Introduction
Health is defined as a state of physical, mental, social and emotional well being in which the body functions with comfort, confidence, creativity and contentment eventually leading an economically productive life. In essence, health is fundamental to human progress[1].
Pregnancy is a delicate condition involving complex physical and physiological changes.[2] Hormonal effects cause changes to almost every organ system, including the oral cavity. Prevention and health promotion interventions could enhance her own health or that of her infant. Gingival and periodontal changes during pregnancy have been well-documented[3] and research has shown that a great number of pregnant women do not undergo dental visits during the prenatal period and there is also high incidence of dental caries.[4]
Pregnancy and early childhood are particularly important times to access oral health care because the consequences of poor oral health can have .a lifelong impact.[4] Evidence suggests that most young children acquire caries-causing bacteria from mothers.[3] Cariogenic or decay-causing bacteria are typically transmitted from mother - or caregiver to child by behaviour that directly pass saliva, such as sharing a spoon when tasting baby food. The earlier those cariogenic bacteria occupy ecological niches in the child's mouth, the greater percentage of the child's plaque will contain these bacteria. Mothers who themselves have experienced extensive past or current caries have particularly a strong need for counseling on how .to avoid early transmission of cariogenic bacteria to their offspring.[4]
Pregnancy-related changes are most frequent and severe on gingival tissue.[5] Some of the periodontal conditions are considered specific to pregnancy, such as pregnancy gingivitis and epulis gravidarum.[6] Periodontal disease, including gingivitis and periodontitis, are infections that if left untreated, can lead to tooth loss.[7]
Pregnancy is a "teachable moment" when women are motivated to change behaviour. Untreated oral infection may become a systemic problem during pregnancy and may contribute to preterm and/or low birth weight deliveries.
Emerging science indicates that women with periodontal disease may be at the greater risk of delivering preterm, low birth weight babies. For this the American association of periodontology recommends that women who are pregnant or planning pregnancy should undergo periodontal examination.[8]
Reports have documented a high prevalence of gingivitis among pregnant women. Physiologic changes such as pregnancy alter women's body response to external stimuli. In the mouth, the greatest effect of pregnancy is seen in the gums. The higher concentration of oestrogen and progesterone during pregnancy especially in the presence of plaque have been implicated in the patho-physiology of pregnancy gingivitis.[9]
Though there is voluminous literature regarding the oral health status of pregnant women,[10] scanty data is available from Indian subcontinent and no study assessedthe influence of various socioeconomic factors on the oral hygiene status. Adler et al.[12] have described a model suggesting, that socio-economic position affects general health through health care, psycho-social factors and health related behaviors. In the present study we have also tried to find a relation of socio-economic status with DMFT scores in pregnant women.
The purpose of the study was 1) To evaluate the effect of socio economic status on DMFT scores of pregnant women. 2) To evaluate the DMFT of pregnant women with proper oral attitude. 3) To correlate socio-economic status and attitude with DMFI' of pregnant females in North India.
Methodology
The study included 238 pregnant females visiting the gynaecology out patient department of the M.M. College of medical sciences, Mullana, Ambala and surrounding primary health centers within a period of 6 months. Ethical clearance was taken for conducting the study. All the patients entered the study voluntarily, following an explanation of its purpose and objectives. A written consent was taken from each patient after explaining the purpose and objectives of the study.
Before the assessment of the oral health status, the patients were asked from a self-rectified questionnaire for the socio-economic and cultural background according to Kuppuswamy scale and demographic data which included the subject's age, month of pregnancy, order of pregnancy, qualification, occupation, status and locality they reside in. Patients were also asked about the frequency of their dental appointments.
After inquiring about the socio cultural status of the subject, oral hygiene of the patient was assessed by asking the subjects about their oral hygiene practices which included habit of brushing, rinsing after meals, duration and frequency of brushing, type of brush used, method used for brushing, use of toothpaste and brush or not, visit to a dentist and regular dental checkups.
