Introduction:
There is a high rate of success in retention of teeth by endodontic therapy. However, many teeth are not restorable because of apical resorption, fracture, incompletely formed roots or carious destruction of coronal structures. A novel approach to restore tooth structure is based on biology ie, regenerative endodontic procedures by the application of tissue engineering.[1]
The goal of Regenerative Dentistry is to induce biologic replacement of dental tissues and their supporting structures. The potential for regenerative dentistry is in large part due to advancements in biologic therapies that apply growth and differentiation factors which hasten or induce natural biologic regeneration. Most of the concepts have emerged from the growing fields of tissue engineering, which emphasizes the spatial assembly of distinct stem cells, growth factors and scaffolds to form a functional tissue or organ.[3] Regenerative medicine provides many advantages for restorative dentistry in terms of restoration survival rates and long-term treatment prognosis.[2]
Regenerative endodontic procedurescan be defined as biologically based procedures, designed to predictably replace damaged, diseased, or missing structures, including dentin and root structures as wellas cells of the pulp dentin complex with live viable tissues preferably of the same origin that restore the normal physiologic functions of the pulp dentin complex (Murray et al, 2007).
Although the challenges of introducing endodontic tissue engineering therapies are substantial, the potential benefits to patients and the profession are equally ground breaking. Patient demand is staggering both in scope and cost, because tissue engineering therapy offers the possibility of restoring natural function instead of surgical placement of an artificial prosthesis. Such translation will require the partnership of researchers and skilled clinicians who can effectively apply advances in knowledge to appropriate clinical cases and develop novel therapies which can be realistically introduced into the clinic.[2]
Before going in detail about regenerative endodontic procedures, we must have a brief knowledge about some factual procedures like:
Tissue Engineering:
Tissue engineering is an interdisciplinary field that integrates the principles of biology and engineering to develop biological substitutes that replace or regenerate human cells, tissue or organs in order to restore or establish normal function (9). There are three key elements for tissue engineering: stem cells, scaffolds and growth factors.
Stem cells : Stem cells are undifferentiated cells that continuously divide. There are two main types: embryonic, and adult or postnatal. Embryonic stem cells are capable of developing more than 200 cell types. In contrast, an adult stem cell can divide and create another cell like itself, and also a cell more differentiated than itself, but the capacity for differentiation into other cell types is limited. This is described as being “multipotent” and is a distinguishing feature of adult stem cells compared to the “pluripotent” or “omnipotent” properties seen in embryonic stem cells. Several types of adult stem cells have been isolated from teeth, as identified in the Table 1.[3]
Scaffolds:
Scaffolds provide support for cell organization, proliferation, differentiation and vascularization. Current REPs have utilized dentin as well as the blood clot[4] or platelet-rich plasma[5] to provide scaffolds in the root canal. However, many types of biodegradable or permanent scaffolds made of natural (collagen, hyaluronic acid, chitosan and chitin) or synthetic (polylactic acid, polyglycolic acid, tricalcium phosphate, hydroxyapatite) materials are available.[6] Recently, peptide hydrogel nanofibers and various fibrin gels have been investigated as potential scaffolds for dental pulp tissue engineering.
Growth Factors:
Growth factors are proteins that bind to receptors on the cell and act as signals to induce cellular proliferation and/or differentiation.[7] Examples of key growth factors in pulp and dentin formation include bone morphogenetic protein, transforming growth factor–beta and fibroblastic growth factor. Current REPs aim to utilize growth factors found in platelets and dentin.[8] Recent studies have shown that dentin contains a number of bioactive molecules that, when released, play an important role in regenerative procedures.
