Introduction
Musculoskeletal disorders (MSDs) have become increasingly common worldwide during the past decades. It is a common cause of work-related disability among workers with substantial financial consequences due to workers' compensation and medical expenses[1]. Dentistry is a demanding profession regarding concentration and precision. Most dentists today work in the sitting position treating the patient in the supine position. Because their work area (the mouth of the patient) is narrow, performance of dental treatment results in a very inflexible work posture[2].
The prevalence of work related musculoskeletal complaints in dentist is high and the past two decades have witnessed a sharp rise in the incidence of various disorders. Studies have shown that dentists have a high frequency of musculoskeletal disorders[3],[4],[5]. The prevalence of general musculoskeletal pain ranges from 64% to 93%. The most effected regions for pain in dentist have been shown to be the back and neck, while the hand and wrist regions were the most common regions for dental hygienist[6].
Dental professionals are among the workers who are more often susceptible to MSDs; they often cannot avoid prolonged static postures. Even in optimal seated postures, more than one half of the muscles of the body are contracted statically and there is a little movement of the vertebral joints. This may result in many pathologies such as tendinitis, synovitis, tenosynovitis, and bursitis[7],[8]. Occupational diseases have not only physical, psychological, and social consequences, but also economic[9] and security impacts when they reach a level of severity that directly affects work capacity, causing absences and early retirement[10].
A number of studies have found that the mechanisms leading to work-related musculoskeletal pain are multifactorial[11],[12].The MSD pain can be attributed to numerous risk factors, including prolonged static postures, repetitive movements, suboptimal lighting, poor working positioning, genetic predisposition, mental stress, physical condition, and age. Each dental team member is predisposed to pain or injury in slightly different areas of the body, depending on the tasks and positioning in relation to the patient[13].
Since 1992 the Occupational Safety and Health Administration (OSHA) has been preparing Federal legislation concerned with ergonomic hazards in at risk workplaces[14]. Ergonomics is the study of people at work to understand the complex relationships among people, machines, job demands, and work methods. As long as stress is kept within reasonable limits, work performance will be satisfactory and the worker’s health and well-being will be maintained. However, if stress is excessive, undesirable outcomes may result in the form of accidents and injuries. A variety of musculoskeletal injuries and disorders can be caused by physical stress in the work environment[15],[16].
The purpose of this pilot study were first, to describe the prevalence and distribution MSDs, secondly, to identify the relationship between working hours per day and MSDs occurring in dentists practicing in Sangli district, Maharashtra, India. In addition, the different treatment modalities of MSDs were also explored.
Materials and Method
A questionnaire pilot study was carried out among a sample of convenience of 60 Indian dentists from Sangli district, Maharashtra. These dentists were belonging to different specialization fields and practicing general dentistry. The only criterion for eligibility to the study was at least one year in clinicalpractice after becoming qualified bachelor or master degree in dentistry and subjects were selected randomly. Subjects with histories of fractures or major trauma, degenerative disc disease, spondylosis and spinal stenosis, neurological deficits and systemic illness were excluded. The dentists were contacted during their free hours and a written consent was obtained from all the participants on a voluntary basis.
For collecting the data, a close ended questionnaire was designed. It was requested that dentists complete and return the questionnaire on the same day. Many complied and returned their complete questionnaire on the same day. For those who did not, we reminded them twice during one week of period to complete and return the questionnaire.
The questionnaire consisted of three major parts: Its first part collected general information about subject’s age, gender, marital status, education level, working hours per day, type of employment (permanent or temporary). The second part was entirely dedicated to the subject’s region of MSDs. The third part of the questionnaire investigated the different treatment modalities subjects were taking for MSDs. The questionnaire was pilot- tested on a group of 10 dentists prior to finalization. After completion of the questionnaire, the candidates were interviewed to clarify any confusion and to furnish any missing data.
