Key-Message :
1. Pay proper attention on selecting the case & motivation of patient for proper maintenance.
2. Give consideration to health of bone, blood supply & diagnostic aids.
3. Do plan the final prosthesis before starting the case.
Introduction
Oral Implantology has come a long way and has become preferred solution to various edentulous situations. The market is flooded with many manufacturing companies & varieties of implants. Patients have also started preferring oral implant over conventional dentures & bridges but this happy picture gets spoiled when we come across various problems or troubles during & after the procedure.
Implant failure, is one such problem when the implant is brought into function and may lead to either premature loss of prosthesis or implant itself from the oral cavity. This may have negative impact on the esteem of patient and may also lead to loss of faith from the dentist.
None of the dentists who specialize in oral implantology would like to face such a situation of embarrassment and hence it becomes essential for them to know where they may have difficulties while executing the planned treatment for the patient and how they could be rectified.
What is a Trouble
When we see the word meaning of ‘Trouble’ it says that a condition of adversity. In Oral Implantology it can be said that when an unexpected situation occurs with negative impact on the efforts of the treating doctor it is a ‘Trouble’.
Various Stages where one can have Trouble with Implants are-
Onset of Surgery
During the Procedure
After the Implant Placement
Loading of Implant by prosthesis
Implant in service
This presentation is focused on the post-operative stages where the surgery is over and implant has been placed on the desired site and has been fully functional.
After surgical site has healed implant failure is largely classified as –
(1) Loss of Integration
(2) Positional failure
(3) Soft Tissue Defect
(4) Biomechanical failure
(1) Loss of Integration : -
Failure of dental implant is often related to the failure of the implant to osseointegrate correctly with the bone or vice versa. A dental implant is considered to be a failure if it is lost, mobile or shows peri-implant bone loss of greater than 1.0 mm in the first year & greater than 2.0mm two year after.
Balshi listed three categories that may explain implant failure according to the severity of the damage to the implant and surrounding tissues.
(i) Ailing Implant
‘Ailing Implant’ is defined as clinically stable implant affected by bone loss with pocketing but static at the maintenance check-up. (R.M. Meffert) Diff Diag & Rx Strat
One in which the surrounding soft tissues are inflamed or exhibit some type of localized trauma. They respond favorably to antimicrobial/anti-infection therapies.
Bone is affected at the earliest level of 1-2mm of crestal changes which are progressive and leads to further loss of bone thus creating a vicious cycle.
Management-Regular oral prophylaxis & brushing
(ii) Failing Implant
An implant characterized by progressive bone loss without marked mobility is considered to be ‘failing’. In failing implant bone loss occurs with pocketing, bleeding upon probing, purulence and there is evidence of continuing bone loss irrespective of therapy.
Management-Periodontal therapy & surgical debridement (curettage), Laser Photo activated disinfection.
(iii) Failure to Integrate (Failed Implant) (Figure-1)
‘Failed Implant’ exhibits mobility or is fractured and must be removed. The site after removal can be grafted and further therapy undertaken.
It is diagnosed radiographically unless the breakdown of the interface with bone has proceeded to the level where the implant becomes clinically mobile.
The radiographic appearance of integration is the presence of a layer of dense bone next to the implant surface and minimal cratering of the ridge crest where it is penetrated by the implant. Where there is evidence of reduced bone density beside the implant or a space between the two then the lack of adequate integration must be suspected.
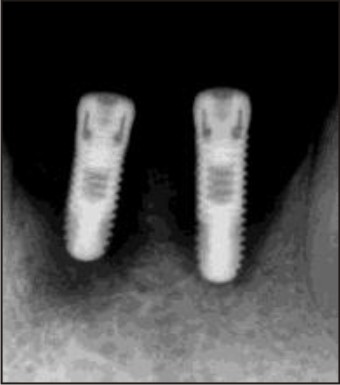 | Figure 1
 |
Underlying causes for the problem are:-
a) Bone Metabolism - impaired either by age related calcium deficiency, bone disorders, medical condition like diabetes or prior radio-therapy of the site before implant is placed
b) Local Infection - specially seen in case of immediate implants where the implant is placed in the fresh extraction socket. The underlying pathology of the socket can impair the integration.
