Introduction
AI is an incompletely understood group of hereditary developmental defects of dental hard tissues particularly enamel. It has a variety of clinical forms and differing patterns of hereditary transmission. The condition is a social hindrance to the patient and treating such individuals brings drastic transformation in their psychosocial behaviour and approach towards life. Aesthetic problems often have to be addressed early in life when cooperation is difficult. The dentist has to balance the decision for early intervention and long term survival of restoration of lost function[1],[2]. This article reviews literature about AI with main focus on the different treatment means.
Background
Amelogenesis Imperfecta is a group of hereditary disorders characterized by alteration of quantity and quality of enamel in humans and is frequently associated with a significant dental disease[3]. The term, AI was introduced by Weinmann and co-workers. It has an incidence of 1:14000 (Witkop and Sauk). Heredity is an important factor in the aetiology of AI[4]. The most widely accepted classification[5] given by Witkop and Sauk;
• Type I- Hypo-plastic pattern
• Type II- Hypo-maturation pattern
• Type III- Hypo-calcified pattern
• Type IV- This variety of AI exhibits enamel hypoplasia combined with hypomaturation and is seen in the systemic disorder, tricho-dento-osseous syndrome.
AI has been reported to be associated with other dental conditions such as Taurodontism, pulpal calcifications, multiple tooth impactions, oligodontia, hyper-cementosis, distorted roots, aberrant dentin formation and marked follicular hyperplasia and malocclusion[5],[6],[7],[8]. Tranchade NI and others[9] documented co-existence of AI and Nephrocalcinosis syndrome.
Treatment Aspects
The main problems with AI are loss of aesthetics, dental sensitivity, loss of vertical dimension of occlusion and function. In addition there is prevalence of caries, anterior open bite, delayed eruption, tooth impaction and/or gingival inflammation as secondary factors. Most patients approach dentists for improvement of aesthetics or treatment of sensitivity and gingival bleeding or with pain due to pulpal exposure caused by rapid enamel wear.
Role Of Dental Radiographs
Collins and others described[10] radiographic densities of different types of AI; density was most variable in hypo-plastic type, whereas the hypo-calcified had lowest mean enamel density due to substantially reduced mineral content. In hypo-maturation variety, the autosomal recessive had decreased mineral content. Understanding the degree of enamel mineralisation is critical while trying to decide whether there is adequate mineral for bonding or tooth must be crowned.
Phases And Principles Of Treatment
Active dental intervention in a complex AI case may span several decades, involving participation of various dental specialities[6]. The age related treatment approach involves;
• Temporary or Initial phase (primary dentition 2-6 yrs)
• Transitional phase (early mixed dentition 6-11yrs)
• Final permanent phase (mixed to permanent dentition)
Desort KD[6] said in the initial phase, oral hygiene instructions are enforced and a‘wait and see’ attitude is adopted to assess the degree of enamel derangement.
Bedi R[11] discussed principles of treatment while managing children with AI;
1. Pain relief
2. Motivation of child and parent
3. Introduction to dental procedures
4. Maintenance of occlusion
5. Aesthetics
Bouvier D and co-workers reported[12] a case of a ten year old girl in whom they performed intial treatment for anteriors. This resulted in a spectacular psychological transformation and motivated the patient for further treatment. Mackie IC and Blinkhorn AS presented[13] a case report of an 8 year old boy with AI . They used a combination of prompt clinical action and preventive care and stressed importance on prevention of caries and gingivitis, improvement of aesthetics and lastly prevention of wear of permanent teeth using crowns.
Allowing the maxillary and mandibular growth
Bouvier D and co-workers[14] presented the sequence of a 2 phase treatment in a 7 year old boy. The temporary phase lasted more than 3.5 years. Preformed Nickle-Chromium crowns were fitted on the first permanent molars and second deciduous molars to halt attrition and stabilise occlusion. Maxillary and mandibular incisors were restored with carboxylate crowns. Upon eruption premolars and canines were restored with carboxylate crowns. Upon eruption, second molars were given Nickle-Chromium crowns. Third molar tooth germs were removed and 2mm bite was raised. In the next phase, permanent restorations were given. Planas in 1992 said that, In treating AI in children, it is important to allow for maxillary and mandibular growth by using individual restorations on teeth.
Hunter and Stone[15] used adhesive cast Cobalt-Chromium onlays in supra-occlusion as an alternative to preformed crowns. Cobalt-chromium could be cast accurately to 0.3mm and this could be used before teeth are fully erupted and tooth preparation in unnecessary.
Improving quality of life with a team approach
Treatment of AI involves a multidisciplinary approach, that includes initial extractions followed by assessment of periodontal tissues and performing the necessary treatment. Most AI patients present poor gingival health. The periodontal procedures may range from simple scaling and oral hygiene maintenance to surgical modes. Storie and co performed[16] osseous surgery to provide cervical margins on sound tooth structure that improved the crown height required for retention of the crowns.