Statistical Analysis
Data were entered into the Microsoft excel program and analyzed using SPSS (Statistical Package for Social Sciences version 20.0 software). Basic statistics were calculated, including prevalence rates. The collected data was summarized by calculating frequency and percentage for discrete variables and mean, standard deviation for continuous variable like age and sex. The analysis was performed by using Pearson’s chi- square test to identify the significant difference between the discrete data. P-values below 0.05 were considered statistically significant throughout.
Results:
Among 60 dentists (mean age 37.6, SD 8.05) interviewed by questionnaire, 30 were males (mean age 40.5, SD 8.55) and 30 were females (mean age 34.7, SD 6.45), and the age range of the study subjects was 26-65. These subjects were divided into three groups according to age: <30 (12 subjects), 31-40 (31 subjects), >41 (17 subjects).
Prevalence of MSDs in these subjects is 88.33% i.e. 53 subjects have MSDs among 60. In these subjects, highest prevalence is in 31-40 years age group (41.67%), next age group is >41 years (28.33%) and <30 years age group (18.33%).
Since many subjects presented multiple MSDs, the total number of such disorders far exceeds the number of subjects with MSDs. The greatest single MSD is lower back, with 41 subjects (68.33%). Other MSDs in decreasing order is; shoulder with 40 subjects (66.6%), neck with 34 subjects (56.6%), hand &wrist with 14 subjects (23.33%), hip with 11 subjects (18.33%), upper back with 10 subjects (16.67%), knee with 8 subjects (13.33%), ankle with 6 subjects (10%) (Graph 1). Statistically significant difference between different age group (<30, 31-40, >40) is observed in lower back, knee and ankle MSDs (p<0.05) and no statistical significant difference between different age group in other MSDs. (Table 1)
High prevalence rate of MSDs is observed in females (46.6%) as compared to males (41.6%), but only the lower back and upper back MSD is high in males (38.3% & 10% respectively) compared to females (30% & 6.6% respectively). There is no statistical significant difference observed between males and females in various MSDs. (Table 2 & Graph 2)
Prevalence rate of MSDs in those who are working <5hrs (43.3%) is nearly same as those who are working >5hrs (45%) per day. Only in upper back, lower back and hip MSDs are slightly high prevalent in those who are working <5hrs compared to those who are working >5hrs per day. But, the prevalence rate is comparatively high in knee and ankle disorders in those who working <5hrs per day and also statistically significant difference is observed (p<0.05). (Table 3)
