Introduction
Apicoectomy is a well known surgical procedure, used when conservative endodontic treatment has failed to retain natural teeth. Endodontic surgery in anterior teeth is usually carried out without hesitation, whereas in posterior regions endodontic surgery was not much preferred because of the extremely close relationship between the apices of the premolar and especially the molar teeth and the floor of the maxillary sinus in the maxilla and inferior alveolar nerve in mandible.[1],[2] Pathological exposure of the sinus floor predisposes many surgical endodontic procedures to maxillary sinus communication.[3]
A clinical case of apical surgery on a maxillary molar through the maxillary sinus is presented, using a sinus lift procedure and retrofilling with MTA.
Case Report
A 30 year old male patient with sporadic swelling in the right maxillary region (Figure 1-a) and tenderness to percussion of the maxillary first molar was referred to The Advanced Dental Care Center, Visakhapatnam . Past dental history revealed discontinued endodontic treatment 1 year back. The intraoral radiograph revealed radiolucent periapical lesion involving the three roots of the maxillary first molar and the proximity of the mesiobuccal root apex to the sinus membrane (Figure 1-b).
The temporary restoration was removed; the canals were cleaned and shaped. Calcium hydroxide was placed in to the canals and the tooth was sealed with temporary filling material.
One month after the initial visit he still complained of an intermittent sensitivity on biting for which endodontic surgery was planned. A written informed consent was given by the patient prior to surgery.
After the removal of calcium hydroxide by copious irrigation with 5% sodium hypochlorite and normal saline all the canals were filled with guttapercha and zinc oxide eugenol sealer by lateral condensation. The tooth was temporarily restored with zinc oxide eugenol.
Anesthesia was performed with buccal and palatal infiltration of 2% lidocaine and 1:80.000 adrenaline over the apices of the maxillary first molar and adjacent teeth to involve the surgical site. A full thickness flap was raised with a #15 scalpel blade to create a triangular flap. After retraction of the flap the buccal bone was assessed and no perforation of the cortical plate was evident. The position of the apices was estimated and the bone was removed with an ISO size 18 sterile bur (Dentsply Mallifer, Switzerland) in a straight handpiece with copious sterile saline using light brush strokes. The granulation tissue was curetted and osteotomy was prepared (Figure 1-c) and 3mm of root apex was resected for mesiobuccal and distobuccal roots. During the granulation tissue removal of the mesiobuccal root the schneiderian membrane was revealed and sinus lift was performed to avoid penetration at the following surgical steps (Figure 1-d). The exposed tissues were moistened with sterile saline throughout the surgical procedure to avoid dehydration of the bone and soft tissues.
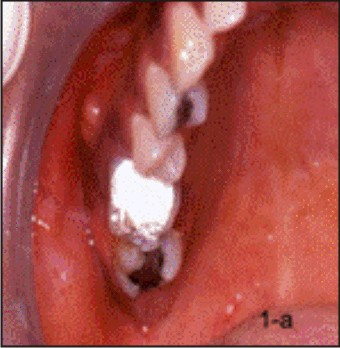 | Figure 1-a: Preoperative Clinical Picture Of 16 With Intraoral Swelling
 |
 | Figure 1-b: Pre-operative Radiograph Of 16.
 |
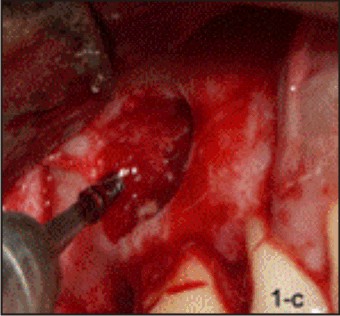 | Figure 1-c: Clinical Picture Of Osteotomy
 |
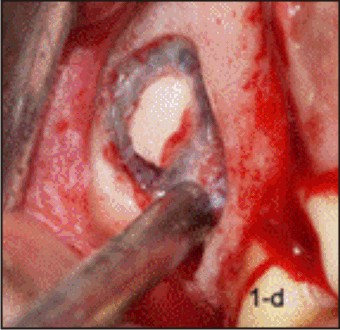 | Figure 1-d: Clinical Picture Showing Lining Of Maxillary Sinus
 |
Later full thickness flap was raised on the palatal aspect and secured with a sling suture. The root end of the palatal root was resected. The root end preparation of all the three roots was carried out with ultrasonic powered tips in a P5 unit (Satalec; France) to a depth of 3 mm. All three preparations were undertaken using copious amounts of coolant of sterile saline. The root end was dried and MTA (Proroot, Dentsply, USA) was placed with a flat plastic instrument and packed in to place with microplugger. The flap was repositioned and sutured with 5 -0 silk suture (Figure 2-a). The postoperative radiograph was taken (Figure 2-b). The patient returned one week later for suture removal with no post operative pain; healing was uneventful. The patient was examined clinically and radiographically at a 3 month and 9 month recall visit. Periapical healing around roots was observed radiographically at the 9 month recall (Figure 2-c). The tooth was restored with full metal crown (Figure 2-d).
