Introduction
Most dental trauma’s cannot be anticipated and if not managed with the right approach can have severe consequences and uneventful healing. Intrusion has been reported only in 0.3-2% of all traumatic injuries to the permanent teeth[1]. It can have varied complication ranging from inflammatory root resorption, pulpal necrosis, ankylosis, pulp calcification to ankylosis. So while managing such cases the main focus should be either elimination or at least reducing the above mentioned complication.[2], [3]
The final outcome of the treatment depends mainly on the extent of injury, the quality and timeliness of initial care, and the follow-up evaluation and care. The quality and timeliness of initial care contribute to a desirable outcome by promoting healing. Avoiding additional trauma to the already injured tissues has been emphasized in the literature. Long-term successful outcome of such tooth depends on critical evaluation and regular follow-up.[4] Endodontic considerations in management of traumatized tooth cannot be underestimated as the long-term success for a traumatized tooth is related to the pulpal response to trauma. Previous studies have shown 100 % incidence of pulp necrosis, 70% incidence of external root resorption, 31% incidence of marginal bone loss and 3% incidence of ankylosis in intrusive luxated permanent with closed apices.[3]
This case report describes successful management of intrusive luxation of the central and lateral incisors by surgical repositioning and root canal treatment.
Case Report
A 28 year old pregnant woman who was in her third trimester reported to the Department of Conservative Dentistry and Endodontics KLESVK Institute of Dental Science with the chief complaint of displacement of her upper front teeth due to traumatic injury (Figure 1). The patient incurred trauma to the teeth due to a fall, while fetching water about an hour before she reported. Extraoral examination revealed diffuse swelling of the upper and lower lips and laceration of the lips and perioral area. Temperomandibular joint and facial bones were examined for any pain on palpation or crepitus to rule out fractures. She had no other major injuries and her medical history was uneventful.
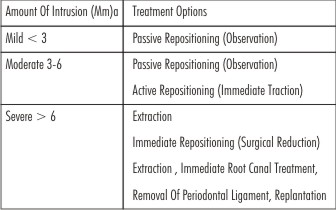
 | Table 1 : Treatment Options For Intrusions By Amount Of Intrusion
 |
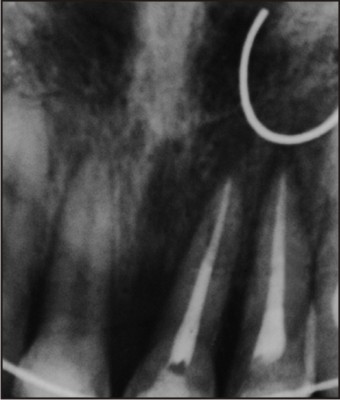
Intraoral examination revealed apical displacement of 21 and 22 deep into the alveolar bone (Figure 2). Both the affected teeth were tender on percussion with no signs of mobility. Comparing the affected teeth with the normal adjacent 11 revealed an intrusion of around 4-5mm with 21 and 7mm with 22. There were no visible signs of fracture in 11 and 12. Vitality testing for the contralateral 11, 12, 13 and 23 showed positive responses to both cold and electric testing. Laceration of the gingiva and bleeding was noted around the site of 21 and 22.
 | Figure 1 : Extraoral Photograph Showing Diffuse Swelling Of Lips
 |
Radiographic examination revealed the intrusion of 21 and 22, both the teeth had closed apices, periodontal spaces around the teeth were disrupted though no root fractures were detected (Figure 3). Since palpation of the lips due to soft tissue injury was not possible, radiographs with reduced (25-50%) exposure were also taken to allow detection of non-organic materials like glass, gravel and tooth fragments.
 | Figure 2 : Intraoral Photograph Showing Intrusion Of Teeth And Bleeding
 |
Orthodontic movement of the intruded tooth was not a viable approach at that moment, because of the severity of intrusion and completed root development. The treatment planned was of immediate surgical repositioning of 21 and 22. The area of injury was anaesthetized using topical anesthesia followed by local infiltration with 2% lignocaine hydrochloride without adrenaline. Both the teeth which were displaced from their respective sockets were repositioned and splinted to avoid any movement of the tooth during root canal treatment. The teeth were repositioned back in the sockets to a level such that the cementoenamel junction was in plane with the free gingival margin. The teeth were immobilized in their new position by splinting with 0.6 mm stainless steel wire and light-cured composite resin (Ceram X mono, Dentsply Maillefer,USA) (Figure 4, 5). All the centric and eccentric tooth contacts were eliminated by selective grinding to aid in healing and prevent further trauma to the supporting structure. Lacerations were sutured with 3-0 black braided silk. The decision to perform root canal treatment was made as the patient was not available for the conventional approach, where repositioning would be done immediately followed by multiple sitting root canal treatment after one week. So with the prospective of arresting the external inflammatory root resorption progress resulting in the loss of the tooth, root canal treatment was done.
