Introduction
Gingival recession is a common occurrence and its prevalence increases with age.[1] The recession of the gingival, either localized or generalized, may be associated with one or more surfaces, resulting in attachment loss and root exposure.[2] From the centuries, human beings have given great importance in terms of beauty and aesthetics. Apart from root surface hypersensitivity,[3] gingival recession can lead to clinical problems such as root caries, cervical root abrasions, difficult plaque control and diminished cosmetic and aesthetic concerns.[4] Therefore, it should not be viewed as merely a soft tissue defect, but rather as the destruction of both soft and hard tissues.[2] The incidence of gingival recession varies from 8% in children to 100% after the age of 50 years.[5] Longitudinal human studies have demonstrated the efficacy and predictability of periodontal plastic surgical procedures to correct gingival recession esthetically and functionally.[6],[7],[8],[20],[21] Factors such as bone height, biotype of gingival tissue, and anatomy of exposed root surface can have a negative impact on the degree of root coverage after a periodontal surgical procedure.[7] However on some occasions, the situation becomes even more complex, with the presence of grooves, caries, resorption, or non-carious cervical lesions (NCCLs).[8] It has been recognized that gingival recession combined with a wedge shaped defect in the cervical area are often seen affecting the same tooth & also cervical lesions (CLs) prevalence varies from 5%–85%, with both prevalence & severity increasing with age.[9]
Despite such a close association between gingival recession and CLs, only restorative procedures are being selected frequently as a single therapy.[10] The conventional restorative techniques results in protection against further loss of tooth structure and sensitivity only, but they often do not meet the esthetic demands of the highly concerned patients. Additionally these anatomical root surface presentations can impair the mechanical root planing that is done prior to the surgical procedure for root coverage procedures. In such cases, combined restorative and periodontal surgical procedures should be under taken.[11]
Clinicians in the past have used Geristore - resin ionomer restorations or fluoride-releasing resin materials with pre-reacted glass (PRG), called giomer , in the subgingival locations with predictable success.[12] It has been demonstrated histologically that both epithelium and connective tissue can adhere to the modified resin ionomers in the subgingival environment.[13] Outcome of mucogingival procedures on restored root surfaces and results of the CPF in the treatment of CLs restored with Resin Modified Glass Ionomer cement (Fuji LC Type II) is limited.[8],[14],[15] In this context, the ideal therapeutic treatment modality for gingival recession associated with CLs still continues to be a challenge to the clinicians. Thus, the aim of the present study was to evaluate the percentage of relative root coverage (rRC) by CPF in the treatment of both intact and restored root surfaces with RMGI over 6 - months postsurgically.
Materials & Method
Twenty sites were selected from patients with class I and II gingival recession and were enrolled in this study
Inclusion Criteria used was:[16] 1) Age group between 18-50 years; 2) Patients diagnosed as having buccal Miller's Class I & II gingival recession associated with and without buccal CL (abfraction, erosion, abrasion, or caries) in anterior maxillary region and premolar region; 3) Full-mouth visible plaque index and full-mouth BOP index scores <20%; 4) PSD < 3 mm; 5)KTH >1 mm.
Exclusion Criteria used was; 1) Patients having known allergy/sensitivity; 2) Use of any tobacco products by the patient; 3) Patient who is medically compromised and under medication; 4) Inability to provide informed consent by the patient; 5) Patient who is not able to maintain oral hygiene; 6) Patient who is on use of any antibiotic from past six months prior to the initiation of treatment; 7) Endodontically treated teeth; 8) History of mucogingival surgery at the defect; 9) Pregnant subjects; 10) patients were selected for this study. The patients were given detailed information and written oral hygiene instructions. After being informed about the aim of the study, consent was taken from the patients.
Study Design
The study design used was a prospective, parallel, & randomized clinical design. Based on presence or absence of CLsteeth were assigned to one of the following two groups:
GROUP 1 (Control group; n = 10): Gingival recession without CL.
GROUP 2 (Test group; n = 10): Gingival recession associated with CL.
