Introduction:
Beauty has been defined as a combination of qualities that give pleasure to the senses or to the mind. It is a philosophical concept, the aspects of which are studied under the term aesthetics, derived from the Greek word for perception (aisthesis).Aesthetics, therefore,is the study of beauty and, to a lesser extent, its opposite, the ugly. It involves both the understanding and evaluation of beauty, proportions and symmetry.[1] The assessment of facial beauty is immersed in subjectivity and therefore leans towards the world of art. Facial proportions and facial balance, however, can be measured and therefore fit somewhere between art and science. Aesthetics itself is now essentially a science in the formation, although obviously with a very strong philosophical and artistic background.
Historical Background:
In western literature beauty has been described as everything from a ‘social necessity’ to a ‘gift from God’, with facial beauty being perhaps the most valued aspect of human beauty. The human perception of facial beauty may have genetic, environmental or multifactorial foundations. A considerable quantitative meta-analysis undertaken by Langlois et al[2] seems to confirm that there is also cross-cultural agreement regarding facial beauty. with composite facial photographs gaining higher attractiveness ratings than their individual facial photographs.[3] However, Perrett[4] have shown that attractive composite faces were made more attractive by exaggerating the shape differences from the sample mean. Therefore, an average face shape is attractive but may not be optimally attractive.[5] Facial symmetry also seems to be an important aspect of facial beauty, although mild asymmetry is essentially normal.[6] Therefore, our perception of what constitutes facial beauty seems to be multifactorial.
Facial Proportion And Symmetry:
The concept that ‘ideal’ proportions are the secret of beauty is perhaps the oldest idea regarding the nature of beauty.[7] Throughout the ages, painters and sculptors have attempted to establish ideal proportions for the human form, however, possibly the most famous of all axioms about ideal proportions is that of the Golden Proportion.[8] This is a geometrical proportion in which a line AB is divided at a point C in such a way that AB/AC = AC/CB. That is, the ratio of the shorter section to the longer section of the line is equal to the ratio of the longer section to the whole line. This gives AC/AB the value 0.618, termed the Golden Number. The point at which the line is divided is known as the Golden Section and is represented by the symbol (Phi), derived from the name of the Greek sculptor Phidias. This proportion has classically been described as pleasing to the eye, the emphasis being upon the proportion of the parts to the whole.
Importance Of Facial Aesthetics:
Self image and negative self-perception: A person’s own perception of their facial appearance and any associated deformity is of great importance.[9] Of course, there is considerable individual variation in people’s abilities to adapt to their facial deformity, whatever the severity. Some individuals remain comparatively unaffected, while others may have significant difficulties, which affect their quality of life.
Social disability: It has been argued that facial deformity may be a ‘social disability’, as its impact is not only on the individual affected, but is noticed by and reacted to by others.[10] Attractive children tend to be perceived more positively by their parents,[11] by teachers who perceive more attractive children as being more intelligent[12] and, in professional life, where less attractive adults are perceived as having fewer qualifications and less potential for employment success.[13] Although an individual’s facial appearance contributes to the opinions other people form of them, obviously these opinions may well change as interpersonal relationships form. Nevertheless, an individual’s first impression on others may well affect their own self-esteem and quality of life.
Stereotyping: It is suggested that people tend to stereotype others based on their facial appearance. For example, individuals with significant Class II malocclusions and mandibular retrognathia/retrogenia may be seen as weak and possibly idle, whereas individuals with significant Class III malocclusions and mandibular prognathism may be seen as aggressive personality types.
Teasing: Children in the school environment can be unsympathetic and hostile to those with visible differences, with teasing and bullying being everyday occurrences. The frequency of teasing directed at those with dentofacial differences is significant.[14]
Severity of deformity : The psychological distress caused by a facial deformity is not proportional to its severity. Research seems to indicate that facial deformities of a mild to moderate nature actually cause patients greater psychological distress than severe facial deformities.[15] This is thought to be because other people’s reactions towards milder deformities are more unpredictable, whereas more severe deformities tend to evoke more consistent reactions, albeit negative, allowing the patient to develop better coping strategies. The variability in people’s reactions to milder facial deformities also results in considerable patient distress.
Clinical assessment: The most important aspect of the clinical assessment is for the clinician to know what to look for. Leonardo da Vinci called this ‘saper vedere’, or ‘Knowing how to see’.[16] Every face has disproportions and asymmetries, as does every smile and its associated dentition. Therefore, it requires a clinician’s educated eye if the correct diagnosis is to be reached.
