Introduction
If the luxation be left unreduced the patient will remain a living memorial of the surgeon's ignorance or inattention-Sir Astley Cooper[1]
Temporomandibular joint(TMJ) dislocation is defined as an excessive forward movement of the condyle beyond the articular eminence with complete separation of the articular surfaces and fixation in that position.[2],[3]
Dislocation is the complete separation of the articular surfaces with fixation in an abnormal position.The facial profile changes while the ligaments around the joint often stretch with intra-articular effusion, causing severe discomfort and difficulty with speech and mastication from muscle spasms and joint pain.[4],[5]
While subluxation or habitual luxation refers to excessive abnormal excursion of the condyle secondary to flaccidity and laxity of the joint capsule, recurrent dislocation is characterized by a condyle that slides over the articular eminence, catches briefly beyond the eminence and then returns to the fossa.[6],[7]
Dislocation of the temporomandibular (TMJ) represents 3% of all reported joint dislocations. Acute dislocation is not a cause of concern to the surgeon, as almost always this can be reduced by manual reduction under local anaesthesia or sedation.[8]
There is significant literature relating to the surgical treatment options of TMJ dislocation , considering one or the other type of treatment without comparison of treatment option.
The aim of this article is to review, analyze , summarize the management options and the changing trends available for the different types of TMJ dislocation reported in the literature in last decades.
Methods and Materials
A thorough digital search in literature was performed using the Pubmed search. Key words temporomandibular joint dislocation was used for the search. The reference list of the reviewed articles was also searched from medline and google scholar search engines for cited and related literature . Case reports/series, and original articles that documented the type of dislocation, number of cases treated in the series and original articles were taken into account.
Results
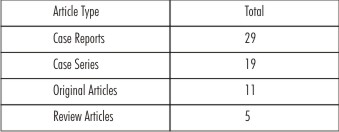
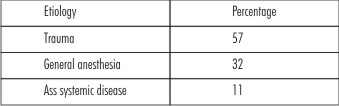
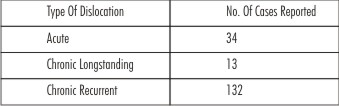
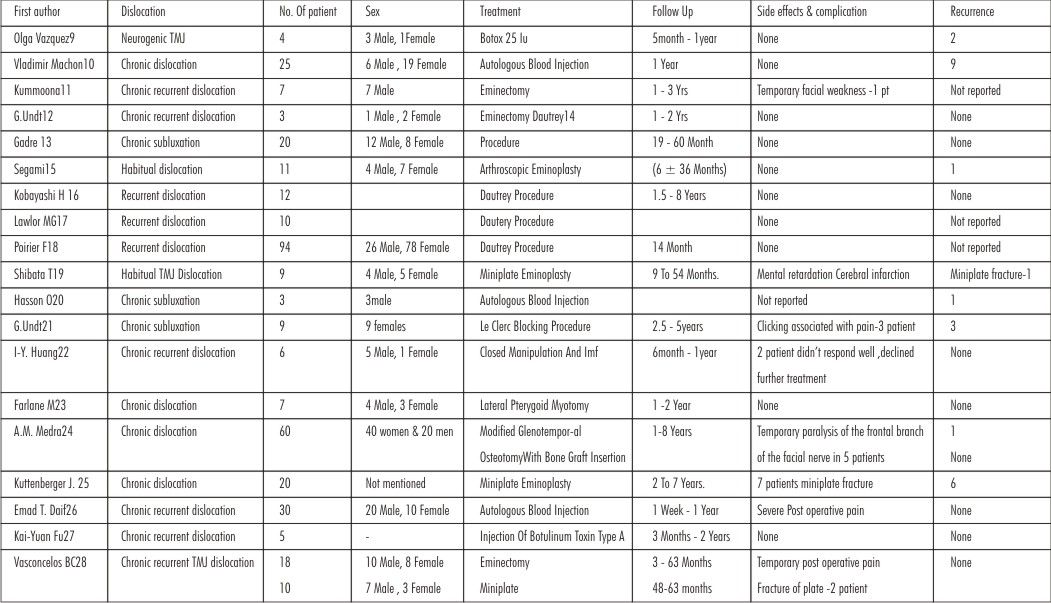
A total of 163 articles were reviewed out which 64 were found relevant. Of these, 29 were case reports, 19 were case series and 11 were original articles and 5 review articles. 34 cases were acute, 13 cases were chronic longstanding and 132 cases were chronic recurrent TMJ dislocations (Table 1). Etiology was predominantly trauma in 57% of cases ,other causes like excessive mouth opening from yawning, laughing, singing, prolonged mouth opening dental procedures, forceful mouth opening under the general anaesthetic procedure like laryngeal mask airway insertions in 32% cases and 11 % accounted for those under effect of medications secondary to systemic diseases (Table 2).