The different treatment modalities seeking by the subjects are as follows; Massage (26.6%), Exercise (31.6%), Medication (36.6%) and alternative treatments (10%). Massage, exercise and alternative treatments are observed high in males whereas medications like analgesics and muscle relaxants are observed high in females and also statistically significant difference is observed (p<0.05). (Table 4) (Graph 3)
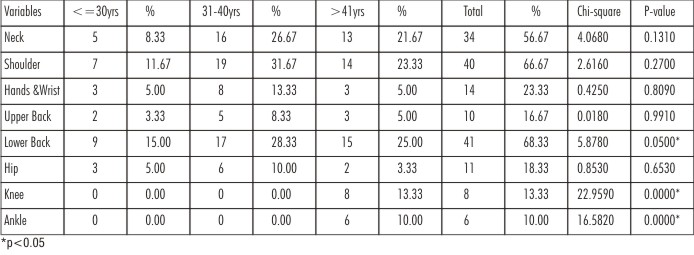 | Table 1: Prevalence of MSDs by age groups
 |
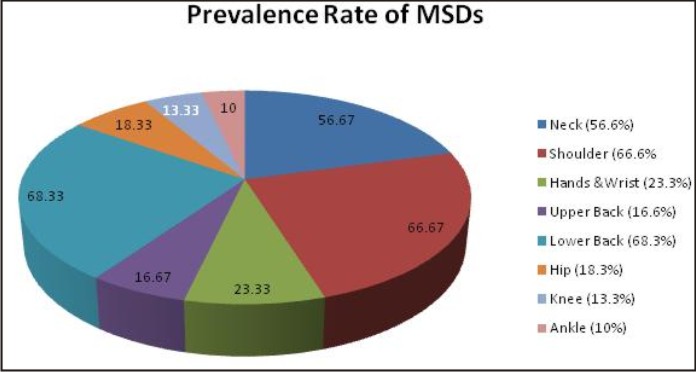 | Graph 1: Prevalence of MSDs
 |
 | Table 2: Prevalence of MSDs by sex
 |
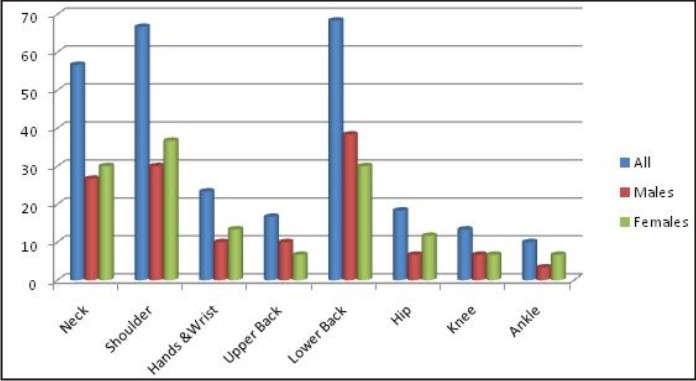 | Graph 2: Prevalence of MSDs by sex
 |
 | Table 3: Prevalence of MSDs by working hours per day (in hrs)
 |
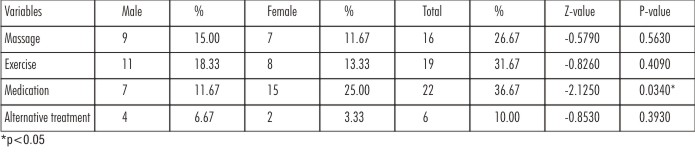 | Table 4: Distribution of different treatments for MSDs and sex
 |
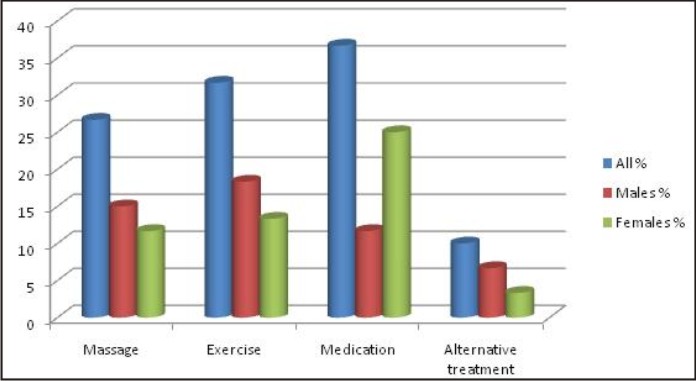 | Graph 3: Distribution of different treatments for MSDs and sex
 |
Discussion
The dentists are normally included within the group of professionals at risk of suffering from MSDs due to prolonged awkward or forced postures at work and failure to adopt preventive measures[17]. The present study found that most of the dentists had some kind of musculoskeletal pain and stiffness while performing their professional work in the last 6 months.
The mechanism of musculoskeletal pain production has been studied extensively. The onset of modern dentistry, as evidenced by four-handed dentistry, has made the major part of the dentist’s tasks purely sedentary in nature. This has resulted in dramatic rise in musculoskeletal symptoms[18].
The present study shows the prevalence of MSDs among dentists (88.33%). In a study conducted by Dajpratham et al[19], they found high number of participants (96.3%) reported presence of MSDs. Sartorio et al[20] in their review found a prevalence of MSDs ranging from 54-93%. In these studies authors found slightly higher prevalence of MSDs compared to our study. This may be because in other two studies authors included clinical instructors, post graduate students, dental assistants and hygienist in sample but in our study we included only qualified dentists with one year clinical experience.
In our study, there are no significant differences found in basic demographic data and different MSDs between the female dentist and male dentist. In 30 female dentist 28 (93.3%) are suffering from MSDs, which is higher than male dentist 25 (83.3%). This was similar to the recent studies by Omid Aminia et al[21] (91.6%), Kierklo et al[22] (92%) and Leggat et al[23] (87.2%). This could be explained because female usually has lower threshold of tolerance than male.