Williams WP and co-workers[17] used combination of periodontic and prosthodontic treatment to treat a 16 year old girl. The patient was apprehensive and refused orthodontic treatment. Other factors included short clinical crowns, less enamel and large pulp. Periodontal full flap surgeries were done to increase the crown height followed by full coverage restorations.
Treating a patient in the peer age group is most challenging, as in those individuals personality traits are still in the stages of development. The growth and development stage as well as the patient’s economic status have to be considered. The dentist must balance the many treatment alternatives with goals of the patient in order to arrive at a reasonable and suitable plan of action. One needs to evaluate the order of different speciality procedures to be carried out. It would be plausible to initially perform full bonded orthodontics for alignment of dentition followed by restorations. The next dilemma would be about how appropriately the teeth can be restored. A limited temporary-permanent treatment would serve during temporary and transitional growth phases. Teeth can be protected using temporary restorations that can later be replaced by permanent restorations.
Encinas RP and others[18] discussed a case of AI with congenitally missing teeth, openbite and bilateral posterior crossbite. Endodontic treatment of first four molars was done. As patient refused surgery an orthodontic camoflouge was adopted. A pre-adjusted bracket appliance with quad-helix was used to correct occlusal problems. After 4 months retention, crown lengthening was done followed by ceramo-metal restorations on all teeth.
Keles A and others reported[19] a case of AI with class III skeletal pattern, asymmetry, high angle and severe anterior open bite. An interdisciplinary treatment encompassing orthodontics, orthognathic surgery and prosthodontics was done. Pre-surgical orthodontics included rapid palatal expansion and fixed appliance therapy. The surgical part involved maxillary posterior impaction with anterior advancement and mandibular setback using vertical chin reduction and genioplasty. The final restorations consisted of anterior ceramic veneers and posterior full ceramic crowns.
Final Treatment Phase
The final treatment is started in the late mixed dentition and carried into the permanent dentition stage. The goals of treatment involve; 1.Maintenance of arch dimensions, 2.Final restoration and maintenance of occlusion and function, 3.Restoration of aesthetics
Maintenance of arch dimensions starts from the initial stages of treatment and is carried on till the final phase. Temporary crowns have be used for this purpose in past[14],[15]. Arch dimensions can also be achieved by a combination of Myofunctional therapy, interceptive orthodontics and cephalometric measurement during orthognathic surgery as described by some authors[18],[19],[20]. Once arch dimensions are established, occlusion, contacts and function are restored. As final restoration, full crowns on teeth provide predictable, durable and aesthetic results. Full Ceramo-metal, ceramic and Full metal crowns have been used in the past[13],[14],[15],[16].
Aesthetics
Cosmetic rehabilitation of AI ranges from simple bleaching, veneering to full crowns, considering the amount of available tooth structure, radio-density of enamel, economic condition and aesthetic demands of the patient.
Wong SL and Winter GB reported[21] use of micro-abrasion with an abrasive paste and 18% hydrochloric acid followed by application of sodium fluoride to restore fluoride rich layer. Soares CJ and others[22] used acid etching with directly applied restoration using hybrid and micro-filled composites along with a contemporary enmel/dentin adhesive system. Rada and Hasiakos[23] used direct facial composite veneer restorations with glass-ionomer cement and dentinal priming agents. Venezie DD[24] and others presented a novel approach for bonding an orthodontic bracket to a tooth affected by AI by pre-treating it for 1 minute with 5% sodium hypochlorite. Sodium hypochlorite is an excellent protein denaturant capable of removing excess enamel protein in Hypocalcified AI. Use of ceramic veneers increased from the time of their introduction. They are a good choice for anteriors when full coverage is not necessary[22].
Seyman and Kiziltan[25] discussed use of overdenture prosthesis for occlusal and esthetic rehabilitation of a four year old patient diagnosed with autosomal dominant hypocalcified AI.
Conclusion
The entire rehabilitation of a patient suffering from AI encompasses the collaborated effort of different disciplines of dentistry. The purpose of such an effort is to provide a pain-free, aesthetic and efficient masticatory apparatus and should enable the patient to lead a normal life without any physical, emotional and social disturbances.