Clinical Parameters
The following clinical parameters were assessed and recorded by the same examinerat baseline one, three and six months after the surgery: 1) Local Plaque Index (PI): Presence (1) or Absence (0) assessed by a manual periodontal probe.[16],[17]; 2) Local Bleeding on Probing (BOP): Presence (1) or Absence (0) of bleeding up to 10 seconds after gentle probing.[16],[17]; 3) Probing Sulcus Depth (PSD): Distance between the GM and the bottom of the gingival sulcus in mm.[16]; 4) Relative Recession Height (rRH): Distance between a fixed landmark (stent)[16] and the most apical point of the GM in mm.[16]; 5) Relative Clinical Attachment Level (rCAL): Distance between a fixed landmark (stent)[18] and the bottom of the gingival sulcus in mm.[16]; 6) Keratinized Tissue Height (KTH): Distance between most apical extension of the GM and the MGJ chemically disclosed with a Schiller's iodine solution in mm.[16]; 7) At the same visits, Recession Height (RH): Distance between the CEJ and the most apical point of the GM, was obtained only from the control group in mm.[16]; 8) At baseline, Lesion height (LH) & Lesion width (LW) of the CLs were obtained by means of a digital vernier caliper only from test group:
The assessed clinical parameters were used to obtain:
Recession reduction(RR):[16] calculated for both groups as- (preoperative rRH - postoperative rRH)
Clinical attachment level gain(CALG) : [16] calculated for both groups as- (preoperative rCAL - postoperative rCAL)
Percentage of relative root coverage(rRC) : [16] calculated for both groups as- (preoperative rRH - postoperative rRH) x 100 preoperative rRH
Percentage of root coverage (RC) : [16] calculated for control group as- (preoperative RH - postoperative RH) x 100 PreoperativeRH
Percentage of restored root coverage (RRC) : [16] calculated for test group as- (preoperative rRH - postoperative rRH) x 100 LH
Presurgical Procedure:[16]
Following initial examination and treatment planning, the selected patients underwent phase I therapy. All patients were instructed to use a non-traumatic brushing technique (coronally directed roll technique) with a soft tooth¬brush. After 2-4 weeks those patients who maintained optimum oral hygiene (Full-mouth visible plaque index and full-mouth BOP index scores <20%) [17] were subjected for the surgical procedure (CPF) alone in the control group and combined restorative and surgical procedures (RMGI + CPF) in the test group.An individual customized occlusal stent[18] was made by acrylic prior to surgery for both the groups. (Figure 1).
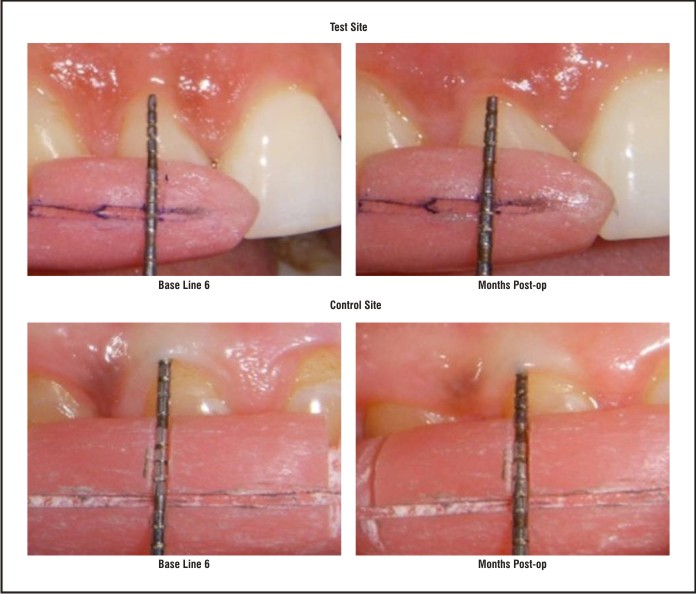 | Figure 1 : Preparation Of Occlusal Stents
 |
Restorative procedures for test group:[16]
At the beginning of the restorative appointment, the sites with gingival recession combined with CLs were assigned to the test group only. Initially, isolation of test sites was carried out by using a retraction cord. Dentin and enamel was etched by using 35% phosphoric acid gel for 15 seconds, followed by rinsing with water for 10 seconds, and the excess moisture was blotted with blotting paper. CLs were restored with RMGI after primer application and were light cured for 60 seconds as recommended by the manufacturer. Each restoration was finished grossly with a tapered, carbide finishing bur under abundant water irrigation. Final contouring and finishing were accomplished with progressively finer grit aluminum oxide disks and no attempts were made to polish the restored surfaces.[19] (Figure 2 I,II,III)
After 1-2 weeks of the restorative appointment, the subjects underwent surgical procedure by the same operator.