 |
 |
 |
 |
 |
 |
 |
 |
 |
 |
 |
 |
Discussion With Review Of Various Treatment Modalities:
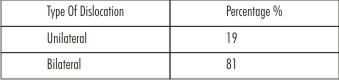
Dislocation can be partial (subluxation) or complete (luxation), bilateral or unilateral[28],[29],[30], Acute, chronic long standing, chronic recurrent. Also, it can be anterior-medial, superior, medial, lateral or posterior dislocation and the cause is either spontaneous or induced by trauma[31],[32],[33],[34],[35],[36],[37] forceful mouth opening from endotracheal intubation with laryngeal mask or tracheal tube, dental procedures, endoscopy[38], [39], [40], [41], [42], [43], [44], [45], [46], [47], [48], excessive mouth opening from yawning[49],[50] laughing, vomiting[51] and also during seizures from the effect of major tranquilizers / neuroleptics[52],[53] used for neuro-psychiatric diseases or secondary to systemic diseases like Marfans syndrome , Ehlers danlos syndrome.[54]
Diagnosis:
Diagnosis of temporomandibular joint dislocation is based purely on clinical findings and clinical history which can be aided by the radiographic findings. The patients commonly present with a chief complaint of inability to close the mouth/mastication, severe pain, deviation of chin, unilateral occlusion.[55],[56]
As described by Sir Astley Cooper(1837)[1] “the appearance is just that of a person when yawning. There is a depression just before the meatus auditorius, from the absence of the condyloid process from its cavity, and there is a projection of the cheeks, from the coronoid processes being advanced towards the buccinators”.
In case of chronic & long standing dislocation, patient would present with any of the signs mentioned above but with more frequency of dislocation. The patient do not present with severe pain, which is in contrast with that of acute dislocation. It generally results from the undiagnosed or inadequately reduced acute dislocation cases. TMJ hypermobility is noted only when it interferes with smooth mandibular movements. Hypermobility was found to be present in 70% of population ,may predispose to dislocation and subluxation.[57],[58]
Boering et al found incidence of subluxation as 1.8% in population of 400 patients with symptomatic TMJ disorders.
Treatment Perspectives
Typically, the management of TMJ dislocation depends on whether it presents as an acute, chronic or recurrent condition, accordingly all the available treatment options given in the literature have been categorized as conservative or surgical.
The choice of treatment ranges from simple closed reduction, intraoral splint and traction to a complicated osteotomies with bone grafts.
The term acute refers to untreated dislocation upto 72 hrs from the time since it got dislocated.
Recurrence in dislocation is been used synonymously with chronic in literature[58]. Dislocated joint left untreated for days to years is referred as long standing. In terms of position the antero- superior dislocation of the temporomandibular joint is reported most commonly in the literature.
Posterior dislocations typically occur secondary to a direct blow to the chin. The mandibular condyle is pushed posteriorly toward the mastoid .Injury to the external auditory canal from the condylar head may occur from this type of injury.[58],[59]
The term anterosuperiorly and superolaterally are used interchangeably in the literature and in agreement with Worthington[60],the correct nomenclature should be anterosuperior dislocation as the condyles were placed anterior to the fossa and superiorly into the temporal fossa.[10]
Prophylactic Methods
Prolonged rest for TMJ for atleast 1-2 months aided by painkillers and soft diet for the joint to overcome the stress it has suffered during dislocation episode.