c) Inappropriate preparation of bone by over heating - a fault on the part of the dental surgeon when the technique is improper and no adequate cooling is done while drilling the bone. It is also called as thermal necrosis of bone.
d) Bone of unsuitable quality - when the underlying bone is of D4 category and is loaded in a short span of time, it may lead to non-integration of the implant.
e) Inadequate primary stability - a factor often overlooked by the dentist in a hurry to load the implant as soon as possible.
When implants are in failing mode; and perio-implant repair is tried, bone loss greater than 1-2 mm around the implant creates continuous problems since the bone will not predictably re-osseointegrate & soft tissue may not adept adequality.
Epithelial growth might occur in the gap which may lead to deep pocket formation and lodgment of bacteria in the site; thus ultimately leading to implant failure.
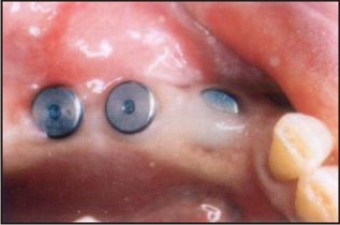
Management (Figure-2)
Implant should be removed and the region is left for healing for 6-12 months, when a further fixture may be placed if required.
A different site may be chosen or a sleeping fixture brought into use by making a new prosthesis or modifying the existing one.
 | Figure 2
 |
(2) Positional Failure
A) Malposed Implants (Figure-3)
A condition often seen because of mistake on part of the operating dental surgeon. This occurs when the surgical guide is not being used for guidance and there is change of direction while drilling the bone. When the access is limited or when multiple implants are being placed in a single procedure, there is quite a chance of loosing the orientation of direction and ultimately resulting in malposed implants.
 | Figure 3
 |
Management :
To avoid procedural error 3D CT dental scan or CBCT Scan and surgical guide is useful. As they give us information in all three planes so we can see the volume of the bone rather than just a 2D image which will give limited information. The safe distance is 3 mm between 2 implants and 1.5-2 mm between implant & tooth.
When the mistake is of minor type and there are just mal-aligned implants which are not parallel but are placed at a safe distance from each other or from the neighboring teeth, the condition can be corrected and again the parallelism can be achieved by help of ‘Angled Abutments’ (angulated at various degrees). They are the modified version of the normal abutments and are especially helpful in dicey situations of proclined or mal-aligned teeth and implants.
B) Unaesthetic Results due to wrong position of implant (Figure-4)
Implant placement in esthetic zone requires precise three dimensional tissue reconstruction and ideal implant placement. If it’s path is misdirected, it can create unaesthetic result like diastema or wrongly angulated prosthesis.
 | Figure 4
 |
Management
This can be corrected by monitoring the implant placement so that error doesn’t happen or by using angled abutment post healing of implant to some extent.
Also a surrounding-type abutment can be used in place of metal abutment to achieve more aesthetically appropriate aspect if the implant placed too high.
(3) Soft Tissue Defect :-
A) Soft Tissue Enlargement (Figure-5)
Often, Some time after the implant is placed in service a soft tissue growth is seen around the implant site once the tissues have stabilized after healing. This is seen resulting in inflammation of the area leading to Gingivitis
 | Figure 5
 |
This hyperplasia of the gingiva is mainly due to chronic irritation caused by:-
Positioning of bar too close to the soft tissue ridge
Short height abutments
Exposed threads of the implant
Poor oral hygiene of the patient
When the bar is placed too close it causes hypertrophy and hyperemia of the soft tissues leading to spontaneous bleeding that requires cutting back the tissue.
If the bar is kept more than 3 mm off the ridge this problem doesn’t occur.
Similarly the short height abutments causes irritation to the soft tissue when the masticatory load is excessive as the tissue gets impinged under them.