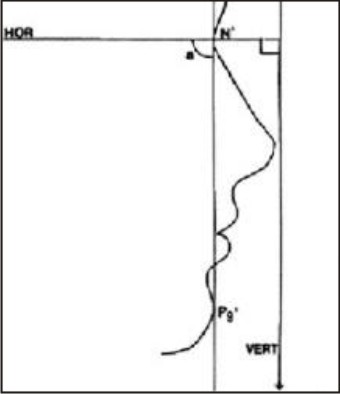
Natural head position: In order to assess facial proportions patients must be examined in natural head position (NHP).[17] NHP (Fig. 1) is a standardized and reproducible position of the head in space when the subject is focusing on a distant point at eye level. In NHP, the visual axis is horizontal. This allows an extra-cranial vertical, and a horizontal perpendicular to that vertical, to be used as reference lines for facial aesthetic analysis. This is important as the cant or inclination of all other reference lines, such as the Frankfort plane, is subject to biologic variation.[18]
 | Concepts Of Dentofacial Esthetics - An Overview
 |
Frontal facial analysis
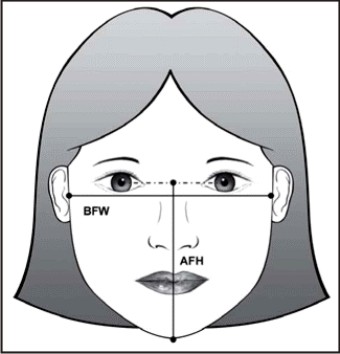
Facial type: The facial height to width ratio (Facial index) (Fig. 2) gives the overall facial type, such as ‘long’ or ‘short’ or ‘square’ face .The proportionate facial height to width ratio is 1.35:1 for males and 1.3:1 for females. Bizygomatic facial width, measured from the most lateral point of the soft tissue overlying each zygomatic arch (zygion), is approximately 70% of vertical facial height. In addition, bitemporal width, measured from the most lateral point on each side of the forehead, is 80−85% of bizygomatic width. Bigonial width, measured from the soft tissue overlying the most lateral point of each mandibular angle (soft tissue gonion), is usually 70−75% of bizygomatic width.
 | Neha Vaidya Vishal Seth Sidharth Shankar
 |
Vertical facial proportions: Knowledge of vertical proportions is important in any prosthodontic treatment plan aimed at altering the occlusal vertical dimension, as well as in planning dentofacial surgery. The vertical facial thirds should be approximately equal, although the lower facial third may be slightly greater than the middle third in males. The lower facial third may be further subdivided, with the upper lip forming the upper third and the lower lip and chin forming the lower two-thirds.
Transverse facial proportions: The ‘rule of fifths’ describes the ideal transverse proportions of the face to comprise equal fifths, each roughly equal to one eye width. The alar base width should be equal to the intercanthal width. This is important clinically as anterior repositioning of the maxilla tends to increase the alar base width. This may be partially counteracted by the placement of a ‘cinch suture’ at the time of surgery to maintain the alar base width.
Facial symmetry: The face must also be examined for bilateral symmetry, bearing in mind that a small degree of asymmetry is present in most individuals and essentially normal.The facial midline can be constructed using two main landmarks. The mid-philtrum of the upper lip (Cupid’s bow) will be in the midline of the face, except in exceptional circumstances, e.g. cleft lip. A line joining this point to the mid-glabellar region (glabella), midway between the eyebrows, forms the facial midline. In the symmetrical face, this line will extend to the mid-point of the chin. The presence of a cant in the transverse occlusal plane may be assessed in relation to the interpupillary line with the patient biting on a wooden spatula, either in the incisor/canine region or the premolar/molar region. In the absence of a maxillary cant and/ or vertical orbital dystopia, the transverse occlusal plane should be parallel to the interpupillary line.