Conservative Methods
Hippocrates in 5th century B.C first described mandibular dislocation and its treatment, his method of reducing a dislocated temporomandibular joint has survived ages and is still universally accepted.[61]
In case the hippocrates traditional method of manual reduction fails , the wrist pivot method which is slight modification of the original one as suggested by Lowery et al has been quite effective.[62]
Appliance therapy has also been used with fulcrum in the molar region and extra oral extension for elastic traction in case the traditional methods tends to fail to relocate condyle in normal anatomical position as suggested by Adekeye et al[63]
Treatment with botulinum toxin offers the option of minimal invasive therapy under outpatient conditions. Toxin prevents the release of acetylcholine at neuronal synapses. The resulting neuromuscular blockade causes paralysis of skeletal musculature and smooth muscles supplied by the parasympathetic system. Potential contraindications for treatment with botulinum toxin include neurological conditions affecting the motor endplate such as myasthenia gravis or Eaton- Lambert syndrome. Due to passage across the placenta, the use during pregnancy is also contraindicated.[64],[65],[66]
Surgical Procedures:
These can be broadly classified into basic principles of A) Anti translatory procedures B) Obstructing C) Obstruction clearance D) Reduction of muscular forces Anti translatory procedures basically refers to the prevention of the forward translatory movement of the condyle which included capsular plication, capsullorraphy, anchoring of the coronoid process to zygoma,these treatments are of out of date with better promising techniques now replacing them.[58]
Obstructing procedures included soft tissue and bony procedures to cause hindrance to abnormal movements from its normal path. Soft tissue procedures included Konjetzny[67] method of surgically creating a closed lock and others followed were by bony procedures included one devised by Dautrey[14] and later modified by Le Clerc[68] in which the zygomatic arch was cut vertically in front and lowered aiding in resistance to the forwardly gliding of the condyle, a procedure still followed universally.
Obstruction clearance procedures had been devised to remove the obstacle`s in the condylar paths that may evoke the dislocation of condyle 1) Discectomy using interpositional adipose tissue. 2) Eminectomy - popularized by Myrhaug,[69] which is still one of most accepted modality or chronic recurrent dislocation.
Eminectomy though widely being used these days it does not address the uncoordinated muscle activity and the lax capsule or ligament, and this had made some surgeons to adopt a modified mini-invasive eminectomy and relocation of the lateral pterygoid muscle or redirection of the temporalis muscle which aims to act on both the obstacle and the cause with respect to restoration of TMJ biomechanical constraints .However, about 95% success rate have been recorded after eminectomy and use of metallic implants on the articular eminence.[70],[71],[72]
Combined procedure eliminating the blocking and limiting translation procedures included a)Lateral pterygoid myotomy b) Condylotomy c)Condylectomy procedures.
Release of the lateral pterygoid muscles will directly alter the musculature.[73] This procedure involves excision of the insertion of the lateral pterygoid muscle at the condylar neck and joint capsule. The operation attempts to disable the lateral pterygoid muscles, allowing only rotational movement of the condyle.
When temporalis muscle is short and contracted in nature, Laskin had proposed an intraoral surgical approach to the muscle via a coronoid incision to do a temporalis myotomy[74],[75],[76]. Where access is difficult, when there is fibrosis or adhesions of muscle and cases where reunion of the muscles may occur, coronoidotomy with or without condylotomy[77],[78] is advocated
Gotlieb advocated condylectomy and coronoidectomy procedures in cases where there is ankylosis but there is possibility of entering the base of the skull and excessive bleeding from pterygoid plexus, internal maxillary and middle meningeal vessels.[79]
Shorey and Campbell et al[80] , classified the treatment for temporomandibular joint dislocation depending upon the alteration in the stability factors being ,integrity of ligaments associated with the joints , activity of the musculature on the joint , bony architecture of the joint surfaces. The article summarizes the validity of treatment option eminectomy as the treatment of choice as far as long term resolution of recurrent dislocation is desired.