After acquiring all the information, the subject was examined for the oral health status by determining the DMFT score, according to WHO oral health assessment form (2004). All the Patients were examined by a well trained observer accounting for the DMFT of the individual.
KUPPUSWAMY'S SOCIO-ECONOMIC STATUS SCALE was used for the socio economic assessment of the subjects in consideration. The professional categories for education were defined as 1) Illiterate 2) Primary school certificate 3) Middle school certificate 4) High school. certificate 5) Post high school diploma 6) Graduate 7) Post graduate
On the basis of occupation 1) unemployed 2)Un-skilled worker 3) Semi skilled worker 4) Skilled worker 5) Clerical, Shop owner, Farmer 6) Semi – Professional 7) Professional.
On the basis of family income scale is classified as 1) less than Rs.1093 2) 1093- 3248 3) 3249- 5414 4) 5415- 8121 6) 8122- 10829 10) 10830 – 21659 12) more than Rs. 21660.
Oral Health Assessment
All the patients were examined by a previously trained observer. Number and type of teeth were recorded. The DMFT score of each patient was assessed to check the oral health status of the patient using WHO oral health assessment form (2004). DMFT was assessed as 0- sound, 1- decayed, 2- filled and decayed, 3- filled without decay, 4- missing due to caries, 5- missing for any reason other than caries, 6- sealent or varnish, 7- bridge abutment, 8- unerupted tooth, 9- excluded tooth, T-trauma or fracture.
The data was transferred to the computer, corrected for logical errors. The statistical analysis was performed using the Statistical Program for Social Sciences (SPSS 11.0 for Windows), using Kruskal Wallis test and Fisher’s Exact test.
Results & Analysis
Table 1 Shows demographic distribution of the population including 238 pregnant females between the ages of 18 to 30 years. Most of the subjects were under the age of 25 years (63.9%). More than half were conceiving for the first time (60.9%).
A total of 238 pregnant women were considered in the study. Mean age of the subjects were 23.97.
63.9% of the subjects were among the age group of 21 – 25yrs.
Table 2: As the data for DMFT is non parametric KRUSKAL WALLIS test was applied to compare the mean DMFT values with 3 socioeconomic groups ie; upper, middle and lower 73.5% of the subjects were residing in rural areas & 26.5% were residing in urban areas, as is reflected in Table no. 2 . Lower half of table 2 shows distribution of study subjects according to socioeconomic status and locality. More than half of the subjects were from lower middle class ie; 62.2%. However lower upper class were 39 ie; 16.4% And upper middle class were represented by 48 pregnant females ie; 20.2% And only 3 subjects ie; 12% were from upper class.
Table 3. a) and b) Comparison of mean DMFT between different socio-economic classes using Kruskal wallis test and post hoc analysis:
Shows comparison of mean dmft between different socioeconomic classes using kruskal wallis test and post hoc analysis.
In Table 3(a) p value less than 0.05 shows some significant difference in the DMFT between three socioeconomic classes there.
Table 3(b) shows significant difference between lower class and middle class as mean values are 3.62 and 2.72
However, there is no significant difference between upper and middle class as mean values in these two classes are 2.72 and 1.67 saying that DMFT of these two classes is almost same.
Similarly in lower and upper class, mean DMFT was 1.67 and 3.63. Thus the difference is insignificant.
Table no. 4. Association of oral hygiene aids and socio-economic status *p value < 0.05
Table 4 Shows that there was not much difference between lower, middle and upper class as regards the habit of mouth rinsing after snacking.
Secondly, there was no significant difference between the material used for cleaning by various groups ie; whether datun or tooth brush, neither was there any difference between the frequency of tooth brushing and time in changing the tooth brush.
However, method of tooth brushing was significantly different between 3 socioeconomic groups.
Rest all other oral hygiene habits were almost similar.