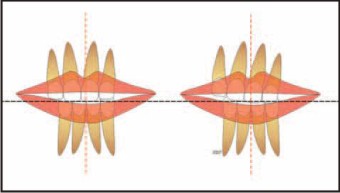
Dental midlines: The relationship of the dental midlines to their respective jaws and to the facial midline must also be assessed. The maxillary dental midline (Fig. 3) can be assessed in relation to the midpoint of the upper lip (Cupid’s bow). In addition to the relationship of the maxillary incisors to the facial midline, their transverse angulation must also be assessed.[19] The mandibular dental midline is assessed in relation to the midpoint of the chin.
 | Senior Lecturer , Dept. of Prosthodontics Senior Lecturer , Dept. of Orthodontics Reader, Dept. of Periodontics Himachal Dental College
 |
Upper lip to maxillary incisor relationship: Leonardo da Vinci described the importance of the ‘strongly movable section of the face around the mouth and chin in determining facial expression’, emphasizing the importance of observing the face in animation as well as static.[4] The vertical exposure of the maxillary incisors in relation to the upper lip at rest should be 2−4 mm, and on smiling the entire crown of the maxillary incisors should be exposed, with up to 1−2 mm of associated gingiva. A spontaneous smile, which is involuntary and expresses joyous emotion, tends to raise the upper lip slightly more than a posed `smile, which is voluntary.
Dark buccal corridors: The ‘buccal corridor’ or ‘negative space’ is the space created between the buccal surface of the posterior teeth and the commissures of the lips when a patient smiles. The presence of dark buccal corridors may be due to transverse narrowing of the maxilla, especially in the premolar region. Expansion of the maxillary arch is required in order to fill the corners of the smile. Palatal angulation of the maxillary posterior dentition. Increased palatal root torque and/or expansion of the posterior maxillary dentition, primarily the premolar region, are required. In cosmetic dentistry, an increase in the thickness of the buccal aspect of ceramic restorations on the premolar teeth may help to fill out the smile. Retro-positioned maxilla. Maxillary advancement is the treatment of choice.
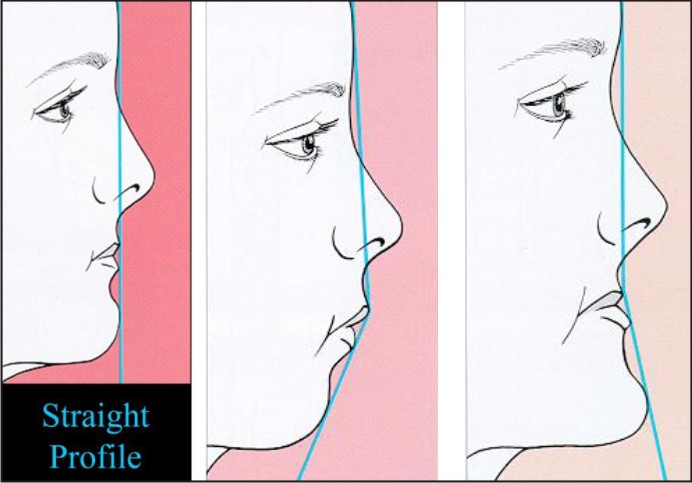
Facial profile analysis : Facial profile (Fig. 4, 5) convexity is an indication of an underlying Class II skeletal pattern either due to maxillary prognathism, or more likely due to mandibular retrognathism. Facial profile concavity is an indication of an underlying Class III skeletal pattern either due to maxillary retrognathism or mandibular prognathism, or both. Paranasal hollowing is a sign of midface deficiency, as are a flattened upper lip and an obtuse nasolabial angle. Increased sclera show above the lower eyelid, normally assessed in the frontal facial examination, is also a sign of midface deficiency.A number of useful soft tissue profile analyses exist. [20], [21], [22], [23], [24] The clinical examination may be supported by lateral and posteroanterior cephalometric radiographs with in-depth analyses to assess the soft tissues [25],[26] and underlying hard tissue relationships further.[27] Three dimensional imaging may also be used to assess more complicated cases, including severe asymmetries and craniofacial deformity.[28]
 | Dr. Neha Vaidya Senior Lecturer Department Of Prosthodontics, Himachal Dental College Sundenagar (H.P.)
 |
 | The clinical ability to alter dentofacial form requires an understanding of facial aesthetics. This is vital for any clinician involved in treatment that will alter a patient’s dentofacial appearance, whether through facial growth modification, corrective
 |
Conclusion:
In the assessment of dentofacial aesthetics, art and science must act in unison. The clinician must be able to discuss every treatment option with the patient, both in terms of its effects on dental aesthetics and its potential effect on facial aesthetics, be it positive or negative. As our clinical practice should always be based upon a sound knowledge of theory, this article has described the historical and theoretical background to our contemporary understanding of facial aesthetics and a number of useful basic guidelines for the clinical evaluation of dentofacial aesthetics have been described to aid the clinician involved in the treatment of patient.