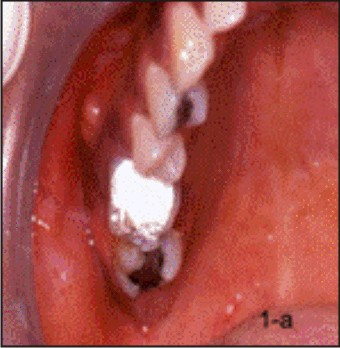 | Figure 1-a: Preoperative Clinical Picture Of 16 With Intraoral Swelling
 |
 | Figure 1-b: Pre-operative Radiograph Of 16.
 |
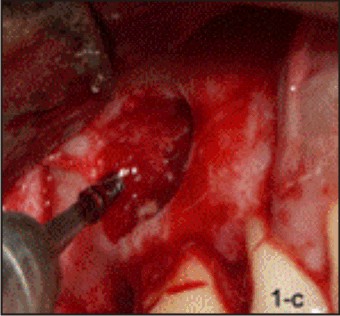 | Figure 1-c: Clinical Picture Of Osteotomy
 |
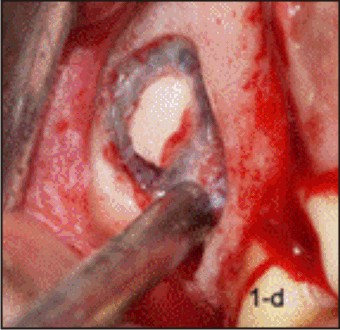 | Figure 1-d: Clinical Picture Showing Lining Of Maxillary Sinus
 |
Discussion
Periradicular surgery might be the treatment of choice in cases with an unsuccessful outcome of the primary root canal therapy of non surgical retreatment.[4] Periradicular surgery aims at the removal of disease at periapical tissues and sealing of the apical root canal system to facilitate the regeneration of hard and soft tissues including the formation of a new attachment apparatus.[5]
Periapical surgery of maxillary molar is technically more different to perform than on other teeth, because of anatomical reasons. Also, complications are potentially more serious in comparison to surgery in other regions. Bearing in mind these complications, surgical endodontics for maxillary molars should be performed by experts.
After apicoectomy there will often be sinus mucosal thickening and signs of sinusitis that may either be attributed to the introduction of foreign material in to the sinus at the time of endodontic surgery of a maxillary molar.[6] It is thus of at most importance that a meticulous technique be used to ensure that foreign material or the resected root apex does not enter the sinus.[7] Barnes (1991) suggested cutting through the bone and approaching the root from the front and below never from the above.[8]
The palatal roots of maxilla molar pose a special problem during endodontic surgical procedures. These roots are 50% closer to the sinus than they are to the palate,[9] show apical communication with the sinus 20% of the time and are less than 0.5 mm from the sinus 40% of the time.[10]
A major concern with any palatal flap is its reapproximation and reattachment following surgery. The pooling of blood between the flap tissue and the bone may cause gravitational sag with ischemia and sloughing.[11]
An advantage of surgical technique utilizing ultrasonics is that the size of the osteotomy can be reduced to just 3 to 4 mm in diameter. A smaller osteotomy results in faster healing[12] and less postoperative pain and swelling.[13] This ultrasonic technique eliminates the large bevel that was required with traditional techniques for areas with rotary burs.