In another review article by Wijmenga J.P.H. 40 cases of long standing dislocation of temporomandibular joint has been discussed in relation to the treatment modalities devised. Surgical method suggested were open reduction, condylectomy and osteotomies sometimes extended with coronoidectomy, in difficult cases condylectomy was preferred. Post condylectomy if neaarthrosis was formed with a good range of mandibular movement and malposition , some form of osteotomy was indicated.[81]
V. I. Ugboko presented a review dealing with the aetiology prevalence and treatment of tmj dislocation in the Nigerians with a sample size of 96 patients and this study has shown that excessive mouth opening while yawning is the commonest cause of temporomandibular joint dislocation in Nigerians, and conservative approaches to management remain quite effective irrespective of the duration and clinical subtype. The best choice of surgical technique had been unanimously mandibular osteotomy.[82]
Shou Shan Bu et al reported that manual reduction is the first choice for Anterosuperior dislocation which was followed by manual reduction with forcep mouth gag and in case close reduction not possible , one has to go for the open reduction, condylectomy with or without arthroplasty.[83]
Author had suggested the manual reduction with fergussen mouth gag under local anesthesia , when the conventional manual reduction had failed to relocate condyle along with chin cup and head gear to exert a continuous posterior traction on the condyle,in case of anterosuperior dislocation[84]
Kummoona et al described surgical reconstruction of TMJ for seven patients suffering from chronic subluxation & dislocation in which conservative methods have failed and reported successful outcome after long term followup.[11]
Undt G described treatment of recurrent mandibular dislocation in patient who underwent blocking procedures of Leclerc and Girard as modified by Gosserez and Dautrey and reported high incidence of clicking and pain on long term follow up , which was not present pre operatively.[21]
Vasconcelos B C et al has reported a rare case of posterior dislocation in intact mandibular condyle which was reduced under general anesthesia using zygomatic hook placed in mandibular notch.[55]
Deng M et al had discussed the use of endoscopically assisted reduction of long standing TMJ dislocation, which sounds promising to medically compromised individual, as it is a minimally invasive procedure, who cannot tolerate open procedures.
Güven O presented a retrospective study on management of chronic recurrent TMJ and compared the free excursions of the condyles achieved in the patients treated by two different techniques and found that maximum interincisal openings were higher in the patients treated by eminectomy when compared with the patients who had eminoplasty.[85]
Inverse temporomandibular joint dislocation is a rare and unique entity reported by R M Aleman, with symptoms apposite to conventional dislocation, where the patient has inability to open the mouth with a concave profile. A successful closed reduction was achieved under sedation.[86]
B C Vasconcelos et al conducted a study to compare two types of treatment for chronic mandibular dislocations, eminectomy and miniplates and concluded that the eminectomy had less chance of recurrence without creating articular damage, and with miniplates, the chance of recurrence increased because there is always the possibility of the miniplate fracturing.[28]
Spanio et al has reported the intracranial dislocation of condyle wherein the temporal craniotomy was performed and condylar head was successfully tracted downward on to the glenoid fossa which was inserted into the mandibular angle.[87]
Subhas Chandra Debnath et al reported a case of of a long-standing dislocation of the temporomandibular joint which was successfully treated in our department by bilateral vertical-oblique osteotomy of ramus extraorally without internal fixation when number of conventional modalities failed to reduce displaced condyle.[88]
Lee S et al had reported prolonged bilateral dislocation of the mandibular condyle which was simply reduced by a midline mandibulotomy without any complications compared to other surgical techniques which were often associated with the complications.[89]
A.S.R. Pinto et al reported the use of autologous blood and adjunctive face lift bandage in the management of recurrent temporomandibular joint dislocation[90]
A.M. Medra reported management of chronic recurrent dislocation and hypermobility of the temporomandibular joint with glenotemporal osteotomy and bone grafting with success.[24]
Conclusion
It was seen that female had a greater tendency for dislocation as compared to males in our study. Change of trend was seen in the management of TMJ dislocation. The more complicated and less known of treatment may does not offer best treatment outcome, therefore conservative management must always be kept in mind before opting for the more invasive surgical techniques which should be done after thorough assessment and treatment planning. Surgical treatment must therefore be based on the etiology , duration, symptoms and the experience of the surgeon. It was observed unanimously in review that all surgeons prefer closed reduction for dislocation primarily failing which open reduction is done as far as acute dislocation are concerned. For chronic recurrent dislocation the trend has been changing from condylectomy in `80 `s to eminectomy in 90`s and osteotomies along with autologous injections in 21st century. Hence we conclude the surgical treatment of TMJ dislocation is left entirely to discretion of the surgeon.
References
1. Cooper. A. Lectures on principles and practice of surgery, pp.638-640. London; Henry Renshaw.1837-8.
2. Talley RL, Murphy GJ, Smith SD, Baylin MA, Haden JL: Standards for the history, examination, diagnosis, and treatment of Temporomandibular disorders (TMD): a position paper. American Academy of Head, Neck and Facial Pain. Cranio 1990, 8(1):60-77.