Photographs - Legends
Fig 1 Focal Hypoplastic AI
Fig 2 Pitted Hypoplastic pattern associated with open bite
Fig 3 Hypomineralisation variety presenting severe attrition
Fig 4 Hpocalcification type associated with poor gingival health and gingival hyperplasia
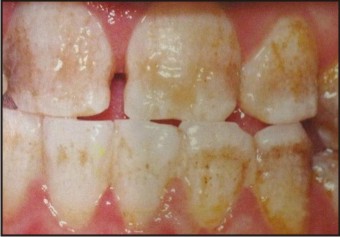 | Fig 1. Focal Hypoplastic Ai
 |
 | Fig 2. Pitted Hypoplastic Pattern Associated With Open Bite
 |
 | Fig 3. Hypomineralisation Variety Presenting Severe Attrition
 |
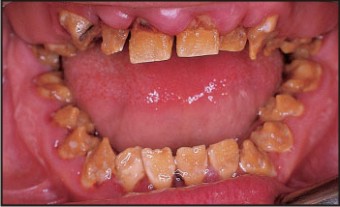 | Fig 4. Hpocalcification Type Associated With Poor Gingival Health And Gingival Hyperplasia
 |
References
1. Navarro LF, Garcia AA, Marco JB, Llena-Puy C. A study of the clinical, histopathologic and ultrstructural aspects of enamel agenesis: Report of case. Journal of Dentistry for children 1999;30:208-12.
2. Light EI, Rakow B, Fraze RL. An esthetic transitional treatment for AI: report of two cases. JADA 1975;90:166-70.
3. Tandon S. Text book of pedodontics. 1st Edition India Paras Company; 2003 pp 102.
4. Kida M, Ariga T, Shirakawa T, Oguchi H, Sakiyama Y. Autosomal-dominant hypoplastic form of AI caused by an enamelin gene mutation at the Exon-Intron boundary. J Dent Res 2002;81:738-42.
5. Witkop CJ Jr.. AI, dentinogenesis imperfecta and dentin dysplasia revisited: problems in classification. J Oral Pathol 1989;17:547-53.
6. Desort KD. AI: the genetics, classification and treatment. J Prosthet Dent 1983;49:786-92.
7. Lykogeorgos T, Duncan K, Crawford PJM, Aldrrd MJ. Unusual manifestations in X-linked AI. Int J Paediatr Dent 2003;13:356-61.
8. Fritz GW. AI and multiple impactions. Oral Surg Oral Med Oral Pathol. 1981;51:459-60.
9. Tranchade IN, Bonarek H, Marteau JM, Boileau MJ, Nancy J. AI and nephrocalcinosis: a new case of this rare syndrome. J Clin Paediatr Dent 2002;27:171-76.
10. Collins MA, Mauriello SM, Tyndall DA, Wright JT. Dental anomalies associated with amelogenesis imperfecta. Oral Surg Oral Med Oral Pathol Oral Radiol Endod 1999;88:358-364.
11. Bedi R. The management of children with AI. Restorative dentistry 1989;30:28-34.
12. Bouvier D, Duprez JP, Bois D. Rehabilitation of young patients with AI: A report of two cases. Journal of Dentistry for children 1996;63:443-47.
13. Mackie IC, Blinkhorn AS. AI: Early interception to prevent attrition. Dent Update 1991;18:79-80.
14. Bouvier D, Duprez JP, Pirel C, Vincent B. AI- prosthetic rehabilitation: A clinical report. J Prosthet Dent 1999;82:130-31.
15. Hunter L, Stone D. Supraoccluding cobalt-chrome onlays in the management of AI in children: A 2-year case report. Quintessence Int 1997;28:15-17.
16. Storie DQ, Cheatham JL. Management of AI by periodontal and prosthetic therapy. J Prosthet Dent 1970;24:608-
17. Williams WP, Becker LH. AI: functional and esthetic restoration of a severly compromised dentition. Quintessence Int 2000;31:397-403.
18. Ecinas RP, Espona IG, Mondelo JMNR. AI: Diagnosis and resolution of a case with hypoplasianand hypocalcification of enamel, dental agenesis and skeletal openbite. Quintessence Int 2001;32:183-89.
19. Keles A, Pamukcu B, Isik F, Gemalmaz D, Guzel MZ. Improving quality of life with a team approach. Int J Orthod Orthognath Surg 2001;16:293-99.
20. Gemalmaz D, Isik F, Keles A, Kurer D. Use of adhesively inserted full ceramic restorations in the conservative treatment of AI: A case report. J Adhes Dent 2003;5:235-42.
21. Wong SL, Winter GB. Use of microabrasion to improve dental aesthetics. Br Dent J 2002;193:155-58.
22. Soares CJ, Fonseca RB, Martin LRM, Giannini M. Esthetic rehabilitation of anterior teeth affected by enamel hypoplasia: a case report. J Esthet Restor Dent 2001;14:340-48.
23. Rada RE, Hasiakos PS. Current treatment modalities in the conservative restoration of AI: a case report. Quintessence Int 1990;21:937-42.
24. Venezie DD, Vadiakas G, Christensen R, Wright JT. Enamel pre-treatment with sodium hypochlorite to enhance bonding in hypocalcified AI: case report and SEM analysis. Paediatr Dent 1994;16:433-36.
25. Seymen F, Kiziltan B. AI: a scanning electron microscope and histopathologic study. J Clin Paediatr Dent 2002;26:327-36.
|