The complex root canal morphology of the mesiobuccal root is an important consideration for apical surgery of the maxillary molar tooth. Degerness and Bowles examined the anatomic determination of the mesiobuccal root resection level in maxillary molars and found that 80% of lateral canals were eliminated when a 3.64 mm resection was performed.[14]
MTA has been suggested as the more appropriate root end filling material as invivo studies have shown that MTA has bio-inductuive properties in relation to bone, dentin and cementum regeneration.[15],[16],[17] Chong et al reported a success rate of 92% in a prospective study using MTA as a root end filling material.[18]
If apicoectomy of posterior teeth is properly performed the operation on molars can offer the same prognosis results as done on anterior teeth. It was reported that the success rates between 75% and 90%.[19]
Conclusion
For successful surgical management an astute knowledge of the regional anatomy and surgical technique is mandatory.
Ultrasonic retropreparation and MTA as a root end filling material are associated with improved outcome for treatment similar to orthograde treatment. Endodontic surgery cannot replace non surgical root canal treatment, however, when indicated it is a treatment modality that can enhance the outcome.
References
1. Gutmann JL, Harrison JW Posterior endodontic surgery: anatomical considerations and clinical techniques. Int Endod J 1985;18: 8–34.
2. Skoglund LA, Pedersen SS, Holst E Surgical management of 85 perforations to the maxillary sinus. Int J Oral Surg 1983;12:1–5.
3. Selden HS The endo–antral syndrome: an endodontic complication. J Am Dent Assoc 1989;119:397–402.
4. Danin J,Stromberg T,Forsgren H, Linder LE, Ramskold Lo Clinical management of non healing periradicular pathosis. Oral Surg Oral Med and Oral Pathol 1996; 82, 213-7.
5. Von Arx T, Gerber C, Hard T N Periradicular surgery of molars: a prospective clinical study with a 1-year follow-up. Int Endod J 2001; 34, 520-5.
6. Ericson S, Finne K, Persson G Results of apicoectomy of maxillary canines, premolars and molars with special reference to oroantral communication as a prognostic factor. Int J Oral Surg 1974;3:386–93.
7. Jerome CE, Hill AV Preventing root tip loss in the maxillary sinus during endodontic surgery. J Endod 1995; 21: 422–4.
8. Barnes IB (1991) Surgical Endodontics, 2nd edn. London, UK: Wright, 561.
9. Wallace JA Transantral endodontic surgery. Oral Surg Oral Med Oral Pathol Oral Radiol and Endod 1996; 82: 80–4.
10. Watzek G, Bernhart T, Ulm C Complications of sinus perforations and their management in endodontics. Dent Clin North Am 1997;41:563–83.
11. Arens DE, Torabinejad M, Chivian N, Rubinstein R (1998) Practical Lessons in Endodontic Surgery. Illinois, USA: Quintessence Publishing Co., Inc, 18.
12. Rubinstein RA, Kim S. Short-term observation of the results of endodontic surgery with the use of the surgical operation microscope and Super-EBA as root-end filling material. J Endod1999;25:43–48.
13. Kim S, Kratchman S. Modern endodontic surgery concepts and practice: a review. J Endod 2006;32:601–623.
14. Degerness R, Bowles W. Anatomic determination of the mesiobuccal root resection level in maxillary molars. J Endod 2008;34:1182–1186.
15. Torabinejad M, Pitt Ford TR, McKendry DJ, Abedi HR, Miller DA, Kariyawasam SP. Histologic assessment of mineral triodide aggreagateas a root-end filling material in monkeys. J Endod 1997;23:225–228.
16. Thomson TS, Berry JE, Somerman MJ, Kirkwood KL. Cementoblasts maintain expression of osteocalcin in the presence of mineral trioxide aggregate. J Endod 2003;29:407–412.
17. Baek SH, Plenk H Jr, Kim S. Periapical tissue responses and cementum regeneration with amalgam, SuperEBA and MTA as root-end filling materials. J Endod 2005;31:444–449.
18. Chong BS, Pitt Ford TR, Hudson MB. A prospective clinical study of mineral trioxide aggregate and IRM when used a root end filling materials in endodontic surgery. Int Endod J 2003;36:520–526.
19. Altonen, M and Mattila, K: Follow up study of apicectomized molars. Int J of Oral Surg 1976:5;33-40.
|