Introduction
Diagnosis of soft tissue enlargements of oral cavity are challenges to medical as well as dental professionals because of diverse group of pathologic processes which can give rise to such lesions. Enlargements can occur due to variety of reasons which can be in the form of inflammation, cysts, developmental anomalies, and neoplasms. Reactive hyperplasias are also one of the reasons for soft tissue enlargements which develop in response to a chronic and recurring tissue injury that stimulates an exuberant or excessive tissue repair response. Pyogenic granuloma is of the most common pathology resulting in soft tissue enlargements[1].
In human beings occurrence of pyogenic granuloma was firstly reported in 1897 by Poncet and Dor which was termed as botryomycosis hominis at that time. The name pyogenic granuloma was coined by Crocker in 1903[2]. It is defined as an inflammatory hyperplasia characterised by inflamed fibrous and granulation tissues which is non-neoplastic in nature. Oral pyogenic granuloma can be seen on gingiva, lips, tongue, buccal mucosa, which shows striking predication for gingiva accounting for 75% of total cases[3].
Pyogenic Granuloma can affect person of any age, it has a wide range of occurrence of 18 to 39 years, but in children this lesion is rare[4]. Exact etiopathogenesis of pyogenic granuloma is not clear. Various theories have been proposed in relation to etiopathogenesis of pyogenic granuloma which includes hormonal factors which is seen as pregnancy gingivitis in females due to hormonal influences, trauma to the tissues that provide a pathway for invasion of nonspecific types of microorganisms which causesrelease of various endogenous substances including angiogenic factorsfrom the tumour cells and can also lead to disturbances in the vascular system of the affected area[1].The present case report shows pyogenic granuloma in 4 year old child patient due to chronic irritation.
Case Report
A four year old male child presented with a complaint of a growing mass in lower left posterior region on the floor of the mouth for more than one year.The patient couldn’t recall the exact time of initiation of the growth. The lesion was asymptomatic although its size had a potential to affect speech and mastication and used to bleed on being traumatised.
Extraoral examination didn’t reveal any facial asymmetry. No dental mobility was noted and dental vitality was normal. There were not any palpable submandibular lymph nodes either.
Intraoral examination revealed a solitary growth measuring 2 x 1 x 1 cm, in lower left lingual surface in relation to lower left deciduous canine and first deciduous molar (Fig.1). Lesion consists of lobulated reddish- purple surface which was attached through a pedunculated base on the keratinized mucosa.The mass was painless on palpation with soft consistency but with certain firm doughy margins.Routine intra oral periapical radiograph revealed normal lingual marginal bone in relation to first deciduous molar without root resorption (Fig. 2). Complete hemogram showed all blood counts within normal limits.
A conservative surgical excision of the lesion was planned. After local anaesthesia, the pedunculated mass was completely excised through the base of the lesion. The underlying tissue was curetted to prevent recurrence of the lesion (Fig. 3). After the excision of pedunculated mass, a dressing of coe-pack is applied over the raw area on the left sublingual area (Fig. 4). Antibiotics and analgesics were prescribed for 5 days. Patient was advised to have soft and cold diet and antiseptic mouthwash is prescribed to maintain oral hygiene.
 | Clinical Intraoral Image Of The Exophytic Lesion
 |
 | Intra Oral Periapical Radiograph Revealing Normal Lingual Marginal Bone.
 |
 | Clinical Intraoral Image Immediately After Extraction
 |
 | Surgical Coe-pack Placed Over Raw Area.
 |
The excised tissue was submitted for histopathological analysis. Hematoxaline - Eosin staining section showing hyperplastic stratified squamous parakeratinised epithelium with an underlying fibrovascular stroma. The stroma shows a large number of budding capillaries, fibroblasts and area of extravascular blood and dense chronic inflammatory cells. The final pathological diagnosis based on the microscopic findings was a pyogenic granuloma (Fig. 5). The patient was monitored postoperatively and one year later, the gingival tissue and the adjacent alveolar mucosa were healthy with successful healing without recurrence (Fig.6).