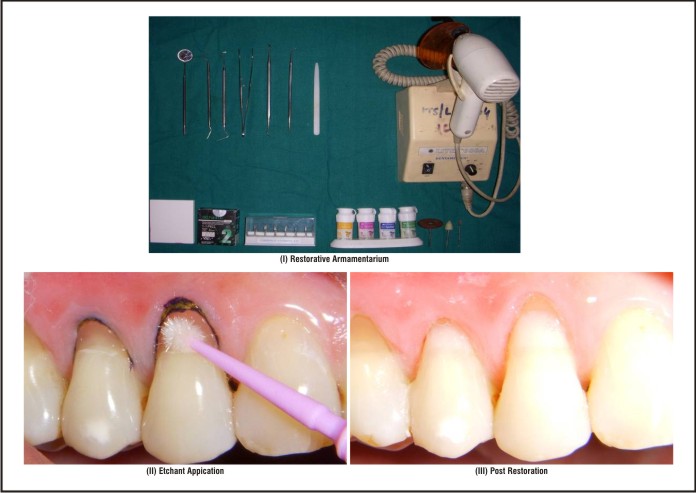 | Figure 2 : Pre And Post Restoration Photographs Of Patient With Cervical Lesion Restored With Rmgic
 |
Surgical Procedure: De Sanctis M & Zucchelli G in 2007[16], [20]:
The operative site was anaesthetized with local anesthesia (2% lidocaine with 1:200,000 epinephrine), an intrasulcular incision was made at the buccal aspect, and two horizontal incisions were made at right angles to the adjacent papillae. Subsequently, two divergent oblique incisions at the mesial and distal aspects of the recession, extending apically 3-5mm beyond the MGJ were given to complete a trapezoidal flap design. A periosteal elevator was used to reflect an initial full-thickness flap till the MGJ. After this point, a split-thickness flap was dissected apically, as necessary to release any tissue tension. The papillae adjacent to the involved tooth were deepithelialized. Tissue debridement, root planning (the root surface was planed thoroughly with periodontal manual curettes, until a smooth root surface was achieved) and irrigation with sterile saline solution was performed. The flap was displaced coronally, completely covering the operative site, and was sutured with a non-resorbable 4-0 black silk suture by sling sutures. Finally, interrupted sutures were placed at the vertical incisions to facilitate tissue stabilization. No periodontal dressing was used in this study. (Figure 3 I,II,III).
 | Figure 3 : Coronally Positioned Flap Design
 |
Data Analysis And Methodology
Data analysis was performed by using SPSS statistical package. The results were presented as mean ± standard deviation. PI, BOP, RRC, Rc, and rRC were expressed in percentages. Intragroup comparisons were made by paired “t” test and intergroup comparisons were made by unpaired “t” test. The results were also ascertained by nonparametric methods like Wilcoxan’s test and Mann-Whitney test whenever measurements were found to be non normal. A p-value of < 0.005 was considered for statistical significance.