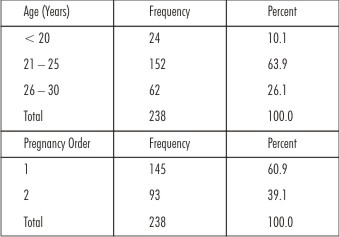 | Table.1. Demographic Description Of The Study Population (N = 238)
 |
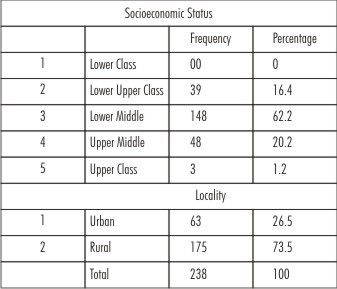 | Table 2. Shows Distribution Of Study Subjects According To Socio-economic Status And Locality
 |
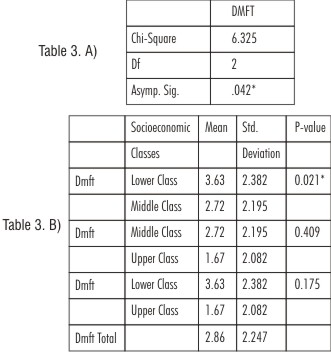 | Table 3. A) And B) Comparison Of Mean Dmft Between Different Socio-economic Classes Using Kruskal Wallis Test And Post Hoc Analysis
 |
 | Table 4. Association Of Oral Hygiene Aids And Socio-economic Status *p Value < 0.05
 |
Discussion
Pregnancy involves complex changes in the body. Every system in even healthy women is altered to some degree during pregnancy including saliva and oral cavity. The monitoring and care of oral cavities in pregnant women are amongst important public oral health activities in India, as healthy oral cavity in pregnancies is directly related to a decrease in DMFT and leads to improvement inchild oral health indicators and in quality of life for women.
A number of features inherent in this study deserve some clarification for convenience; although the present study aimed to estimate the oral hygiene of pregnant females in North India & to explore the association of various sociodemographic factors on oral hygiene status of pregnant women, the study was conducted in a limited area and socio-demographic data collected was based on subjective information. It is recognized that the external validity of this study is limited, and therefore, the results cannot be generalized to all of the pregnant women, which is one of the limitations of the study.
The results of the present study support earlier reports, confirming that DMFT is increased in pregnant females.[11],[12] Al–Nuaimy K et al conducted a study on 200 females to assess Decayed, Missing and Filled Teeth Index (DMFTI) among other parameters during pregnancy. The result of this study during pregnancy showed increased DMFT Index as compared with the controls.[11] Results of our study also showed that DMFT index is high in pregnant females.
Majority of the pregnant females were under 25 years of age. Results of study revealed that pregnant women in younger age group i.e. up to 25 years had good oral hygiene practices as compared to women in comparatively older age group i.e. 26 years to 30 years. The implication of this observation is that the women who are pregnant in older age groups need to be observedmore diligently and their oral health practices are required to be improved. This is possible witha concerted effort on the part of oral healthpractitioners to educate these women about oral health to improve the quality of their life and oral health of their offspring.
Educated women possess a better oral hygiene as compared to illiterate women as they are more concerned about their oral health. Oral health education to all pregnantwomen should be mandatory at the health centres.
Wandera M[12] in a study on socio demographic factors related to periodontal diseases and tooth loss of pregnant females concluded that rural, nulliparous and those who never visited a dentist were less likely, whereas women from larger households were more likely, to have lost at least one tooth. Similar results were found in our study where DMFT score was more in urban pregnant females as compared to pregnant females from rural areas.
Acharya S[13] conducted a study on pregnant females and concluded that those women with previous history of pregnancies had more severe levels of gingivitis than those who were pregnant for the first time. Machua G[6] in their study also showed that women in 2nd and 3rd trimester reported some inflammatory changes evident during these stages of pregnancy. Several hormonal factors have been associated with these periodontal changes, particularly rising serum progesterone levels.[15] Similar to the periodontal changes, in our study, the DMFT score was more pronounced in 3rd and 2nd trimester of pregnancy as compared to 1st trimester.