There can be potential methods for regenerative endodontic technology which are as following:
Potential technologies for regenerative endodontics:
Following are the areas of research that might have application in the development of regenerative endodontic techniques:
1. Root canal revascularization via blood clotting
2. Postnatal stem cell therapy
3. Pulp implantation
4. Scaffold implantation
5. Injectable scaffold delivery
6. Three – Dimensional cell printing
7. Gene therapy
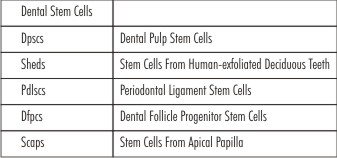 | Table 1
 |
Root canal revascularization via blood clotting:
Revascularization is the procedure to reestablish the vitality in a nonvital tooth to allow repair and regenerationof tissues.[9] Therationaleof revasculari zation is that if a sterile tissue matrix is provided in which new cells can grow, pulp vitality can be reestablished.[9] Several case reports have documented revascularization of necrotic root canal systems by disinfection followed by establishing bleeding into the canalsystem via overinstrumentation.[10] An important aspect of these cases is the use of intracanal irrigants (NaOCl and chlorhexdine) with placement of antibiotics (e.g. a mixture of ciprofloxacin, metronidazole, and minocycline paste) for several weeks. It disinfects and increases revasculari zation of avulsed and necrotic teeth.[11] Revascularization of necrotic pulps with fully formed (closed) apices might require instrumentation of the tooth apex to approximately 1 to 2mm in apical diameter to allow systemic bleeding into root canal systems.
The revascularization method assumes that the root canal space has been disinfected and that the formation of a blood clot yields a matrix (e.g., fibrin) that traps cells capable of initiating new tissue formation. It is not clear that the regenerated tissue's phenotype resembles dental pulp; however, case reports published to date do demonstrate continued root formation and the restoration of a positive response to thermal pulp testing. Another important point is that younger adult patients generally have a greater capacity for healing.[12]
There are several advantages to a revascularization approach. First, this approach is technically simple and can be completed using currently available instruments and medicaments without expensive biotechnology. Second, the regeneration of tissue in root canal systems by a patient's own blood cells avoids the possibility of immune rejection and pathogen transmission from replacing the pulp with a tissue engineered construct.
The case reports of a blood clot having the capacity to regenerate pulp tissue are exciting, but caution is required, because the source of the regenerated tissue has not been identified. Enlargement of the apical foramen is also necessary to promote vascularization and to maintain initial cell viability via nutrient diffusion. Cells must have an available supply of oxygen; therefore, it is likely that cells in the coronal portion of the root canal system either would not survive or would survive under hypoxic conditions.[13]
 |
 |
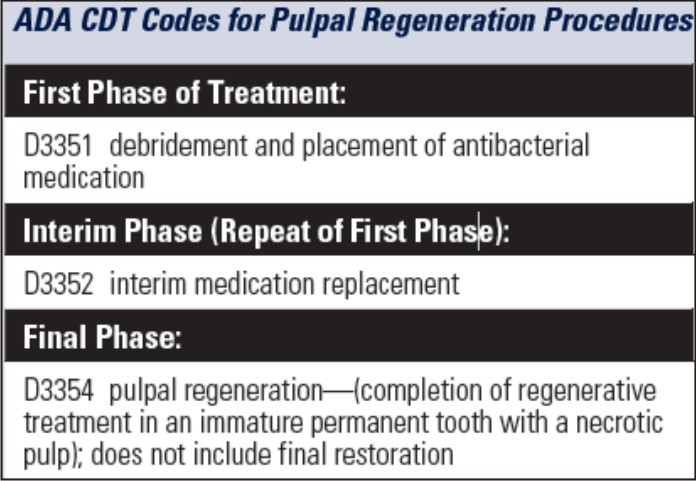
Fig 1:from left to right
a) Immature permanent teeth with open apex and periapical infection.
b) Access cavity is prepared.
c) Minimal or no instrumentation of canal.
d) Irrigation with 5.25% NaOCl and 0.12% chlorhexidine or 5.25% NaOCl and 3% H2O2 .
e) Triple antibiotic is placed in the canal.
f) Over instrumentation to induce bleeding into the canal
g) Stop bleeding 3mm below the CEJ
h) Follow up 6 months to 2 years show increased thickness dentinal wall and narrowing of pulp space
Post Natal Stem Cell Therapy: The simplest method to administer cells of appropriate regenerative potential is to inject them into disinfected root canal systems after the apex is opened.[7] Adult/postnatal stem cells are prime candidates for cell therapy.[14] Postnatal stem cells can be derived from multiple tissues, including skin, buccal mucosa, fat, and bone.[7] A major research obstacle for regenerative endodontics is the identification of a postnatal stem cell source capable of differentiating into the diverse cell population found in adult pulp (e.g., fibroblasts, endothelial cells, odontoblasts).[7]
Thereare several advantages to an approach using postnatal stem cells. First, autogenous stem cells are relatively easy to harvest and to deliver by syringe, and the cells have the potential to induce new pulp regeneration. Second, this approach is already used in regenerative medical applications, including bone marrow replacement, and a recent review has described several potential endodontic applications.