When the threads of the implant get exposed, a capillary seepage of microbes occurs from the surrounding area to the implant site leading to chronic infection.
Management
Periodontal treatment of the site is a must, thus ridding the area off the micro-organisms and hence the infection. The patient is also advised and taught to maintain the oral hygiene in a good manner so that there is minimum chance of deposition of plaque in the area.
B. Soft tissue deficiencies:
The transmucosal part of the implant restoration may emerge through non keratinized mucosa particularly in situation where there has been severe loss of bone e.g. edentulous Jaws. Non-keratinized mucosa looks redder and more delicate than keratinized tissue and may lack attachment to the underlying bone. This can give rise to soreness and compromised plaque control, particularly in implant denture cases. Persistent soreness and inflammation can be overcome by grafting keratinized mucosa to the site in a procedure that is the same as free gingival graft using donor tissue from palate.
Management
To correct the gingival defect grafting of the soft tissue is done around the implant so as to make the gingiva thicker and to provide a wider base for the abutment.
Also with the help of healing abutments an emergence profile is created.
‘Emergence profile’ is a thick band of gingiva formed around the healing abutments when left in place for few weeks. This band of soft connective tissue gives the appearance as if the crown is emerging from the gums and is not an artificial prosthesis.
C. Persistent gingivitis
Persistent inflammation discomfort may arise due to poor implant positioning & over contoured prosthesis which may be difficult to clean. It may require recontouring of the soft tissues to allow patient cleaning, and this may reveal the less than satisfactory aesthetics produced by poor planning and execution of treatment. In other more severe cases the only remedy may be to remove the implants or bury them permanently beneath the mucosa.
(4) Biomechanical failure :-
(A) Pain : Three main causes for it are
(i) Loosening of abutment
(ii) Creation of excessive stress in implant-prosthesis system
(iii) Damage to any anatomical area.
i) Loosening of Abutment
It happens in the case where the abutment is attached to the implant by means of screw.
The screw connects the implant to the abutment thus holding the two parts together. As the screw is of very small size the threads present on it are very delicate. Any excessive pressure while tightening the screw or wrong angulations of the driver may cause damage to the threads thus leading to loosening later on.
When an abutment does not fit precisely on a fixture it may also cause considerable pain which is sharp in nature and is due to pinching of soft tissues between the two components. This type of pain is relieved by tightening the fixing screw.
Before it is done the soft tissues should be retracted by running a probe gently in the crevice around the abutment.
Also it is to be noted that loose abutments can lead to implant failure in the long run. Hence they shall be tightened on priority basis. This problem can be minimized by friction lock abutments or by using screw retained prosthesis.
ii) Creation of excessive stress in implant-patient system
This is a typical condition seen mostly in case of ‘Bruxers’; or in the patients having Para-functional habits.
In the natural dentition when there is high load on the teeth the periodontium adapts to it by thickening of the lamina dura of alveolar bone and hypertrophy of periodontal ligament fibers. The teeth adapt to the force by getting attrited and flattening of the occlusal table, but in case of implants this is not possible.
Hence the excessive force is bear by the bone and the implant. When the force exceeds the thresh hold limit focal pressure necrosis occur at the sites where the load is maximum and the patient feels the pain in the region.
If untreated this may lead to bone necrosis around the implant site as the osteoclasts get generated in large numbers outnumbering the osteoblasts and ultimately the implant gets loosened and lost.
iii) Damage to any anatomical area.
Before placement of implant some anatomic consideration should be assessed. Particularly for mandibular implants, in the vicinity of the mental foramen, there must be sufficient alveolar bone above the mandibular or inferior alveolar canal. Failure to precisely locate the IAC & MF invites surgical insult by the drills and the implant itself.
Such insult may cause irreparable damage to the nerve, often left as a paresthesia or dysethesia of the gums, lip and chin. The condition may persist for life and may be accompanied by unconscious drooling.
In maxillary implants perforation of the maxillary sinus can cause implant failure as the implant may not get desired osseo-integration & may also land up in sinus.