3. Luyk NH, Larsen PE: The diagnosis and treatment of the dislocated mandible. Am J Emerg Med 1989, 7(3):329-35.
4. Thomas ATS, Wong TW, Lau CC: A case series of closed reduction for acute temporomandibular joint dislocation by a new approach. Eur J Emerg Med 2006, 13:72-5.
5. Sens!5;z O, Usta1;ner Et, Celebioğlu S, Mutaf M: Eminectomy for the the treatment of chronic subluxation and recurrent dislocation of the temporomandibular joint and a new method of patient evaluation. Ann Plast Surg 1992, 29(4):299-302.
6. Gambling DR, Ross PL: Temporomandibular joint subluxation on induction of anaesthesia (letter). Anesth and Analg 1988
7. Chin RS, Gropp H, Beirne OR. Longstanding mandibular dislocation: report of a case. J Oral Maxillofac Surg 1988: 46: 693–696.
8. Caminiti MF, Weinberg S. Chronic mandibular dislocation: the role of nonsurgical and surgical treatment. J Can Dent Assoc 1998: 64: 484–491.
9. Olga Vázquez Bouso,Gabriel Forteza González, Jens Mommsen et al. Neurogenic temporomandibular joint dislocation treated with botulinum toxin: report of 4 cases. Oral Surg Oral Med Oral Pathol Oral Radiol Endod 2010;109:e33-e37
10. Vladimir Machon, Shelly Abramowicz, Jan Paska et alAutologous Blood Injection for theTreatment of Chronic Recurrent Temporomandibular Joint Dislocation. J Oral Maxillofac Surg 67:114-119, 2009.
11. Kummoona R. Surgical managements of subluxation and dislocation of the temporomandibular joint: clinical and experimental studies. J Craniofac Surg. 2010 Nov;21(6):1692-7.
12. Undt G, Kermer C, Piehslinger E, Rasse M: Treatment of recurrent mandibular dislocation, Part I: Leclerc blocking procedure. Int J Oral Maxillofac Surg 1997, 26(2):92-7
13. Gadre et al. Dautrey’s Procedure for Recurrent Mandible Dislocation. J Oral Maxillofac Surg 2010
14. DAUTREY, J. (1975) Reflections sur la chirurgie de l’articulation temporomandibulare. Acta Stomatologica Belgica, 72, 577
15. Segami N, Kaneyama K, Tsurusako S, SuzukiT. Arthroscopic eminoplasty for habitual dislocation of the Temporomandibular joint: preliminary study. J Craniomaxillofac Surg 1999;27:390-7.
16. Kobayashi H, Yamazaki T, Okudera H. Correction of recurrent dislocation of the mandible in elderly patients by the Dautrey procedure. Br J Oral Maxillofac Surg.2000 Feb;38(1):54-7.
17. Lawlor MG: Recurrent dislocation of the mandible: treatment of ten cases by Dautery procedure. Br J Oral Surg 1982, 20:14-2
18. Poirier F, Blanchereau C, Francfort E, Agostini P, Petavy A, Khorshid M,Mahieddine R, Adi AR, Kolev T. [Surgical treatment of temporomandibular joint:apropos of 94 cases]. Rev Stomatol Chir Maxillofac. 2006 Dec;107(6):436-40.
19. Shibata T, Yamashita T, Nakajima N, Ueda M, Ishijima T, Shigezumi M, Arisue M: Treatment of habitual temporomandibular joint dislocation with miniplate eminoplasty: a report of nine cases. J Oral Rehabil 2002,29(9):890-4
20. Hasson O, Nahlieli O: Autologous blood injection for treatment of recurrent temporomandibular joint dislocation. Oral Surg Oral Med Oral Pathol Oral Radiol Endod 2001, 92(4):390-3
21. Undt G. Temporomandibular joint eminectomy for recurrent dislocation. Atlas Oral Maxillofac Surg Clin North Am. 2011 Sep;19(2):189-206.
22. Huang IY, et al. Management of long-standing mandibular dislocation, Int J Oral Maxillofac Surg (2011), MaCFarlane WI: Recurrent dislocation of the mandible: treatment of seven cases by a simple lateral pterygoid myotomy. Br J Oral 1977,14:227-9
23. MaCFarlane WI: Recurrent dislocation of the mandible: treatment of seven cases by a simple lateral pterygoid myotomy. Br J Oral 1977,14:227-9.