However, there are several disadvantages to a delivery method of injecting cells. First, the cells may have low survival rates. Second, the cells might migrate to different locations within the body, possibly leading to aberrant patterns of mineralization. A solution for this latter issue may be to apply the cells together with a fibrin clot or other scaffold material. This would help to position and maintain cell localization.
Pulp implantation: In pulp implantation, replacement pulp tissue is transplanted into cleaned and shaped root canal systems. The source of pulp tissue may be a purified pulp stem cell line that is disease or pathogen-free, or is created from cells taken from a biopsy, that has been grown in the laboratory.The cultured pulp tissue is grown in sheets in vitro on biodegradable membrane filters like polymer nanofibers or on sheets of extracellular matrix proteins such as collagen I or fibronectin. Membrane filters will be required to be rolled together to form a three-dimensional pulp tissue, which can be implanted into disinfected root canals.
The advantagesof this method are that the cells are relatively easy to grow on filters in the laboratory. Moreover, aggregated sheets of cells are more stable than dissociated cells administered by injection into empty root canal systems.
Thepotential problemsassociated with the implantation of sheets of cultured tissue is that specialized procedures may be required to ensure that the cells properly adhere to root canal walls. Another disadvantage of this technique is that implantation of sheets of cells may be technically difficult.
 | Figure 1
 |
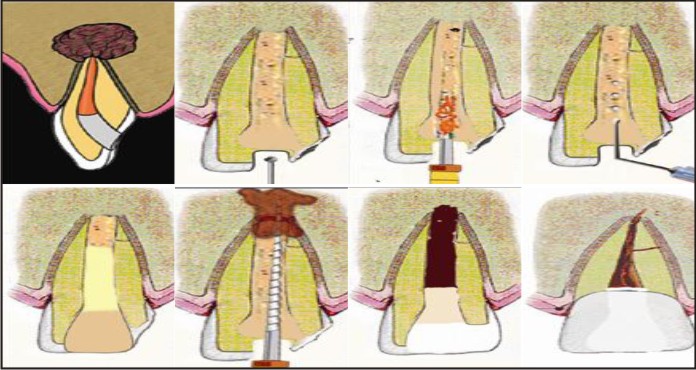
Fig 2 : Dentin-pulp complex formation with optimal orientation for clinical application of regenerative therapy. The pulp stem cells are transduced with BMP gene and attached to a defined scaffold to differentiate into odontoblasts. The tubular dentin-pulp complex can be transplanted on the exposed or amputated pulp in the cavity.
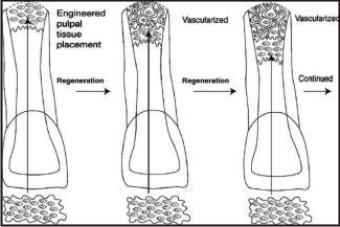
Scaffold Implantation
To create a more practical endodontic tissue engineering therapy, pulp stem cells must be organized into a three-dimensional structure that can support cell organization and vascularization. This can be accomplished using a porous polymer scaffold seeded with pulp stem cells. A scaffold should contain growth factors to aid stem cell proliferation and differentiation, leading to improved and faster tissue development..In pulp-exposed teeth, dentin chips have been found to stimulate reparative dentin bridge formation. Dentin chips may provide a matrix for pulp stem cell attachment and also be a reservoir of growth factors.The natural reparative activity of pulp stem cells in response to dentin chips provides some support for the use of scaffolds to regenerate the pulp-dentin complex.[7]
 | Figure 2
 |
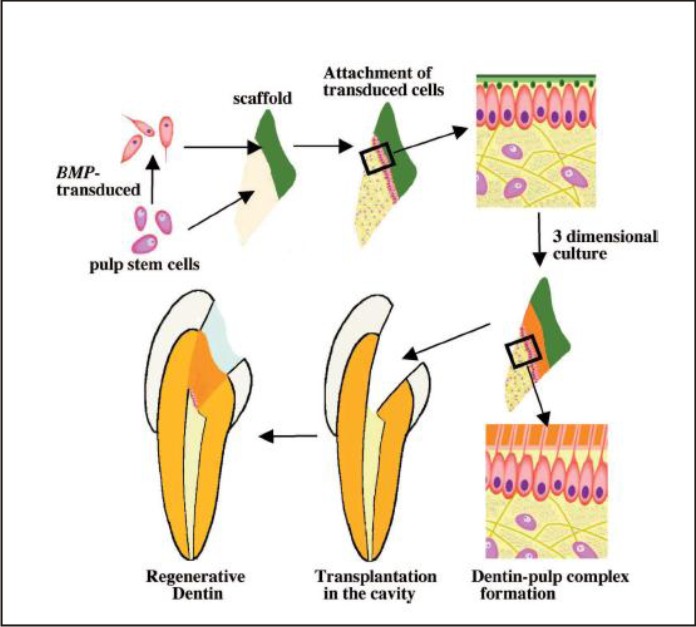
Fig 3: Engineered pulp Engineered pulp Engineered pulp installment Second Installment Third installment First layer
Injectable scaffold delivery
In root canal systems tissue engineered pulp tissue is administered in a soft three-dimensional scaffold matrix, such as a polymer hydrogel. Hydrogels are injectable scaffolds that can be delivered by syringe. Hydrogels have the potential to be noninvasive and easy to deliver into root canal systems.The hydrogel may promote pulp regeneration by providing a substrate for cell proliferation and differentiation into an organized tissue structure. Controlled release of growth factors is also possible by incorporating it into a gelatin hydrogel which gradually releases growth factor during in vivo biodegradation.Hydrogels at are at an early stage of research, and this type of delivery system, although promising, hasyet to be proven to be functional in vivo.