Management-
Ideally the implant shall be atleast 1mm above the canal lining or sinus lining. Post surgically if the condition is diagnosed in short time from surgery (< 2 weeks) implant should be removed from the site & nerve should be relieved as soon as possible. Because when it is late then there is no scope for correction of nerve insult. Also to complete the treatment plan a new site is prepared and another implant is placed to restore the lost function.
(b) Infection (Figure-6)
The very basic cause of many of the problems and often overlooked by the dental surgeon is infection around the implant and this condition is termed as ‘Peri-Implantitis’. (Meffert) It is defined as an inflammatory reaction with the loss of supporting bone in the tissues surrounding a functioning implant.
 | Figure 6
 |
It happens because of following factors:-
a) Presence of microbes in the region
b) Poor oral hygiene
c) Poor asepsis protocol during the surgery
d) Smoking
a) Presence of microbes in the region
When the case selection is not appropriate and the patient suffers from periodontitis at the time of implant placement there is quite a probability that the microbes from the neighboring areas may move and get deposited on the implant surface and cause inflammation there. The microbes responsible are mostly Gram-negative rods, including Bacteroides, Fusobacterium subspecies, Actinobacillus actinomycetemcomitans, Prevotella and Porphyromonas species. (Becker et al).
b) Poor oral hygiene
Any food lodgment in the oral cavity for a prolonged period may initiate development of microbes in the oral cavity. This might trigger onset of periodontitis around remaining teeth and periimplantitis around the implants.
The patient has to be motivated to maintain the oral hygiene in a proper way by brushing and flossing and regular visit to the dental surgeon for oral prophylaxis.
c) Poor asepsis protocol during the surgery
The worst of all but still happening around in small dental offices is the poor asepsis control. When the surgical instruments are not cleaned and sterilized in a proper way there may be a very high probability of infection occurring in the surgical site right at the time of surgery which might lead to failure of implant. It’s not just the patient but also the operating dental surgeon who is at risk of getting blood borne infection and thus it is mandatory to have good sterilization practice in the dental office.
d) Smoking
When smoking is done the carbon gets deposited in the gingival tissue as well as around the implant thus causing non union with the bone.
Goreman et al found that implant failures were twice as common in smokers as in nonsmoker at second stage of surgery. In general, it can be concluded that smoking has a negative effect on implant survival, especially during the early healing period after implant installation.
Patients shall be advised not to smoke atleast from one week prior to surgery to 2 weeks after the prosthesis placement.
Management
Even after taking all the precautions yet at times there is occurrence of infection on the implant site. It is identified by the classical signs and symptoms of inflammation and should be treated immediately and thoroughly. The management of ‘periimplantitis’ involves three phases. The first phase involves the control of the acute infection and the reduction of inflammation. This involves the local removal of the plaque deposits with plastic instrument (implacare) and the polishing of all the accessible surfaces with pumice, the sub-gingival irrigation of all peri-implant pockets with 0.12% chlorhexidine; systemic antimicrobial therapy for 10 consecutive days; and improved patient compliance with oral hygiene by advising patient to start with -
Hot salt mouth washes,
Chlorhexidine mouthwash
They act directly on the implant site and help in eradication of infection. Also to combat the microbes under the soft tissue and in the bone regimen of systemic antibiotics is started.
Diode lasers can be used around the implant to irradicate bacteria & make the site sterile. Also if possible the implant shall be kept non functional or with reduced pressure on it during treatment of periimplantitis.
Treatment
When the drug therapy fails or when there is loss of bone from the implant site due to ongoing infection the dental surgeon is not left with much of the options. In such conditions it is advised for:-
Removal of Implant
Preparation of ‘Alternative Site’
The existing implant has to be removed and another site is chosen and prepared for the placement of a new implant. (Figure-7)
(c) Superstructure Fracture
As the superstructure of a fixed prosthesis is curved to fit the dental arch, it is subjected to twisting and bending movements. These result in fracture of the prosthesis as a result of overload or fatigue failure.
