contact area for bonding the retainer to the enamel is one of basic concepts, which can be achieved by extension of the preparation around 1800 of the axial surface.[22],[23],[24] As the group 3 preparations lacked this feature, this might be another reason for less retention as compared to group 2.
Visual inspection of the surface of the prostheses (71.33%) after dislodgement from the teeth showed that there were no remnants of the luting agent on their surfaces. This implies an adhesive failure at the interface between the cement and the prosthesis. 26.67% prostheses after dislodgement from the teeth showed that cement was retained on their surfaces, but there were areas free of cements, implying that the mode of failure was a combination of adhesive and cohesive failures. Only 2% of prostheses showed cohesive failure.
Most of the adhesive failures in this study occurred at the metal-cement interface indicating that this was the weakest link in the system. This observation was in agreement with the several clinical studies done by Hansson and Moberg[25], Rammelsberg et al[26], Boening[27], Hansson and Bergstrom.[28]
The extrapolation of the results from work of a purely in vitro nature must always be made with caution. In the oral environment, failure of RBFPDs takes place under conditions of repeated compressive and lateral forces of mastication, under the influence of thermal changes, and under changing pH of the salivary fluids, not under a continuous tensile load similar to that used in this study. This study assessed the tensile bond strengths of RBFPDs after 24 h of water storage. It is possible that a longer storage time and/or thermal cycling and cyclic (fatigue) loading would give different results.
Another crucial factor is the ability of an RBFPD to distribute stress under function. Hence a photoelastic stress analysis study may be useful in this regard.
Conclusion
Within the limitations of the study, the following conclusions were made:
1. The mean tensile bond strength of modified RBFPDs with proximal slots, occlusal rest seats and lingual wings was significantly higher than that of conventional RBFPDs and modified RBFPDs with class II inlays.
2. Modified RBFPDs with class II inlays had higher mean tensile bond strength than that of conventional RBFPDs, the difference was not statistically significant.
3. The tensile bond strengths were significantly affected by the surface area covered i.e., area available for bonding. Incorporation of slots, 1800 wraparound and occlusal rest seats increase the surface area thereby increasing the retention of the RBFPDs.
4. The positive findings of this study warrant a long term clinical trial of the modified RBFPDs.
References
1. Rochette AL. Attachment of a splint to enamel of lower anterior teeth. J Prosthet Dent 1973; 30:418-23.
2. Howe DF, Denehy GE. Anterior fixed partial dentures utilizing the acid-etch technique and a cast metal framework. J Prosthet Dent 1977; 37: 28-31.
3. Livaditis GJ. Cast metal resin bonded retainers for posterior teeth. J Am Dent Assoc 1980; 101:926-9.
4. Edelhoff D, Sorensen JA. Tooth structure removal associated with various preparation designs for posterior teeth. Int J Periodont Rest Dent 2002; 22: 241-9.
5. Aggstaller H, Edelhoff D, Rammelsberg P, Gernet W, Beuer F. Long-term clinical performance of resin-bonded fixed partial dentures with retentive preparation geometry in anterior and posterior areas. J Adhes Dent 2008; 10: 301-6.
6. Burgess JO, McCartney JG. Anterior retainer design for resin-bonded acid etched fixed partial dentures. J Prosthet Dent 1989; 61: 433-6.
7. El Mowafy O. Posterior resin-bonded fixed partial denture with a modified retentive design: a clinical report. J Prosthet Dent 1998; 80:9-11.
8. Botelho M. Resin-bonded prostheses: the current state of development. Quintessence Int 1999; 30:525-34.
9. Doh RM, Lee KW. Dislodgement resistance of modified resin bonded fixed partial denture utilizing tooth undercuts in vitro study. J Adv Prosthodont 2009; 1: 85-90.
10. El Mowafy O, Rubo MH. Retention of a posterior resin bonded fixed partial denture with a modified design: an in vitro study. Int J Prosthodont 2000; 13:425-31.
11. El Salam Shakal MA, Pieffer P, Hilgers RD. Effect of tooth preparation design on bond strengths of resin bonded prosthesis- a pilot study. J Prosthet Dent 1997; 77: 243-9.
12. Xie Q, Lassila LVJ, Vallittu PK. Comparison of load-bearing capacity of direct resin-bonded fiber-reinforced composite FPDs with four framework designs. J Dent 2007; 35:578-82.
13. Leevailoj C, Platt JA, Cochran MA, Moore BK. In vitro study of fracture incidence and compressive fracture load of all-ceramic crowns cemented with resin-modified glass ionomer and other luting agents. J Prosthet Dent 1998; 80: 699-707.
14. Michalakis KX, Stratos A, Hirayama H, Kang K, Touloumi F, Oishi Y. Fracture resistance of metal ceramic restorations with two different margin designs after exposure to masticatory simulation. J Prosthet Dent 2009; 102: 172-8.
15. Hannig C, Westphal C, Becker C, Attin T. Fracture resistance of endodontically treated maxillary premolars restored with CAD/CAM ceramic inlays. J Prosthet Dent 2005; 94: 342-9.
16. Lankford RJ, Christensen LC. Pin-retained, resin-bonded fixed partial dentures. J Prosthet Dent 1991; 65: 469-70.
17. Eshelman JR, Janus CE, Jones CR. Tooth preparation designs for resin bonded partial dentures related to enamel thickness. J Prosthet Dent 1988; 60: 18-22.
18. Crispin BJ. A longitudinal clinical study of bonded fixed partial dentures: the first 5 years. J Prosthet Dent 1991; 66: 336-42.
19. Creugers NHJ, De Kanter, Verzijden, Van’t Hof. Risk factors and multiple failures in posterior resin-bonded bridges in a 5-year multi-practice clinical trial. J Dent 1998; 26: 397-402.
20. Isidor F, Stokholm R. Resin-bonded prostheses for posterior teeth. J Prosthet Dent 1992; 68 (2):239-43.
21. Kiremitci A, Yalcin F, Gokalp S. Bonding to enamel and dentin using self-etching adhesive systems. Quintessence Int 2004; 35: 367-70.
22. Priest G. An 11 year reevaluation of resin bonded fixed partial dentures. Int J Periodont Rest Dent 1995; 15: 238-47.
23. Lin CL, Hsu KW, Wu CH. Multifactorial retainer design analysis of posterior resin bonded fixed partial dentures: a finite element study. J Dent 2005; 33:711-20.
24. Creugers NHJ, Kayser AF. An analysis of multiple failures of resin-bonded bridges. J Dent1992; 20: 348-51.
25. Hansson O, Moberg LE. Clinical Evaluation of Resin-Bonded Prostheses. Int J Prosthodont 1992; 5: 533-41.
26. Rammelsberg P, Pospiech P, Gernet W. Clinical factors affecting adhesive fixed partial dentures: a 6-year study. J Prosthet Dent 1993; 70: 300-7.
27. Boening KW. Clinical performance of resin-bonded fixed partial dentures. J Prosthet Dent 1996; 76: 39-44.
28. Hansson O, Bergstrom B. A longitudinal study of resin-bonded prostheses. J Prosthet Dent 1996; 76: 132-9.
|