Three-Dimensional Cell Printing
The final approach for creating replacement pulp tissue may be to create it using a three-dimensional cell printing technique. Merely combining all three elements generates a tissue with haphazardly distributed cells and a questionable functional capacity. To overcome these deficiencies and in the hope of creating a more structured and functional tissue, an engineered three dimensional model is advocated. In theory, an ink-jet-like device is used to dispense layers of cells suspended in a hydrogel to recreate the structure of the tooth pulp tissue. The three- dimensional cell printing technique can be used to precisely position cells, and this method has the potential to create tissue constructs that mimic the natural tooth pulp tissue structure.Theoretically, the disadvantage of using the three-dimensional cell printing technique is that careful orientation of the pulp tissue construct according to its apical and coronal asymmetry would be required during placement into cleaned and shaped root canal systems.
Gene therapy
Gene therapy is recently used as a means of delivering genes for growth factors, morphogens, transcription factors, extracellular matrix molecules locally to somatic cells of individuals with a resulting therapeutic effect. The gene can stimulate or induce a natural biological process by expressing a molecule involved in regenerative response for the tissue of interest. Both anin vivoand anex vivoapproach can be used for gene therapy. In the in vivo approach, the gene is delivered systemically into the bloodstream or locally to target tissues by injection or inhalation.The ex vivo approach involves genetic manipulation of cells in vitro, which are subsequently transplanted to the regeneration site.
 | Figure 3
 |
Though regenerative endodontic procedures performed either in clinic or laboratory provide promising results but there are some stones in the path of success. So, here are some challenges that are associated with regenerative endodontic procedures
Challenges in regenerative endodontics
The possibility of pulp tissue regeneration is restricted by several factors, like, the dental pulp has minimal collateral blood supply, impairing the ability of the immune system to combat infections. Furthermore, odontoblasts are post-mitotic cells that have limited (or no) ability to proliferate. Thus, regenerating a functional pulp-dentin complex remains a challenge for the clinicians[15]. There are various barriers that have to be addressed in order to permit the introduction of regenerative endodontics.
These are:
1. Disinfection and shaping of the root canals in a fashion to permit regenerative endodontics.[7]
2. Creation of replacement pulp-dentin tissue.[7]
3. Delivery of replacement pulp-dentin tissues.[7]
4. Nerve and vascular regeneration.[14]
5. Ageing and regeneration.[17]
6. Measuring appropriate clinical outcomes.[7]
Disinfection
Attempts to regenerate pulp tissue under conditions of inflammation or partial necrosis have proven to be unsuccessful. In the presence of infection, the pulp stem cells that survive appear to be incapable of mineralization and deposition of tertiary dentin bridge. Furthermore it has been observed that pulp stem cells, periodontal stem cells, and fibroblasts do not adhere and grow in infected root canal systems. Disinfection of the root canal must be achieved by irrigation and the placement of an intracanal medicament.