24. A.M. Medraa,A.M. Mahrous.Glenotemporal osteotomy and bone grafting in the management of chronic recurrent dislocation and hypermobility of the temporomandibular joint. British Journal of Oral and Maxillofacial Surgery 46: 119–122,2008
25. J. J. Kuttenberger, N. Hardt.Long-term results following miniplate eminoplasty for the treatment of recurrent dislocation and habitual luxation of the temporomandibular jointInt. J. Oral Maxilla/ac. Surg. 2003; 32: 474-479.
26. Emad T. Daif. Autologous blood injection as a new treatment modality for chronic recurrent temporomandibular joint dislocation. Oral Surg Oral Med Oral Pathol Oral Radiol Endod 2010; 109:31-36
27. Kai-Yuan Fua, Hui-Min Chen, Zhi-Peng Sun et al. Long-term efficacy of botulinum toxin type A for the treatment of habitual dislocation of the temporomandibular joint British Journal of Oral and Maxillofacial Surgery 48 (2010) 281–284.
28. Vasconcelos BC, Porto GG: Treatment of chronic mandibular dislocations: a comparison between eminectomy and miniplates. J Oral Maxillofac Surg 2009, 67(12):2599-604.
29. Nakashima M, Yano H, Akita S, Tokunaga K, Anraku K, Tanaka K, et al: Traumatic unilateral temporomandibular joint dislocation overlooked for more than two decades. J Craniofac Surg 2007, 18(6):1466-70
30. Thangarajah T, McCulloch N, Thangarajah S, Stocker J: Bilateral temporomandibular joint dislocation in a 29-year-old man: a case report. J Med Case Reports 2010, 4:263
31. Kai S, Kai H, Nakayama E: Clinical symptoms of open lock position of the condyle. Relation to anterior dislocation of the temporomandibular joint. Oral Surg Oral Med Oral Pathol 1992, 74:143.
32. Hoard MA, Tadje JP, Gampper TJ, Edlich RF: Traumatic chronic TMJ dislocation: report of an unusual case and discussion of management. J Craniomaxillofac Trauma. Winter 1998, 4(4):44-7.
33. Stone KC, Humphries RL: Maxillofacial and head trauma. Mandible fractures. Current Diagnosis & Treatment Emergency Medicine. 6 edition.McGraw Hill; 2008
34. Harstall R, Gratz KW, Zwahlen RA: Mandibular condyle dislocation into the middle cranial fossa: a case report and review of literature. J Trauma2005, 59(6):1495-503
35. Gassner R, Tuli T, Hachl O, Rudisch A, Ulmer H: Cranio-maxillofacial trauma: a 10 year review of 9,543 cases with 21,067 injuries. J Craniomaxillofac Surg 2003, 31(1):51-61
36. Hoard MA, Tadje JP, Gampper TJ, Edlich RF: Traumatic chronic TMJ dislocation: report of an unusual case and discussion of management. J Craniomaxillofac Trauma. Winter 1998, 4(4):44-7,
37. Laskin DM: Temporomandibular joint disorders.Edited by: Frederickson JM, Krause CJ. Otolaryngology: Head and Neck Surgery. St. Louis: Mosby- Yearbook; 1993:1443-50.
38. Ting J: Temporomandibular joint dislocation after use of laryngeal mask airway. Anaesthesia 2006, 61:201.
39. Bhandari S, Swain M, Dewoolkar LV: Temporomandibular joint Dislocation after Laryngeal mask airway insertion. The Internet Journal of Anaesthesiology 2008, 16(1):1-4.
40. Swee-Leong Sia, Yin-Lung Chang, Tsang-Mu Lee, Yu-Yung Lai Temporomandibular Joint Dislocation After Laryngeal Mask Airway Insertion. Acta Anaesthesiol Taiwan 2008;46(2):82−85
41. Sosis M, Lazar S. Jaw dislocation during general anaesthesia. Canadian Journal of Anaesthesia 1987; 34: 407–8.
42. Lipp M, Von Domarus H, Daublender M: Temporomandibular joint dysfunction after endotracheal intubation. Anaesthetisa 1987, 36:442-45.
43. Kepron W: Bilateral dislocations of the temporomandidibular joint complicating fibreoptic bronchoscopy. Chest 1986, 90:465.