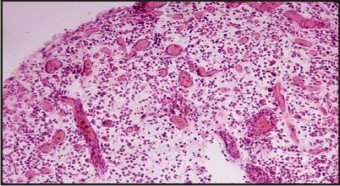 | Microscopic Appearance Showing Typical Histological Features Of Pyogenic Granuloma
 |
 | Postoperative View Of Lesion Site After One Week.
 |
Discussion
The incidence of the pyogenic granuloma has been described as between 26.8% to 32% of all reactive lesions[5] which is very high, but in children this type of lesions is very rare identity. Factors responsible can be trauma, chronic irritation and hormonal influences like in pregnancy in females which is termed as pregnancy tumour and accounts for 5% of all pregnancies[1]. Other factors which can be an etiological factor for pyogenic granuloma are drugs, gingival inflammation, exfoliation of primary teeth, eruption of permanent teeth, pre-existing vascular lesions, faulty restorations in the region of tumour, food impaction and presence of a foreign object or material[6]. It is now generally accepted that aetiological factor for the lesion is an exaggerated localized connective tissue reaction to minor tissue injury or localised chronic irritation. The most favourable site for occurrence of pyogenic granuloma is the buccal gingival, in the interproximal tissue between teeth. Other most common sites of occourance of pyogenic granulomas are gingiva, lips, tongue (especially the dorsal surface), and buccal mucosa. Pyogenic granuloma in extra gingival sites is mostly associated with a history of trauma, whereas most lesions of the gingiva are a response to chronic irritation. Individuals with poor oral hygiene and chronic oral irritants (eg, overhanging restorations, calculus) are more prone to pyogenic granuloma[7].
Pyogenic granuloma generally presents as a smooth or lobulated lesion with either pedunculated or a sessile base with a deep red or purplish colour. Pyogenic granuloma is highly vascularized lesion with high propensity for bleeding after light probing or any minor injury. The surface of pyogenic granuloma may undergo secondary or nonspecific changes which include ulceration, capillary dilation, stromal edema, inflammation and granulation tissue reaction. It’s size can range from a few millimetres to several centimetres, but lesion with size more than 3cm is rare[8],[9].
Differential diagnosis of pyogenic granuloma includes parulis, kaposis sarcoma, peripheral giant cell granuloma, hemangioma, peripheral fibroma, bacillary angiomatosis, leiomyoma, hemangioendothelioma, hemangiopericytoma, peripheral ossifying fibroma, metastatic tumour, pregnancy tumor and post extraction granuloma[10]. Foreign body reaction can also be considered as a differential diagnosis. Presence of foreign bodies in the oral mucosa is relatively rare, although some materials such as fish bones, wood, fingernail, and toothbrush bristles have been reported as etiological factor for pyogenic granuloma[11].
Treatment of Pyogenic granuloma includes surgical excision with 2mm margins at its clinical periphery and to a depth of periosteum. After surgical excision of gingival lesions, curettage of underlying tissue is recommended[12]. Even after excision, recurrence occurs in up to 16% of the lesions, making re-excision necessary. Recurrence is believed to result from incomplete excision, failure to remove etiologic factors, or re-injury of the area[13]. Other conservative techniques recommended for treatment are like cryosurgery; electrodessication and sclerotherapy [14],[15]. Recent advances have advocated the use of laser surgery by flash lamp pulsed dye laser and especially Nd: YAG laser because of its superior coagulation characteristics over CO2 laser[16],[17]. Now days lasers are fastest growing treatment options for the excision of pyogenic granuloma with added advantages of minimal pain and invasiveness and lack of need for suture placement and packing[18].
In this present case, surgical excision of the lesion was planned under local anaesthesia in the department of paediatric dentistry, Himachal Dental Collage, Sunder Nagar. To prevent relapse of the lesion, we did thorough curettage of the base of the lesion. The wound was then cleaned and irrigated with antiseptic solution. It was then closed with dressing of surgical pack (coe-pack) and antibiotic prophylaxis was given for 5 days. The patient is asked to maintain good oral hygiene using antiseptic mouth wash. After the follow up 1.5 years there is no reoccurrence due to proper removal of etiological factors and curettage of affected tissue.