Results
In this study, 10 patients, 6 females and 4 males aged group of 20-55 years (mean age, 41.38 ± 16.32) with a total of 20 sites satisfying the selection criteria were selected and assigned to control (CPF) and test group (CPF + RMGI). In control group 7 Class I and 3 Class II gingival recession defects were treated while in test group 4 Class I and 6 Class II gingival recession defects were treated. In the control group 3 Premolars, 3 Canines, 2 Lateral Incisors, and 2 Central Incisors while in the test group 5 Premolars, 2 Canines, 2 Lateral Incisors, and 1 Central Incisors were selected. Clinical parameters that were recorded at baseline, and at 1, 3, and 6 months after surgery were PI, BOP, PSD, rRH, rCAL, KTH, andRH(recorded only for control sites). LHand LW were also recorded at baseline only for test sites (Table 1,2). The mean ± SDfor LH and LW were 3.58 ±0.74 and 2.91 ± 0.61 respectively calculated only for the test group. All these parameters were assessed and were used to obtain RR,CALG, rRC, RC (only for the control sites) and RRC (only for test sites). The percentage of coverage of a previously exposed root surface is the primary clinical outcome used to evaluate the effectiveness of a mucogingival procedure. In this study, the RC in the control group (83.33%) confirmed the predictability of the CPF on the intact root surface with 6 sites (60%) achieving complete root coverage. The mean RC score in control group only at 6 month was 83.33% ± 22.21%,which remained unchanged at 1, 3, and 6 months. After 6 months, the maximum recession coverage achieved was 96.7% in the test group (Table 1, 3). The mean RRC at 6 months was 66.02% ± 21.87%, confirming the predictability of the CPF on the restored root surfaces with RMGI. The mean gain in KTH score in control and test group at 6 month post surgery was 0.7mm and 0.6mm. On comparison between control and test groups results were statistically not significant at baseline and 1 month and at 3 and 6 months indicating that both groups achieved approximately similar postoperative KTH values.The mean PSD score for control and test groups at 6 months post surgery was 1.0 ± 0.33mmand 1.1 ± 0.37mm respectively. The mean reduction in PSD in control group was 0.2mm & mean gain of 0.1mm in PSD in test group from baseline to 6-month post surgery, which was statistically not significant.
 | Table 1 : Clinical Parameters At Baseline, 1, 3 & 6 Months Postoperatively
 |
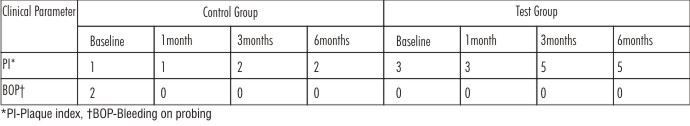 | Table 2 : Number Of Sites With Plaque Accumulation& Bopover A Period Of Time.
 |
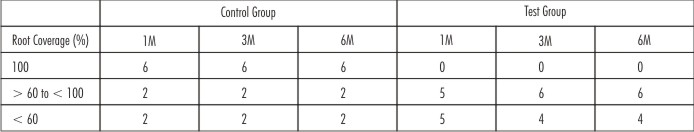 | Table 3 : Predictability Of Recession Coverage In % For Control And Test Groups.
 |
Discussion
One of the challenges for a periodontist is to cover the exposed root surfaces associated with gingival recession. When a root exposure is associated with a CL, the condition becomes more complex and then only cosmetic component of the surgical or restorative procedure may not be successful, especially in apically extensive lesions. The conventional restorative techniques results in protection against the further loss of tooth structure and sensitivity only; but they often do not meet the esthetic demands of the patients. On the other hand, if the surgical procedure for root coverage is individually performed, the coronal portion of the cervical lesion may not be covered by the periodontal flap after the healing period, giving the impression that the procedure was unsuccessful. Therefore, to solve problems of sensitivity and esthetics simultaneously, a combined restorative-surgical therapy is needed for the treatment of gingival recession associated with a CL.[11]
The percentage of coverage of a previously exposed root surface is the primary clinical outcome used to evaluate the effectiveness of a mucogingival procedure. In this study, the RC in the control group (83.33%) confirmed the predictability of the CPF on the intact root surface with 6 sites (60%) achieving complete root coverage. The mean RC score in control group only at 6 month was 83.33% ± 22.21%,which remained unchanged at 1, 3, and 6 months that demonstrated that CPF is effective and stable treatment modality. These results correlate well with the studies done by Baldi et al[21] who reported 82% ±17% mean root coverage after 3months andLucchesi et al[16] who reported 80.83% ± 21.08% mean root coverage after 6 months of evaluation period.