44. Schwartz AJ: Dislocation of the mandible: a case report. ANAA J 2000,68:507-13.
45. Rattan V, Arora S: Prolonged temporomandibular joint dislocation in an unconscious patient after airway manipulation. Anaesth Analg 2006,102:1294.
46. Brijesh Anantharam, Navtej Chahal, Nigel Stephens, and Roxy SeniorTemporo-mandibular joint dislocation: an unusual complication of transoesophageal echocardiography. European Journal of Echocardiography (2010) 11, 190–191
47. Oliphant R, Key B, Dawson C, Chung D: Bilateral temporomandibular joint dislocation following pulmonary function testing: a case report and review of closed reduction techniques. Emerg Med J 2008, 25:435-436.
48. Rosemore J, Nikoomanesh P, Lacy BE: Bilateral temporomandibular joint dislocation after PEG tube placement. Gasintest Endosc 2004, 59:146-7.
49. Avidan A: Dislocation of the mandible due to forceful yawning during induction with propofol. JClin Anaesth 2002, 14:159-60.
50. Tesfaya Y, Skorzewska A, lai S: Hazard of yawning. CMAJ 1991, 14:156.
51. Whiteman PJ, Pradel EC: Bilateral temporomandibular joint dislocation in a 10-month-old infant after vomiting. Pediatr Emerg Care 2000, 16:418
52. Ryan M, LaDow C. Subluxation of the temporomandibular joint after administration of prochlorperazine: report of two cases. J Oral Surg. 1968 Oct;26(10):646-8.
53. Undt G, Weichselbraun A, Wagner A, Kermer C, Rasse M. Recurrent mandibular dislocation under neuroleptic drug therapy, treated by bilateral eminectomy. J Craniomaxillofac Surg. 1996 Jun;24(3):184
54. Thexton A: A case of Ehlers-Danlos syndrome presenting with recurrent dislocation of the temporomandibular joint. Br J Oral Surg 1965, 3:190-3
55. Vasconcelos BC, Rocha NS, Cypriano RV. Posterior dislocation in intact mandibular condyle: an unusual case. Int J Oral Maxillofac Surg. 2010 Jan;39(1):89-91.
56. Schuknecht B, Graetz K: Radiologic assessment of maxillofacial,mandibular, and skull base trauma. Eur Radiol 2005, 15(3):560-8.
57. Kalaykova S, Naeije M., Huddleston J. J. R. & Lobbezoo F. S . Is condylar position a predictor for functional signs of TMJ hypermobility.Journal of Oral Rehabilitation 2006 33; 349–355.
58. Keith.D. Surgery of Temporomandibular joint. Blackwell scientific publications,1988
59. Rastogi ’Nk, Vakhari N, Hung OR: Perioperative anterior dislocation of the temporomandibular joint. Anesth Analg 1997, 84:924-26
60. Worthington P. Dislocation of the mandibular condyle into the temporal fossa.J Maxillofac Surg. 1982 Feb;10(1):24-7.
61. Hippocrates. On the articulations. The genuine works of Hippocrates. Clin Orthop Relat Res. 2002 Jul;(400):19-25.
62. Lowery LE, Beeson MS, Lum KK. The wrist pivot method, a novel technique for temporomandibular joint reduction. J Emerg Med. 2004 Aug;27(2):167-70.
63. Adekeye EO, Shamia RI, Cove P. Inverted L-shaped ramus osteotomy for prolonged bilateral dislocation of the temporomandibular joint. Oral Surg Oral Med Oral Pathol. 1976 May;41(5):568-77.
64. Naumann M, Hefter H, Heinen F (1999) Dysport. Klinische Anwendung von Botulinum toxin. Uni-Med, Bremen
65. Daelen B. Neurogenic temporomandibular joint dislocation. Definition and therapy with botulinum toxin. Nervenarzt 1997;68: 346-50.
66. Porta M (2000) A comparative trial of botulinum toxin type A and methylprednisolone for the treatment of myofascial painsyndrome and pain from chronic muscle spasm. Pain 85:01–105
67. Konzetny GE. Die Behandlung der habituellen luxation der sagenannt habituellen subluxation des unterkiefers u.d kiefergelenksknachens . Ztschr Chir 1929;56:3018
68. Leclerc GC, Girard C. Un nouveau procede de butee dans letraitement chirurgical de la luxation recidivante de la machoire inferieure. Mem Acad Chit 1943;69:437-59.
