The concept of overdenture is not new. Overdenture can be described as any removable dental prosthesis that covers and rests on one or more remaining natural teeth, the roots of natural teeth, and/or dental implants[1]. The main advantages of conventional tooth supported overdenture are the preservation of the remaining tooth structure along with its proprioception, preservation of the alveolar bone, additional support to the dentures apart from the mucosa[2]. Additional retention can also be provided in overdenture with help of various attachment systems available depending on the requirements of the clinical case thus adding to improved patient acceptability. Compared to the conventional tooth supported overdenture, Implant supported overdenture also provides the additional support, retention and preserves the alveolar bone but the proprioception is not maintained. Moreover for implant supported overdenture to be successful other factors are also important like bone condition, loading condition, design of the prosthesis, patient’s habits etc. So wherever possible natural teeth can be preserved to utilize the advantages that overdenture offers over the conventional denture and at reduced cost from that of implant supported overdenture.
As there is an increase in the geriatric population and there has been advancements in dental field, more and more elderly patients present with partially edentulous condition instead of completely edentulous state. So for such patients the standard treatment option becomes to save few remaining teeth and provide with an overdenture instead of complete extraction followed by conventional dentures. This article focuses on few such cases which can be successfully treated with overdenture with and without attachments.
Case 1 : Coping retained overdenture
A 48 year old female patient with few remaining natural teeth presented to the Department of Prosthodontics for the replacement of missing teeth. The patient’s chief complaint pertained to the lack of function and aesthetic deficiency. Clinical examination showed completely edentulous mandibular arch and partial edentulous maxillary arch (Fig 1). The periodontal findings were not significant with mild amount of deposits and calculus. The teeth present in maxillary arch are 14,15,24,25 and are firm with no carious involvement. The patient related a history of tooth loss as a result of decay of tooth due to caries and periodontal disease.
It was concluded that maxillary first and second premolars of both right and left side had suitable periodontal support and can serve as abutments for coping retained overdenture after intentional endodontic treatment thus providing ample stability. Preliminary impression was taken with irreversible hydrocolloid. Diagnostic mounting revealed adequate interarch space for placement of acrylic teeth and short copings. The treatment plan was divided into phases. In phase 1 oral prophylaxis was done with respect to remaining natural teeth. In phase 2 endodontic treatment was done in 14,15,24,25. In phase 3 Prosthodontic treatment was rendered. Tooth preparation was done for short copings (Fig 2). After crown preparation final impression was taken with addition silicone (putty wash technique) for fabrication of dome shaped metal copings (Fig 3). After try-in, copings were cemented with resin reinforced glass ionomer cement (Fig 4).
Secondary impression were made after peripheral tracing with low fusing compound and master casts were obtained. After this face bow record was taken and transferred to articulator was done using semiadjustable articulator. Vertical jaw relations were done using phonetics, aesthetic and functional methods. Horizontal jaw relations and interocclusal records were made. The horizontal and lateral condylar guidances were set, upper and lower anteriors arranged and the incisal guidance was adjusted. The posterior teeth were set in balanced occlusion, thus ensuring even pressure in all parts of the arch while maintain stability of the denture.
 | Fig 1 : Pre-treatment Intra Oral View
 |
 | Fig 2 : Tooth Preparations For Short Coping
 |
 | Fig 3 : Final Impression With Metal Copings
 |
 | Fig 4 : Short Copings Cemented
 |
The trial denture was then tried in the mouth, vertical dimensions verified, centric and eccentric contacts were evaluated. The facial and functional harmony was studied and patient’s approval obtained. The dentures were then waxed and flasked for processing. After curing, laboratory remounting and selective grinding was done. Finally the dentures were finished and polished. The intaglio surfaces was relieved with respect to coping region and then chair side relining was done with auto polymerizing resin (Fig 5). The denture was adjusted and equilibrated. Post insertion instructions were given along with recall appointment. The oral cavity was evaluate after 24 hours to observe any sore areas and final occlusal adjustment were made
 | Fig 5 : Intaglio Surface Of Maxillary Denture
 |
Case Report 2: Access post retained overdenture
A 50 year old male patient reported to the Department of Prosthodontics with the chief complaint of difficulty in mastication of the food and desires replacement of missing teeth. Intra oral examination showed completely edentulous maxillary arch and partially edentulous mandibular arch (Fig 6). Teeth present in mandibular arch were 35 and 43, with severe gingival recession, periodontal involvement and no carious involvement. The patient had history of tooth loss as a result of chronic periodontitis.
 | Fig 6 : Pre-treatment Intra Oral View
 |
Before planning for attachment retained overdenture diagnostic mounting was done to evaluate the interarch space for the placement of attachment and acrylic resin teeth. Treatment for this patient was done in three phases as in the earlier case. In phase 1 oral prophylaxis was done to remove the calculus and deposits followed by phase 2 involved endodontic treatment of 35 and 43 followed by final prosthetic phase included access post retained overdenture.