In the present study, based on the anatomical aspects of a root surface associated with a CL, RRC was considered for test groups instead of RC. As most coronal point of the CL probably is higher than the CEJ, a smaller percentage of tooth/restoration coverage and a reduced number of sites exhibiting complete coverage were expected in test groups than the control group. Thus the treatment effectiveness was determined as a function of RRC and periodontal tissue health at 1, 3, and 6 months after the surgical procedure. After 6 months, the maximum recession coverage achieved was 96.7% in the test group. The mean RRC at 6 months was 66.02% ± 21.87%, confirming the predictability of the CPF on the restored root surfaces with RMGI. These results demonstrate that CPF + RMGIas an effective and stable treatment modality. These results correlate well with the studies done by Alkan et al[8] who documented predictable recession coverage associated with a glass ionomer-restored root surface; Lucchesi et al[11] who reported RRC of 71.09%±18.69%. The % of restored root surfaces with RMGI achieved in our study was slightly less as 60% of teeth restored in test group were premolars in comparison to only 30% in the control group.
In the present study, based on the anatomical aspects of a root surface associated with a CL, it was statistically inappropriate to compare the percentages of coverage between control and test groups. So, we calculated rRC for both the groups. The mean rRC in control and test groups at 6 months post surgery was 15.36 % ± 5.28%and 18.01% ± 6.02%. On comparison between control and test groups, the results were statistically not significant. These findings indicated that the presence of RMGI is not a negative predictor for CPF success over a 6 months period.
Considering the mean RR, the CPF effectiveness for coverage of previously restored root surface was similar to that of an intact root. On comparison between control and test groups, the results were statistically significant at 1 and 3 months. This difference may be due to the greater number of class I gingival recession defects included in the control group than the test group, where Class II gingival recession defects were more in number. The mean RR in control and test groups at 6 months post surgery was 1.3 ± 0.41mmand 1.6 ± 0.58mm and was statistically not significant. These results correlate with the study done by Lucchesi et al[16] & Santos et al.[22] Although, in the present study, within the test group mean RR reduced to 0.3mm from 1 month to 6 months postoperatively, the reduction was statistically not significant, and must be observed in longitudinal evaluation for a longer period. As the periodontal flap was displaced coronally, covering RMGI restorations, it can be assumed that all restorations had their apical border placed in a subgingival location. Although some studies reported that subgingival restorations are harmful to gingival health in long term, Schatzle et al[23] demonstrated that a pathogenic periodontal process may develop slowly and take 1 to 3 years to be detected clinically. In their study authors did not discuss about the type of restorative materials used and technique variables.
In the present study the increase in % of sites showing plaque accumulation in control and test groups from baseline to 6-months post surgery was only 10% and 20% only & the decrease in % of sites showing bleeding on probing in control and test groups from baseline to 6-months post surgery was only 20% and 0%. On comparison between control and test group results were statistically not significant. Thus the data from this study revealed that the restorations in test group do not produce greater gingival inflammation and plaque accumulation compared to the control group. These results correlate well with the studies done by Santos et al[22] who concluded that for the RMGI + CPF group, there was a significant decrease in the proportions of nine periodontopathogens vs Microfilled Composite + CPF and the control group. They also documented no significant differences in PI and BOP scores and thus suggesting that well-finished RMGI or microfilled composite subgingival restorations did not negatively affects the periodontal health in their 6-months evaluation period. These findings probably are related to the fact that all patients in this study performed optimal plaque control, and the restorations were carried out on the buccal aspects of the teeth only, where oral hygiene procedures are easily facilitated. Furthermore, the restorative materials and technique variables were controlled precisely, and restorations were contoured and finished accurately following manufactures instructions, as these procedures are essential to avoid gingival inflammation and plaque accumulation over a period of time.[24]
Initial keratinized tissue thickness and height and have been proposed as essential anatomical factors associated with complete root coverage in a CPF procedure.[21] In this study, the mean gain in KTH score in control and test group at 6 month post surgery was 0.7mm and 0.6mm. On comparison between control and test groups results were statistically not significant at baseline and 1 month and at 3 and 6 months indicating that both groups achieved approximately similar postoperative KTH values. These results correlate well with the studies done byLucchesi et al[16] and Santamaria et al[14] whoreported that the CPF was associated with some gain in KTH scores on the restored root surfaces during the 6 month follow up, but results were statistically not significant. In addition, post surgery KTH remained unchanged at 3 and 6 months after surgery in test group, suggesting that subgingivally placed RMGI restoration may not jeopardize these gingival features over a 6 month period of time.