Space must be allowed for linear movements of two parts of the attachment under load. If this is not done then excessive force will be placed on the attachments.
Care has to be taken in case of cantilevers that their mesio-distal length does not increase more than 8 mm.
 | Figure 7
 |
(d) Implant Fracture (Figure-8)
A number of implants fracture at 3rd thread where the abutment screw ends and acts as a fulcrum at the inner diameter of threaded design.
 | Figure 8
 |
Another common site for fractures to occur is at junction of abutment and the screw owing to the thin diameter of the screw. Thus in a way it is the weakest point in the implant abutment system. To reduce the chances of fracture, friction lock abutment can be selected at the time of surgery.
High cantilever load is yet another good reason for an implant to fracture under moderate to heavy masticatory loads where the diagonally acting force passes through the weaker part of implant and leads to fatigue failure.
To prevent such a situation to occur it is advised to use flatter cuspal forms in the prosthesis rather than C-cusp which gives higher load on implant by ending up in centric interferences thus forming defects around the implant.
(e) Screw failure
The screw is said to be failed when there is
i) Repeated loosening
ii) Fracture of the screw
i) Repeated loosening
The reason for loosening of screw is excessive rotational force on the implant.
The threads of the screw don’t have any anti-rotation guide or lock and thus the unwanted back and forth movements do occur on mastication.
If the dental surgeon just tightens the screw and doesn’t look for the cause of loosening then this situation occurs again and again, ultimately leading to damage to the screw.
It the threads get damaged, the screw has to be replaced or the abutment may just come out and get disappeared leading to loss of prosthesis.
ii) Fracture of the screw
This can happen due to the following reasons:-
a) Damage to screw head
b) Excessive Overload
c) Poor adaptation of implant to the abutment
a) Damage to screw head
This happens when the screw is not positioned properly while being tightened and excessive force is applied to close the gap between implant and the screw head or if the screw driver slips out when tightening is being carried out.
It may also happen when there is frequent tightening of the screw in short span of time resulting in wearing out of the slot.
b) Excessive Overload
A situation not seen that very frequently but most of the time it happens in case of bruxers or people having heavy masticatory force. Any sudden force directed obliquely to the implant axis may cause fracture of the screw as it’s the weakest part of the system.
c) Poor adaptation of implant to the abutment
A typical situation arising when there is growth of gingival tissue in between the screw head and implant after the surgery thus creating a minute gap when the abutment is placed over. This gap breaks the union of abutment to implant by creating a weak spot.
When the patient bites there is not only impingement of soft tissue between screw and abutment but also slight movement of the abutment leading to fracture of the screw.
Management
To treat such a situation when there is repeated loosening of the screw, the first and most common thing a dental surgeon can do is:-
i) Removal of Screw and its replacement
This is merely the temporary solution or sort of immediate treatment what a dental surgeon can offer to the patient when the patient comes to the dentist for the first time. In case when there is repeated incidence of screw loosening one has to look for the underlying causes. In case where there has been damage to screw head, it may require immediate attention and has to be replaced on top priority.
If the screw fractures it becomes quite difficult to retrieve it and requires special skills for it.
The broken screw has to be loosened first by the help of ultrasonic instruments and then with the help of special pliers it is held and pulled out.
For the prosthesis removal pneumatic crown remover is preferred.
ii) Checking for overload on implant
One has to always look for the underlying pathology for the loosening or damage to the screw and very often it turns out to be overload on the implant.
The solution is to reduce the load by bringing the abutment in infra-occlusion and/or correction of the habits of patient which are causing the overload.
iii) Change in abutment & prosthesis design
In case of repeated loosening of abutment friction lock abutments can be used as well as screw retained prosthesis can be a choice of treatment.
Conclusion
To get high success rate and to escape from the humiliation of failing or troubling implants one should give proper attention to the patient information and procedural details taking in account all the possible problems which may occur once the implant has been placed.
To get the maximum benefits out, we shall see the end before we begin and for this one must have adequate training and knowledge of this highly specialized branch of dentistry. |