In the present study, the frequency of MSDs decreases with age and number of year in practice i.e. <40 years age, 60% MSDs and >41 years age, 28% MSDs. The low occurrence of MSDs among older dentists may be due to the “healthy workers effect”. In addition, older dentists have been taught to more frequently use the dental mirror for directly inaccessible areas in the patient’s mouth and older dentists are more specialized with fewer loads of patients, while younger dentists are mainly practicing general dentistry.
Major MSDs in our study showed that 68.3% lower back disorders, 66.6% shoulder disorders and 56.6% neck disorders. Contrary to this, Dajpratham et al[19] found shoulder pain in 72.2%, neck pain in 70.3% and low back pain in 50.6%. Hayes et al[24] found neck pain 64.29%, lower back pain 57.94% and shoulder pain 48.41%. In general, the MSDs in this study were consistent with the other studies[25],[26],[27].
Morken[28] found in his study that, 21% hand and wrist disorders, 20% upper back disorders, 18% hip disorders, 14% knee disorders and 10% ankle disorders which is consistent with our study.
Two studies evaluated the reports of treatments taken by dentists with MSDs. Dajpratham et al[19] found Thai traditional massage (51.9%), medication (28.5%), physical therapy (15.8%), acupuncture (7.6%) and alternative medicine (4.4%) was taken for pain relief. Augustson and Morken[28] found incorporating ergonomic equipment into dental practice alleviated shoulder discomfort. In present study, massage (26.6%), Exercise (31.6%), medication (36.6%) and alternative medicine (10%) was taken for pain relief. There is a statistical significant results were found between males and females in medication treatment for MSDs.
This study gives an insight into the prevalence and various MSDs among Indian dentists. Improper applications of ergonomics in practice put them at risk for the occurrence of MSDs. MSDs are major reason leading for loss of work efficiency as well as early ill health retirement among dentists and the prevalence and severity of these disorders decrease by using proper body posture and positioning during clinical procedures, incorporating regular rest breaks, maintaining good general health, and performing exercises for the affected regions of the body. The presented results are based on the experiences of the respondents. Using physical examinations in this study would provide more detailed information. The study allowed for a general assessment of the occupational health hazards among the dentists and further research should be encouraged.
Conclusion
Within the limitations of the study, musculoskeletal complaints are common among dentists. Lower back pain is the most common complaint followed by neck pain and shoulder pain. There was no significant difference between male and female dentists with regard to MSDs. The prevention and reduction of MSDs among dentists should include their education in dental ergonomics and awareness regardingthe importance of work-related risk factors.Further research is now needed to more carefully elucidate the impact of MSD on dentists, especially with respect to the cessation or reduction of clinical practice, and also to identify specific risk factors and effective measures for reducing MSD among them.
Reference
1. Andersson GBJ: Epidemiologic features of chronic low back pain. Lancet 1999, 354:581-5.
2. Finsen L, Christensen H, Bakke M. Musculoskeletal disorders among dentists and variation in dental work. Appl Ergon 1998; 29(2):119-25.
3. Shugars D, Miller D, Williams D, Fishburne C, Srickland D. Musculoskeletal pain among general dentists. General Dentistry 1987; 4:272-6.
4. Murtomaa H. Work related complaints of dentists and dental assistants. Int Arch Occup Environ Health 1982; 50: 231-6.
5. Kajland A, Lindvall T, Nilsson T. Occupational medical aspects of the dental profession. Work Environ Health 1974; 11:100-7.
6. Hayes M, Cockrell D, Smith DR. A systemic review of musculoskeletal disorders among dental professionals. Int Dent Hyg 2009; 7:159-65
7. Carvalho MV, Cavalcanti FI, Miranda HF, Soriano EP. Partial rupture of supraspinous tendon in a dentist: A case report. FIEP Bull 2006; 76:131.
8. Doorn JW. Low back disability among self- employed dentists, veterinarians, physicians and physical therapists in The Netherlands. Acta Orthop Scand 1995; 263 (suppl):1- 64.