 | Figure 3 : Radiographic Examination Indicating Intruded 21 And 22.
 |
 | Figure 4 : Stabilization With Splint
 |
Root canal treatment was performed using rotary instrument (X-smart Dentsply), cleaning and shaping was carried out with rotary NiTi files (Protaper, Densply Maillefer) and saline was used as an irrigant. Lateral condensation technique with zinc oxide eugenol sealer was used for obturation. Patient was advised antibiotic coverage and instructed to consume a soft diet, avoid any direct trauma during mastication or any other oral habits. Patient was strongly encouraged to maintain good oral hygiene during the healing period. Follow up clinical examination after 6 weeks revealed a reduction in mobility, no tenderness on percussion and good gingival healing (Figure 6). Splint removal was also carried out in the same visit. Vitality testing for 11, 12, 13 and 23 were carried out which gave a positive response. Follow-up radiograph after 5 years showed no signs of root resorption, marginal bone breakdown or ankylosis (Figure 7).
 | Figure 5 : Radiograph After Immediate Repositioning
 |
 | Figure 6 : Soft Tissue Healing After 6 Weeks
 |
Discussion
Trauma to teeth and the supporting structure can either result in separation injury, crushing injury or a combination of both. In avulsion and extrusive luxation, there is cleavage of tissues like the periodontium during displacement of teeth are examples of separation injuries. Such injuries show rapid healing after treatments as the damage of the involved cells are lesser. In crushing injuries there is displacement of teeth against alveolar bone so damage is much more due to destruction of both tissue cells and intercellular components. Intrusion is the worst example of such a injury[5].
Treatment approaches can be varied based on the stage of tooth development. Currently, conflicting evidence with few published studies with very few teeth involved are available regarding the outcomes of the different treatment approaches. Some studies have shown better periodontal and gingival healing when a more conservative approach (spontaneous or orthodontic reposition) was used rather than a surgical repositioning.[3],[6] But contradictory results have also been reported.[7] Two sets of recommendations exist for the management of intrusions-one by Andreasen and Andreasen[8] 1994 and the second by Royal College of Surgeons of England (RCSE).[9] (Table 1).
 | Figure 7 : Radiographic Evidence Of Uneventful Healing After 5 Years
 |
The protocol by Andreasen and Andreasen and the RCSE guidelines are comparable for management of incisors intruded less than 6mm. However the recommendations are different when intrusion is more than 6 mm. The evidence is minimal to support either of them.
Three treatment modalities for intrusive luxation have been suggested by Shapira et al. they are : a) await spontaneous re-eruption b) immediate surgical reduction and fixation c) orthodontic repositioning.[10] In primary or immature permanent teeth spontaneous eruption can be expected as their wide open apex has the potential to re-erupt spontaneously and establish a normal occlusal alignment within a few weeks or months. But this movement in permanent teeth after injury is unpredictable and pathological rather than developmental.[4] So such teeth should be repositioned either surgically or orthodontically or by a combination of both, because if they are allowed to remain in an intruded position, the tooth is very likely to become ankylosed, and later attempts at extrusion will probably be unsuccessful.
Severely intruded teeth do not have a functional PDL which is prerequisite for the orthodontic movement, so such teeth can be ankylosed and do not respond the teeth which are mobile and less severely intruded teeth show favorable response.[11]
Surgical repositioning provides original anatomic situation for healing of the adjacent tissues and can be done immediately.[12] It allows for removal of microorganisms from the contaminated crown and reduces periradicular compression which also decreases the osteoclastic activity. Various authors like Caliskan,[13] Caliskan et al.,[14] Ebeleseder et al.,[6] and Mazumdar et al.,[15] have recommended the surgical repositioning as the treatment of choice for intrusion in permanent teeth. Studies by Kinirons,[7] Sutcliff and Ebeleseder et al[6] have failed to demonstrate that surgical repositioning increases resorption. Though possible damage to the periodontium during extraction can lead to a higher risk of ankylosis but this can be minimized with a skilled operator.
Mazumdar et al.[15] have reported management of 2 teeth with a similar intrusion of 6mm by surgical reposition with uneventful healing and a follow up of 2 years but there endodontic treatment was initiated after 3 weeks after beginning of external root resorption and loss of marginal bone support. But in the present case neither of the complications reported by them were noted which could be attributed to the early pulp extripitation.
Nelson - filho et al.[12] have also has reported successful management of a completely intruded incisor in a 10 year old patient who had reported 15 days after incurring the trauma. They also found development of external inflammatory root resorption after 1 week of surgical repositioning which was treated with calcium hydroxide dressing for four months until the signs of external resorption were controlled which again would have not been possible in the present case due to unavailability of the patient.