A periodontal plastic procedure is considered to be successful when the post surgical gingival margin is at the CEJ, with a PSD < 2 mm with presence of clinically attached gingiva, and no BOP.[25] In the present study the mean PSD score for control and test groups at 6 months post surgery was 1.0 ± 0.33mmand 1.1 ± 0.37mm respectively. The mean reduction in PSD in control group was 0.2mm & mean gain of 0.1mm in PSD in test group from baseline to 6-month post surgery, which was statistically not significant. On comparison between control and test groups, results were statistically not significant & correlates well with the studies done by Santos et al[22]; Lucchesiet al[16] and Santamaria et al.[14]
In the present study, the shallow PSDs were observed post operatively and consistently in both the groups, thus indicating that CPF was associated with CALG on both intact and restored root surfaces during the observed period.The mean CALG in control and test groups at 6 months post surgery 1.5 ± 0.54mm and 1.3 ± 0.43mm. On comparison between control and test groups, results were also statistically not significant, indicating that both groups achieved approximately similar CALG postoperatively. These results correlate with the studies done by Lucchesi et al[16] and Santamaria et al[14] & also correlate with the landmark study by Dragoo[15] wherein he showed clinical and histologic evidence of epithelial and connective tissue adherence to resin ionomer restorative materials during the healing process. However, in the present study we lack histologic evidence to rule out the healing pattern as a repair response (epithelium and /or connective tissue adaptation) or true attachment.
Conclusion:
The results in this study conclude that the CPF is a predictable treatment modality on both intact root surfaces and restored root surfaces with RMGI. As the true benefits for the patient are improved esthetics and the stability of the results overtime, it is relevant to evaluate whether these successful outcomes remain stable or not. Resolution of both gingival and dental defects is one great advantage of this integrated approach. Whether and to what extent these restorations may influence the periodontal tissue negatively, considering the material deterioration, must be observed in longitudinal evaluation for a longer period.
Acknowledgement
The present study received no funding. The authors do not possess any financial relationships that may pose a conflict of interest or potential conflict of interest.
References
1. Serino G, Wennström JL, Lindhe J, Eneroth L. The prevalence and distribution of gingival recession in subjects with a high standard of oral hygiene. J Clin Periodontol.1994; 21(1): 57-63.
2. Kassab MM, Cohen RE. The etiology and prevalence of gingival recession. J Am Dent. Assoc 2003; 134(2): 220-25.
3. Sauro S, Mannocci F, Watson TF, Piemontese M, Sherriff M, Mongiorgi R.The influence of soft acidic drinks in exposing dentinal tubules after non-surgical periodontal treatment: a SEM investigation on the protective effects of oxalate-containing phytocomplex. Med Oral Patol Oral Cir Bucal 2007; 12(7): 542-8.
4. Seichter U. Root surface caries: A critical literature preview. J Am Dent Assoc 1987; 115:305-10.
5. Wooter C. The prevalence and etiology of gingival recession. Periodont Abstr 1969; 17-45.
6. Wennstrem JL. Mucogingival therapy. Ann periodontol 1996;1:671-701.
7. Prato GP, Bald C, Nieri M. Coronally advanced flap: Thepost¬ surgical position of the gingival margin is an important factor for complete root coverage. J Periodontol 2005;76:713-22.