The presence of a smear layer on root canal walls may inhibit the adherence of implanted pulp stem cells, potentially causing the regenerative endodontic treatment to fail. Improved methods to remove the smear layer from the root canal walls appear to be necessary to help promote the success of regenerative endodontics. Most commonly used agent for smear layer removal is a 17% solution of ethylenediaminetetraacetic acid (EDTA) that is applied as a final flush.
A variety of medicaments have been used by the clinicians to disinfect the root canal space. These include triple antibiotic paste (a 1:1:1 mixture of ciprofloxacin/ metronidazole / minocycline or variation thereof, Ca(OH)2 alone or incombination with antibiotics or formocresol.[16] The triple antibiotic paste could be a valuable adjunct for revascularization procedures, since it could be used to create an environment favorable for the in growth of vasculature and regenerative cells by reducing or eradicating bacteria in the canal space of teeth with necrotic pulps and incompletely formed apices.
Engineering A Functional Pulp Tissue
The success of regenerative endodontic therapy is dependent on the ability of researchers to create a technique that will allow clinicians to create a functional pulp tissue within cleaned and shaped root canal systems. The source of pulp tissue may be from root canal revascularization, stem cell therapy, involving the delivery of autologous or allogenic stem cells into root canals; or pulp implantation, involving the surgical implantation of synthetic pulp tissue grown in the laboratory. Each of these techniques to regenerate pulp tissue will have advantages and limitations that still have to be defined through basic science and clinical research.[7]
Concentration and composition of cells trapped in the fibrin clot during revascularization is unpredictable. The entire canal may get calcified thus increasing the difficulty in future endodontic treatment, if required. The type of the tissue that is formed is also not known. It has been suggested that bone-like, cementum-like or periodontal ligament like tissues may be formed in the pulp spaceafter revascularization.[16]
Delivery of replacement pulp-dentin tissues : Scaffoldused for pulp-dentin regeneration should take into account the challenges imposed by engineering a connective tissue within the confines of human dental root.Sterilization of scaffoldsis another challenge to be addressed. The biodegradable polymers pose some challenge to sterilization due to their low thermal transition temperatures (Tg and Tm), and their tendency to hydrate. The most commonly used sterilization techniques for biodegradable polymers utilize chemicals, heat, steam, radiation, or a combination thereof.
Some sterilization methods can significantly affect the mechanical and physical properties of biodegradable polymers due to depolymerization by chain scission, hydrolysis by water molecules, and shape changes by heat. In addition, sterilization procedures can leave harmful residues, causing less than optimal performance of the biodegradable materials in vivo and in vitro.
Challengesin nerve and vascular regeneration :
Nerve regeneration: Dental pulp is richly innervated. The main nerve supply enters the pulp through apical foramen along with the vascular elements. They include both sensory and sympathetic nerves. Pulpal nerves play a key role in regulation of blood flow, dentinal fluid flow, and pressure. The innervation of the pulp has a critical role in the homeostasis of the dental pulp. The pulpal nerve fibers contribute to angiogenesis, extravasation of immune cells and regulate inflammation to minimize initial damage, maintain pulp tissue, and strengthen pulpal defense mechanisms. The increasing interest in tissue engineering of tooth must take into account neuro-pulpal interactions and nerve regeneration.
The challenges include, but not limited to nociceptive mechanisms, altered thresholds to pain in inflamed teeth and dental pain. Thus, the life of teeth can be possibly prolonged by preservation of pulp and odontoblasts and promoting repair and regeneration by the study of neuropulpal interactions.
Vascular Regeneration : The vascular system in the dental pulp plays a role in nutrition and oxygen supply and as a conduit for removal of metabolic waste. The cellular elements of the blood vessels such as endothelial cells, pericytes, and associated cells contribute to pulpal homeostasis along with the nerves. Thus, the vascular contribution to regeneration of dentin pulp complex is immense.
The critical importance of vasculature in tissue repair and regeneration is well known. Vascular endothelial growth factor (VEGF) is an excellent regulator of angiogenesis and is known to increase vascular permeability. VEGF induced chemotaxis, proliferation and differentiation of human dental pulp cells. In addition human dentin matrix contains VEGF. The presence of VEGF in dentin and response of dental pulp cells to VEGF raises the possibility of the presence of endothelial progenitor cells in dental pulp alongside progenitors for odontoblasts and neuronal cells. In view of the role of endothelial progenitor cells in vascularization during tissue regeneration, it is likely VEGF and vascular endothelial cells are critical for dentin regeneration.[14]
Ageing And Regeneration : Histo morphometric analyses of pulpal cell populations indicate that age- related reductions in pulpal cell numbers occur. This includes sub-odontoblastic cells which may be a potential progenitor cell niche., the smaller the population of those cells able to participate, the less likely it is that novel clinical treatments will be effective in harnessing their potential to stimulate regeneration.