References:
1. Naini FB, Moss JP, Gill DS. The enigma of facial beauty: esthetics, proportions, deformity and controversy. Am J Orthod Dentofacial Orthop 2006; 130: 277–282.
2. Langlois JH, Kalanakis LE, Rubenstein AJ, Larson AD, Hallam MJ, Smoot MT. Maxims or myths of beauty: a metaanalytic and theoretical overview. Psychol Bull 2000; 126: 390−423.
3. Langlois JH, Roggman LA. Attractive faces are only average. Psychol Sci 1990; 1: 115−121.
4. Perrett DI, May KA, Yoshikawa S. Face shape and judgements of female attractiveness. Nature 1994; 368: 239−242.
5. Arvystas M. Orthodontic Management of Agenesis and other Complexities: An Interdisciplinary Approach to Functional Esthetics. New York: Martin Dunitz Ltd, 2003.
6. Grammer K, Thornhill R. Human facial attractiveness and sexual selection: the role of symmetry and averageness. J Comparative Psychol 1994; 108: 233−242.
7. Peck H, Peck S. A concept of facial esthetics. Angle Orthod 1970; 40: 284−317.
8. Ricketts RM. The biologic significance of the divine proportion and Fibonacci series. Am J Orthod 1982; 81: 351−370.
9. Cash TF, Pruzinsky T. Body Images: Development, Deviance, and Change. New York: Guilford Press, 1990.
10. Macgregor F. After Plastic Surgery: Adaptation and Adjustment. New York: Praeger, 1979.
11. Langlois JH, Ritter JM, Casey RJ, Sawin DB. Infant attractiveness predicts maternal behaviours and attitudes. Dev Psychol 1995; 31: 466−472.
12. Clifford M, Walster E. The effects of physical attractiveness on teacher expectation. Sociol Educ 1973; 46: 248.
13. Hosoda M, Stone-Romero EF, Coats G. The effects of physical attractiveness on job-related outcomes: a metaanalysis of experimental studies. Personnel Psychol 2003; 56: 431−462.
14. Shaw WC, Meek SC, Jones DS. Nicknames, teasing, harassment and the salience of dental features among schoolchildren. Br J Orthod 1980; 7: 75−80.
15. Macgregor F. Social and psychological implications of dentofacial disfigurement. Angle Orthod 1970; 40: 231−233.
16. Pedretti C. Leonardo da Vinci: Notebook of a Genius. Milan: Powerhouse Publishing, 2001.
17. Moorrees CFA, Kean MR. Natural head position: a basic consideration in the interpretation of cephalometric radiographs. Am J Phys Anthropol 1958; 16: 213−234.
18. Downs WB. Analysis of the dentofacial profile. Angle Orthod 1956; 26: 192−212.
19. Kokich VO, Kiyak HA, Shapiro PA. Comparing the perception of dentists and lay people to altered dental esthetics. J Esthet Dent 1999; 11: 311−324.
20. Ricketts RM. A foundation for cephalometric communication. Am J Orthod 1960; 46: 330−357.
21. Steiner CC. Cephalometrics for you and me. Am J Orthod 1953; 39: 729−755.
22. Holdaway RA. A soft tissue cephalometric analysis and its application in orthodontic treatment planning. Part 1. Am J Orthod Dentofacial Orthop 1983; 84: 1−28.
23. Merrifield LL. The profile line as an aid in critically evaluating facial esthetics. Am J Orthod 1966; 52: 804−822.
24. Bergman RT. Cephalometric soft tissue facial analysis. Am J Orthod Dentofacial Orthop 1999; 116: 373–389.
25. Arnett GW, Jelic JS, Kim J et al. Soft tissue cephalometric analysis: diagnosis and treatment planning of dentofacial deformity. Am J Orthod Dentofacial Orthop 1999; 116: 239−253.
26. Bass NM. Measurement of the profile angle and the aesthetic analysis of the facial profile. J Orthod 2003; 30: 3−9.
27. Bishara SE. Textbook of Orthodontics. Philadelphia: Saunders, 2001.
28. Bishara SE, Burkey PS, Kharouf JG. Dental and facial asymmetries: a review. Angle Orthod 1994; 64: 89−98.
|