Conclusion
Although pyogenic granuloma is a non-neoplastic growth of oral cavity, proper diagnosis and treatment of the lesion is very important. Pyogenic granuloma arises in response to various stimuli such as low grade local chronic irritation, traumatic injuries, sex hormones or certain drugs, so to remove the causative agent should be the major aim of the treatment to avoid reoccurrence. Excisional surgery is the most commonly followed treatment approach, although new techniques such as cryosurgery, excision by Nd:YAG laser, flash lamp pulsed dye laser, injection of ethanol or corticosteroid and sodium tetradecyl sulphate sclerotherepy have been reported as an alternative therapies.
References
1. Kamal R, Dahiya P, Puri A. Oral pyogenic granuloma: various concepts of etiopathogenesis. J Oral Maxillofac Pathol 2012; 16(1): 79-82.
2. Bhaskar SN, Jacoway JR. Pyogenic granuloma – clinical features, incidence, histology, and result of treatment: Report of 242 cases. J Oral Surg 1966;24: 391R09;8.
3. Neville BW, Damm DD, Allen CM, Bouquot JE. Oral and maxillofacial pathology 2002, 2nd edition, WB Saunders, Philadelphia 437-495.
4. Pilch BZ Head and Neck Surgical Pathology 2001. Lippincott Williams and Wilkins,Philadelphia;389-390.
5. Kfir Y, Buchner A, Hansen LS. Reactive lesions of the gingiva: A clinicopathologic study of 471 cases. J Periodontol 1980;51: 655-61.
6. Jafarzadeh H, Sanatkhani M, Mohtasham N. Oral pyogenic granuloma: a review. J Oral Sci 2006; 48(4): 167- 75.
7. Dr. Sanjay Venugopal, Dr. Shobha K.S, Dr. Netravathi T.D. Pyogenic granuloma - A case report. Journal of Dental Sciences & Research 1:1: Pages 80-85.
8. Saravana GH. Oral pyogenic granuloma: a review of 137 cases. BrJ Oral Maxillofac Surg 2009; 47(4): 318-9.
9. Yuan K, Jin YT, Lin MT. expression of Tie-2, angiopoietin-1, angiopoietin-2, ephrinB2 and ephrinB4 in pyogenic granuloma of human gingival implicates in their roles in inflammatory angiogenesis. J Periodontol Res 2000; 35(3): 165-71.
10. Fowler EB, Cuenin MF, Thompson SH, Kudryk VL, Billman MA.Pyogenic granuloma associated with guided tissue regeneration:
11. Chen H, Zhao Z, Gong X et al. A tongue granuloma due to a fish bone mimicking a neoplasm: ultrasound guided differential diagnosis. Ultraschell Med 2011; 32(Suppl 1): S1-2.
12. Marx RE, Stern D. Oral and Maxillofacial Pathology: A rational for diagnosis and treatment. Chicago. Quintessence Publishing Co; 2003. P. 21-3
13. Toida M, Hasegawa T, Watanabe F, et al. Lobular capillary hemangioma of the oral mucosa: clinicopathological study of 43 cases with a special reference to immunohistochemical characterization of the vascular elements. Pathol Int 2003; 53(1): 1-7.
14. Ichimiya M, Yoshikawa Y, Hamamoto Y, et al. Successful treatment of Pyogenic granuloma with injection of absolute ethanol. J Dermatol 2004; 31(4): 342-4.
15. Moon SE, Hwang EJ, Cho KH. Treatment of pyogenic granuloma by sodium tetradecyl sulphate sclerotherapy. Arch Dermatol 2005; 141(5): 644-6.
16. Powell JL, Bailey CL, Coopland AT, et al. Nd: YAG laser excision of a giant gingival pyogenic granuloma of pregnancy. Lasers Surg Med 1994; 14(2): 178-83.
17. Meffert JJ, Cagna DR, Meffert RM. Treatment of oral granulation tissue with the flashlamp pulsed dye laser. Dermatol Surg 1998; 24(8): 845-8.
18. Matsumoto K, Nakanishi H, Seike T, Koizumi Y, Mihara K, KuboY. Treatment of pyogenic granuloma with a sclerosing agent.Dermatol Surg 2001;27:521-3.
|