Access post kit consists of primary reamer, countersink drill; access post and nylon cap (Fig 7). The characteristic feature of this post system is its ball and socket attachment which allows rotation of denture attachment[3].
 | Fig 7 : Access Post Kit (Eds System)
 |
Treatment Procedure
Step 1: Post space preparation
Tooth was reduced to about 1 mm above gingival margin (Fig 8). Post length was measured against the intra oral peri-apical radiograph, leaving 3-5 mm of gutta percha. Gutta percha was removed with Peeso reamer. Primary reamer was used to prepare full length of post. Countersink drill was used to create flange and secondary tier preparation. Trial insertion of access posts was done to determining their fit. To verify the length intraoral periapical radiograph was taken (Fig 9).
 | Fig 8 : Post Space Preparation
 |
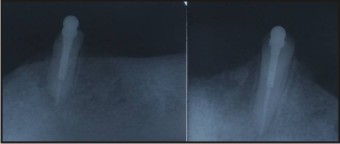 | Fig 9 : Intraoral Periapical Radiograph
 |
Step 2: Post Cementation
After verification of length and fitting of access post, cementation was done with resin cement (Fig 10). The canal was etched and luted with resin cement using lentulo-spiral. Posts were coated with resin cement and placed in canal till the flange and secondary tiers were fully seated. Excess cement was removed.
 | Fig 10 : Access Post Cemented
 |
Step 3: Denture Fabrication
Primary impression was made and custom tray was fabricated. Secondary impressions were made with medium body addition silicone. Jaw relations were recorded and teeth arrangement was done. Try in was done and the denture was processed in a conventional manner.
Step 4: Incorporations of nylon caps in mandibular denture:
Rubber bands were placed to cover the height of contour of ball of post (Fig 11). Female caps were placed on the post. Denture was seated in place and chairside reliner was allowed to set followed by removal of the denture with attachment cap (Fig 12). Rubber bands were removed and excess flash was trimmed.
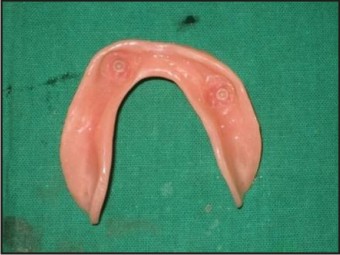 | Fig 11 : Intaglio Surface Of Mandibular Denture
 |
[Image 12]
Discussion :
Complete edentulous state affects the oral and general health as well as the quality of life of patients[4],[5],[6]. The satisfactory treatment outcome of patients rehabilitated with complete denture relies on the successful influences of prosthesis retention and stability[7],[8]. Redford et al demonstrated that more than 50% of conventional mandibular denture have problem with retention and stability and that mandibular denture have more problems than maxillary dentures, primarily because of poor prosthetic retention[9]. Residual ridge resorption is inevitable, but the extent of this process varies depending on individual anatomic, biologic, and mechanical factors. Retention of teeth or tooth roots in the alveolar bone can improve bone maintenance around and between these structures. Bone maintenance is the most significant advantage of tooth borne overdenture because the maintenance of bone volume and vertical height can produce increased prosthetic retention and stability. It also gives patient better functions, comfort and control because of proprioception[10].
In overdenture therapy abutments are prepared in dome shape contour and receive cast copings. Such denture provides mainly the preservation of alveolar bone, maintenance of proprioception and stability of prosthesis. However, if there is requirement of additional retention then variation in design is required. Long copings or attachment can be used to provide additional retention.
Selection of attachment is important and depends upon available interarch space, position of the abutment, amount of retention required, opposing dentition , clinical experience, personal preference and the cost[11].
In case report 1 short coping retained overdenture was planned for the patient to preserve the alveolar bone and maintain proprioception only as there was no additional retention requirement where as in case report 2 attachment retained overdenture was planned to meet the additional retention requirement . Access post overdenture system was used. It is stud attachment which occupies small vertical space and does not require parallelism when placed in different roots and also it allows the rotation of denture. It is relatively easy to use and cost effective. Additional feature of this post system is presence of hollowed tube design which allows venting of hydrostatic pressure during cementation and multiple tier design provides dissipation of forces. Standard nylon caps available with this provide retention of 3-5 pounds and can be easily replaced at low cost as and when required[10].
Conclusion:
Careful planning and selection is required to achieve success in overdenture therapy. However Patient maintenance is also important part of overdenture treatment to avoid failure resulting from dental caries and periodontal diseases.
References:
1. Glossary of Prosthodontic Terms. J Prosthet Dent 2005; 94.
2. DeFranco L R. Overdentures. In, Winkler S (ed), Essentials of complete denture prosthodontics, 2nd edition. USA, Inc Publishers, 2004; 384-402.
3. Cohen BI, Musikant BL, Deutsch AS.The access post and its clinical use. Dent Today 1995; 14:88-89. PMid: 9567115.
4. Marcus PA, Joshi A, Jones JA, Morgano SM. Complete edentulism and denture use for elders in New England. The Journal of prosthetic dentistry. 1996; 76(3):260-6.
5. Gift H, Redford M. Oral health and the quality of life. Clinics in geriatric medicine. 1992;8(3):673.
6. Baran Ý, Ergün G, Semiz M. Socio-demographic and economic factors affecting the acceptance of removable dentures. European journal of dentistry. 2007; 1(2):104.
7. Brill N. Factors in the mechanism of full denture retention–a discussion of selected papers. Dent Pract Dent Rec 1967;18(1):9–19.
8. Mack AO. Full dentures. Bristol, UK: John Wright and Sons, Ltd.; 1971. p. 94.
9. Redford M, Drury TF, Kingman A, Brown LF. Denture use and the technical quality of dental prostheses among persons 18–74 years of age: United States, 1988–1991 [special issue]. J Dent Res 1996;75:714–25.
10. Jain DC, Hegde V, Aparna I, Dhanasekar B. Overdenture with accesspost system: A clinical report. Indian Journal of Dental Research. 2011; 22(2):359.
11. Schwartz IS, Morrow RM. Overdentures. Principles and procedures. Dental clinics of North America. 1996;40(1):169.
|