69. Myrhaug H: A new method of operation for Habitual dislocation of the mandible: review of former methods of treatment. Acta Odontol Scand 1951, 9:247-61.
70. Pogrel MA: Articular Eminectomy for recurrent dislocation. Br J Oral Maxillofac Surg 1987, 25:237-43.
71. Undt G, Kermer C, Rasse M: Treatment of recurrent mandibular dislocation, Part II: Eminectomy. Int J Oral Maxillofac Surg 1997, 26:98
72. Gay-Escoda C: Eminectomy associated with redirectioning of the temporal muscle for treatment of recurrent TMJ dislocation. J Craniomaxillofac Surg 1987, 15(6):355-8.
73. Sindet-Pedersen S. Intraoral myotomy of the lateral pterygoid muscle for treatment of recurrent dislocation of the mandibular condyle. J Oral Maxillofac Surg 1988;46:445-9.
74. Miller GA, Murphy EJ: External pterygoid myotomy for recurrent mandibular dislocation. Review of the literature and report of a case. Oral Surg Oral Med Oral Pathol 1976, 42(6):705-16
75. Gould JF: Shortening of the temporalis tendon for hypermobility of the temporomandibular joint. J Oral Surg 1978, 36:781-3.
76. Dimitroulis G. Surgical management of persistent oromandibular dystonia of the temporalis muscle. Int J Oral Maxillofac Surg. 2011 Feb;40(2):222-4. Epub 2010 Sep 15.
77. Upton LG, Sullivan SM: The treatment of temporomandibular joint internal derangements using a modified open condylotomy: a preliminary report. J Oral Maxillofac Surg 1991, 49(6):578-83.
78. Lamberg MA: Closed condylotomy in the treatment of recurrent dislocation of the mandibular condyle. Int J Oral Surg 1978,7(1):1-6.
79. Gottlieb I. Long-standing dislocation of the jaw. J Oral Surg1952;10:25-32.
80. Shorey C.Dislocation of Temporomandibular joint. Oral surg Oral Med Oral pathol Oral Radiol Endod 2000;89:662-8.
81. Wijmenga et al .Protracted dislocation of temporomandibular joint, Int J. Oral Maxillofac. Surg1986:15:380 -388
82. V. I. Ugboko, F. O. Oginni, S. O. Ajike, H. O. Olasoji, E. T. Adebayo A survey of Temporomandibular joint dislocation: aetiology, demographics, risk factors and management in 96 Nigerian cases. Int. J. Oral Maxillofac. Surg. 2005; 34: 499–502
83. Shou-Shan Bu.Superolateral dislocation of the intact mandibular condyle into the temporal fossa: review of the literature and report of a case. Oral Surg Oral Med Oral Pathol Oral Radiol Endod 2007;103:185-9
84. Kale.T et al long standing temporomandibular joint dislocation:closed reduction-a case report and technical note. Journal of International Oral Health .June 2010 Vol 2 Issue 1 pg 59 -67.
85. Güven O: Review Inappropriate treatments in temporomandibular joint chronic recurrent dislocation: presenting three particular cases. J Craniofac Surg 2005, 16(3):449-52.
86. R M Aleman, Nawas et al: Inverse Temporomandibular joint dislocation . Int. J. Oral Maxillofac.Surg. 2011; In Press.
87. Spanio S et al .Intracranial dislocation of the mandibular condyle: report of two case with review of literature . BJOMS(2002 ) 40,253-255.
88. Debnath Subhas Chandra, Kotrashetti S. M. et al.Bilateral vertical-oblique osteotomy of ramus (external approach) for treatment of a long-standing dislocation of the temporomandibular joint: A case report. Oral Surg Oral Med Oral Pathol Oral Radiol Endod 2006;101:e79–e82
89. S.-H. Lee. Reduction of prolonged bilateral temporomandibular joint dislocation by midline mandibulotomy. Int. J. Oral Maxillofac. Surg. 2006; 35: 1054–1056.
90. A.S.R. Pinto, K.P. McVeigh, R. Bainton.The use of autologous blood and adjunctive face lift bandage in the management of recurrentTEMPOROMANDIBULAR JOINT dislocation.British Journal of Oral and Maxillofacial Surgery 2009; 47 323–324.
|