Andreasen has reported a lower frequency of root resorption when the involved teeth are treated within 90 minutes.[16] In this case, the time elapsed for repositioning of the tooth was less than 90 minutes. Intrusive luxation has been shown to develop pulpal necrosis in upto 80 % of cases which is higher than any type of luxation injury.
For optimizing tissue healing two factors should be taken into consideration. One is the tooth-PDL-bone interface which should experience strains within the ‘physiologic milieu’ and the second is this interface should have controlled micro movement. This maintains sufficient blood circulation and venous return in the healing ligament encouraging revascularization; accelerating the rate of periodontal reorganization and reattachment[17]. For this reason a semi rigid composite wire splint was used in the present case.
Resorption (internal or external) occurs in 5 to 15% of luxation injuries often within the first 2 to 5 months, so follow up evaluation during the first year should be ideally done after 4 to 6 weeks and after 6 months followed by yearly recalls. Recall after 6 months and 1 year could not be done in the present case because of poor patient compliance but after 5 years satisfactory healing is satisfactory results.
Conclusion
This case presented a unique challenge of treating a rather rare traumatic injury under special circumstances. The standard procedures were not followed because the patient was in the third trimester of pregnancy and she needed immediate relief in minimal visits. Thus the decision to perform root canal and surgical repositioning in a single visit were taken. Five year follow up of the case showed that surgical repositioning combined with endodontic treatment constitutes a viable and lasting alternative treatment for intrusive luxations in mature permanent teeth. The management of intusive luxation in particular or any kind of dental trauma should be based not just on scientific evidence and research based knowledge but should also take into consideration the clinical expertise and the prevalent circumstance of the patients.
References
1. Andreasen JO, Bakland LK, Matras RC, Andreasen FM. Traumatic intrusion of permanent teeth. Part 1. An epidemiologic study of 216 intruded teeth. Dent Traumatol 2006;22:83-89.
2. Andreasen JO, Andreasen FM. Essentials of traumatic injuries to the teeth: a step-by-step treatment guide. Copenhagem: Munksgaard; 2000.
3. Andreasen JO. 35 years of dental traumatology. Lecture to the International Association of Dental Traumatology, Melbourne, Australia, March 15, 1999.
4. Andreasen JO, Andreasen FM, Bakland LK, Flores MT. Traumatic dental injuries-a manual. Copenhagen; Munksgaard; 1999.
5. Bakland LK. Andreasen JO. Dental traumatology: essential diagnosis and treatment planning Endodontic Topics 2004;7:14-34.
6. Ebeleseder KA, Santler G, Glockner K, Hulla H, Pertl C, Quehenberge RF. An analysis of 58 traumatically intruded and surgically extruded permanent teeth. Endod Dent Traumat 2000;16:34-39.
7. Kinirons MJK, Succliffe J. Traumatically intruded permanent incisors: a study of treatment and outcome. Br Dent J 1991;170:144-46.
8. Andreasen JO, Andreasen FM. Textbook and Color Atlas of Traumatic Injuries to the Teeth. 3rd edn. Munksgaard, Copenhagen.The C.V. Mosby Co 1994.p 315-82.
9. Kinirons UI: UK National Clinical Guidelines in Paediatric Dentistry, Treatment of traumatic intmded incisor teeth in children. Int J Paed Dent1998;8:165-68.
10. Shapira J, Regev L, Liebfeld H. Re-eruption of completely intruded immature permanent incisors. Endod Dent Traumat1986;2:113-66.
11. Jacobs SG: The treatment of tnumatized permanent anterior teeth: case report and literature review Part 1- management of intnided incisors Aust Orthod J 1995;13:213-18 .
12. Nelson-Filho P, Faria G, Assed S, Pardini LC. Surgical repositioning of traumatically intruded permanent incisor: case report with a 10-year follow up. Dental Traumatol 2006;22:221-25
13. Caliskan MK. Surgical extrusion of a completely intruded permanent incisor. J Endod 1998;24:381-84.
14. Caliskan MK, Gomel M, Turkun M. Surgical extrusion of intruded immature permanent incisors. Oral Surg Oral Med Oral Pathol 1998;86:461-64.
15. Mazumdar D, Roy P, Kumar P. Management of intrusive luxation with immediate surgical repositioning. J Conserv Dent 2009;12:69-72.
16. Andreasen JO. Traumatic injuries of the teeth. Copenhagen: Munksgaard; 1972.
17. Cengiz SB, Atac AS, Cehreli ZC. Biomechanical effects of splint types on traumatized tooth: a photoelastic stress analysis. Dental Traumatol 2006;22:133-38.
|