9. Wunsch Filho V. The Brazilian workers’ epidemiological profile. Rev Bras Med Trab 2004; 2: 103-17
10. Hill KB, Burke FJ, Brown J, Macdonald EB, Morris AJ, White DA, Murray K. Dental practioners and ill health retirement: A qualitative investigation into the causes and effects. Br Dent J 2010; 209:E8.
11. Rundcrantz BL, Johnsson B, Moritz U, Roxendal G. Occupational cervicobrachial disorders among dentists: psychosocial work environment, personal harmony and life-satisfaction. Scand J Soc Med 1991; 19(3):174–80.
12. Murphy DC. Ergonomics and the dental care worker. Washington: American Public Health Association; 1998:113–128, 191, 344, 350.
13. Yamalik N: Musculoskeletal disorders (MSDs) and dental practice Part 2. Risk factors for dentistry, magnitude of the problem, prevention, and dental ergonomics. Int Dent J 2007; 57(1):45-54.
14. Keyserling WM, Chaffin DB: Occupational ergonomics— methods to evaluate physical stress on the job. Annu Rev Public Health 1986; 7:77-104.
15. Pollack R: Dental office ergonomics: how to reduce stress factors and increase efficiency. J Can Dent Assoc 1996;62(6):508-10.
16. Branson BG, Williams KB, Bray KK, McLlnay SL, Dickey D: Validity and reliability of a dental operator posture assessment instrument (PAI). J Dent Hyg 2002; 76(4):255-61.
17. Szymanska J. Disorders of musculoskeletal system among dentists from the aspect of ergonomics and prophylaxis. Ann Agric Enviorn Med 2002; 9:169-73.
18. Pope M. Muybridge lecture. In: Proceedings of XIV Congress International Society of Biomechanics, Paris. 1993.
19. Dajpratham P, Ploypetch T, Kiattavorncharoen S, Boonsiriseth K. Prevalence and associated factors of musculoskeletal pain among the dental personnel in a dental school. J Med Assoc Thai 2010; 93: 714-721.
20. Sartorio F, Vercelli S, Ferriero G, D’Angelo F, Migliario M, Franchignoni M. Work-related musculoskeletal diseases in dental professionals: 1- prevalence and risk factors. G Ital Med Lav Ergon 2005; 27: 165-169.
21. Omid Aminian, Zahra Banafsheh Alemohammad, Khosro Sadeghniiat-Haghighi. Musculoskeletal Disorders in Female Dentists and Pharmacists: A Cross-Sectional Study. Acta Medica Iranica, 2012;50(9): 635-640.
22. Kierklo A, Kobus A, Jaworska M, Botulinski B.Workrelated musculoskeletal disorders among dentists: A questionnaire survey. Ann Agric Environ Med 2011;18(1):79-84.
23. Leggat PA, Smith DR. Musculoskeletal disorders selfreported by dentists in Queensland, Australia. Aust Dent J 2006;51(4):324-7.
24. Hayes MJ, Smith DR, Cockrell D. Prevalence and correlates of musculoskeletal disorders among Australian dental hygiene students. Int J Dent Hyg 2009a; 7: 176-181.
25. Samotoi A, Moffat SM, Thomson WM. Musculoskeletal symptoms in New Zealand dental therapists: prevalence and associated disability. N Z Dent J 2008; 104: 49-53.
26. Thornton LJ, Barr AE, Stuart-Buttle C, Gaughan JP, Wilson ER, Jackson AD et al. Perceived musculoskeletal symptoms among dental students in the clinic environment. Ergonomics 2008; 51: 573-586.
27. Tezel A, Kavrut F, Tezel A, Kara C, Demir T, Kavrut R. Musculoskeletal diosrders in left- and right- handed Turkish dental students. Int J Neurosci 2005; 115: 255-266.
28. Augustson TE, Morken T. Musculoskeletal problems among dental health personnel- a survey of the public dental health services in Hordaland. Tidsskr Nor Laegeforen 1996; 116: 2776-2780.
|