8. Alkan A, Keskiner L, Yuzbasioglu AE. Connective tissue grafting on resin ionomer in localized gingival recession. J Periodontol 2006;77:1446-51.
9. Sangnes G, Gjermo P. Prevalence of oral soft and hard tissue lesions related to mechanical tooth cleaning procedures. Comm Dent Oral Epidemol 1976;4:77-83.
10. Terry DA, Mc Guire MK, Mc Laren E, Fulton R, Swift EJ, Barnes P. Perioesthetic approach to the diagnosis and treatment of carious and non carious cervical lesions. Part I. J Esthet Restor Dent 2003;15:217-32.
11. Terry DA, Mc Guire MK, Mc Laren E, Fulton R, Swift EJ. Perioesthetic approach to the diagnosis and treatment of carious and non carious cervical lesions. Part II. J Esthet Restor Dent 2003;15:284-96.
12. Scherer W, Dragoo MR. New subgingival restorative procedures with Geristore resin ionomer. Pratt Peri¬odontics Aesthet Dent 1995;7:1-4.
13. Dragoo MR. Resin-ionomer and hybrid-ionomer cements: Part II, human clinical and histologic wound healing responses in specific periodontal lesions. Int J Periodont Restor Dent 1997;17:75-87.
14. Santamaria MP, Suaid FF, Nociti Jr. FH, Casati MZ, Sallum AW, and Sallum EA. Periodontal surgery and glass ionomer restoration for the treatment of gingival recession associated with non-carious cervical lesions: Report of 3 cases. J Periodontol 2007;78:1146-53.
15. Dragoo MR. Resin-ionomer and hybrid-ionomer cements: Part II, human clinical and histologic wound healing responses in specific periodontal lesions. Int J Periodont Restor Dent 1997;17:75-87.
16. Lucchesi J.A, Santos V.R, Amaral C.M, Peruzzo D.C, and Duarte P.M. Coronally advanced flap for treatment of restored root surfaces: a 6-month clinical evaluation. J Periodontol 2007;78:615-23.
17. Ainamo J, Bay I. Problems and proposals for recording gingivitis and plaque. Int Dent J 1975;25:229-35.
18. Christopher CD, Chin QT, Bergeron MJ, Chan ECS, Lautar LC, Degruchy K. Reliability of Attachment Level Measurements Using the Cemento-enamel Junction and a Plastic Stent. J Periodontol 1987;58:115-8.
19. Hand JS, Hunt RJ, Reinhardt JW. The prevalence and treatment implications of cervical abrasion in the elderly. Gerodontics 1986;2:167-70.
20. De Sanctis M, Zucchelli G. Coronally advanced flap: a modified surgical approach for isolated recession-type defects: Three-year results. J Clin Periodontol 2007;34:262-8.
21. Baldi C, Prato GP, Pagliaro U, Nieri M, Saletta D, Muzzi L, Cortellini P. Coronally Advanced Flap Procedure for Root Coverage. Is Flap Thickness a Relevant Predictor to Achieve Root Coverage? A 19-Case Series. J Periodontol 1999;70:1077-84.
22. Santos VR, Lucchesi JA, Cortelli SC, Amaral CM, Feres M, Duarte PM. Effects of Glass Ionomer and Microfilled Composite Subgingival Restorations on Periodontal Tissue and Subgingival Biofilm: A 6-Month Evaluation. J Periodontal 2007;78:1522-8.
23. Schtazle M, Land NP, Anuerd A, Boysen H, Burgin W, Loe H. The influence of margins of restorations on the periodontal tissues over 26 years. J Clin Periodontol 2001;28:57-64
24. Laurell L, Rylander H, Petterson B. The effect of different levels of polishing of amalgam restorations on the plaque retention and gingival inflammation. Swed Dent J 1983;7:45-53.
25. Miller PD Jr. Root coverage with free gingival grafts. Factors associated with incomplete coverage. J Periodontol 1987;58:674-81.
|