The data from the study can have some implications on the oral health of the offspring these pregnant women will deliver. As the previous studies[16] have shown that oral health of the mother is indicative of the oral health of the offspring, the data from this study can also be correlated with the oral health of the children of these women & measures can be taken for prevention of oral diseases. Various studies documented that oral health care of pregnant women as an "early preventive strategy” for her child’s oral health which may improve the oral & systemic health of children. Dentistry can be vital in improving prenatal outcome and maternal or fetal dental health through screening, referral and education of pregnant women. These methods can be applied on a larger scale in the community for the better oral health of the mothers and children.
Conclusion
According to the results obtained, it can be concluded that the pregnant women evaluated in this study had unfavorable oral health as regards DMFT, and there was significant difference between the impact of socioeconomic status on DMFT of study samples. Significant difference was seen in the method of tooth brushing amongst three socioeconomic classes and DMFT was higher in lower socio- economic classes as compared to upper and middle class.
References
1. Agarwal A, Gupta D K, Bhatia P- Oral Health –As A Prodrome Of Systemic Diseases. Indian Journal Of Dental Sciences.
2. Gajendra S, Kumar J V—Oral Health And Pregnancy: A Review. Nysdj January 2004.
3. Loe H, Silness J. Periodontal Disease In Pregnancy. I. Prevalence And Severity. Acta Odontologica Scandinavia 1963; 21 : 533-51.
4. Sunali Khannal, Malhotra Shalini2--- Pregnancy And Oral Health : Forgotten Territory Revisited J Obstet Gynecol India Vol. 60, No. 2 : March / April 2010 Pg 123-127.
5. Laine Ma. Effect Of Pregnancy On Periodontal And Dental Health. Acta Odontol Scand 60 (2002).
6. Machuca G. The Influence Of General Health Socio Cultural Variables On The Periodontal Health Of Pregnant Women. J Periodontal July 1999.
7. Alwaeli Ha, Al-Jundi Sh. Periodontal Disease Awareness Among Pregnant Women And Its Relationship With Socio- Demographic Variables. Int J Dent Hygiene 3, 2005; 74¬82.8. 8.American Academy Of Periodontology Statement Regarding Periodontal Management Of Pregnant Patient.. J Periodontol. March 2004.
9. Ifesanya Ju, Ifesanya Ao. Determinants Of Good Oral Hygiene Among Pregnant Women In Ibadan, South-Western Nigeria. Annals Of Ibadan Postgraduate Medicine. Vol. 8 No. 2 December, 2010.
10. Taani Dq, Habashneh R. The Periodontal Status Of Pregnant Women And Its Relationship With Socio-Demographic And Clinical Variables. Journal Of Oral Rehabilitation 2003 30; 440 445.
11. Al–Nuaimy K, Al–Doski F. Pregnancy–Related Changes In Oral Health And Human Unstimulated Whole Saliva. Al–Rafidain Dent J Vol. 3, No. 2, 2003
12. Wandera M, Engebretsen Im. Socio-Demographic Factors Related To Periodontal Status And Tooth Loss Of Pregnant Women In Mbale District, Uganda . Bmc Oral Health 2009, 9:18 Doi:10.4186/1472-6831-9-18.
13. Acharya S, Bhat Pv. Factors Affecting Oral Health-Related Quality Of Life Among Pregnant Women. Int J Dent Hygiene 7, 2009; 102-107.
14. Amar S, Chung Km. Influence Of Hormonal Variation On The Periodontium In Women. Periodontal 2000 1994;6;:79-87.
15. Sooriyamoorthy M, Gower Db. Hormonal Influence Of Gingival Tissue: Relationship To Periodontal Disease. J Clin Periodontol 1989;16:201-208.
16. Boggess KA. Maternal Oral Health in Pregnancy. OBSTETRICS & GYNECOLOGY VOL. 111, NO. 4, APRIL 2008
|