Measuring appropriate clinical outcomes : Once a tissue engineered pulp has been implanted, it is not ethical to remove functioning tissues to conduct a histological analysis. Therefore, it will not be possible to histologically investigate mineralizing odontoblastoid cell functioning or nerve innervation. Clinicians will have to rely on the noninvasive tests in use today, such as laser Doppler blood flowmetry in teeth; pulp testing involving heat, cold, and electricity; and lack of signs or symptoms.
Future of regenerative endodontics : The aspect of dentin-pulp tissue engineering is of great interest, with a large number of studies performed over the past several years. However, the science is still not able to allow clinical procedures to be performed routinely in animals or in humans.
The hope of research to date rests on the ability that the use of naturally occurring cells at the site of injury may lessen side-effect risks. Better understanding of the dentin-pulp complex biology will lead to an exciting era of the development of cell-based approaches. Therefore, there is a need for clinical specialties in dentistry to agree to a formula or creation of definitive standards that allow endodontists to successfully treat teeth or re-treat failures, allow prosthodontists to develop materials that prevent microleakage, and allow periodontists the ability to place implants when necessary.
The development of regenerative endodontics may make those other procedures not needed (extraction and implant replacement), especially with the expectation that both hard (dentin, enamel) and soft (innervated and vascularized dental pulp) tissues would become a normal and successful procedure.[16]
Conclusion
Tissue engineering using the triad of dental pulp stem cells, morphogens and scaffolds may provide an innovative and biologically based approach for generation of clinical materials and treatment of dental diseases. The challenges of introducing endodontic tissue engineered therapies are substantial; the potential benefits to patients and the profession are ground breaking. Better understanding of cell interactions and growth along with further research can make endodontic tissue engineering a reality in the near future.
References:
1. BS. Deepak, DB. Nandini, N. Sathyajith.Tissue Engineering : Is it the future of Endodontics?People’s Journal of Scientific Research 2011;4(1):76-82.
2. Simon SRJ, Berdal A, Cooper PR, Lumley PJ, Tomson PL, Smith AJ. Dentin-Pulp complex regeneration: from lab to clinic. Adv Dent Res 2011;23(3):340-45.
3. Langer R, Vacanti JP. Tissue engineering. Science 1993;260:920-6.
4. Banchs F, Trope M. Revascularization of immature permanent teeth with apical periodontitis: new treatment protocol? J Endod 2004;30:196-200.
5. Torabinejad M, Turman M. Revitalization of tooth with necrotic pulp and open apex by using platelet-rich plasma: a case report. J Endod 2011;37:265-8.
6. Chandrahasa S, Murray PE, Namerow KN. Proliferation of mature ex vivo human dental pulp using tissue engineering scaffolds. J Endod 2011;37:1236-9.
7. Murray PE, Garcia-Godoy F, Hargreaves KM. Regenerative endodontics: a review of current status and a call for action. J Endod 2007;33:377-90.
8. Ishimatsu H, Kitamura C, Morotomi T, et al. Formation of dentinal bridge on surface of regenerated dental pulp in dentin defects by controlled release of fibroblast growth factor-2 from gelatin hydrogels. J Endod 2009;35:858-65.
9. Shah N, Logani A, Bhaskar U, Aggarwal V. Efficacy of revascularization to induce apexification/apexogensis in infected, nonvital, immature teeth : A pilot clinical study. J Endod 2008;34:919-25.
10. B a n c h s F , T r o p e M . Revascularization of immature permanent teeth with apical periodontitis: new treatment protocol? J Endod 2004; 30: 196 -200.
11. Ritter AL, Ritter AV, Murrah V, Sigurdsson A. Trope M pulp revascularization of replanted immature dog teeth after treatment with minocycline and doxycycline assessed by laser Doppler flowmetry, radiography, and histology. Dent Traumatol 2004; 20: 75- 84.
12. Amler MH. The age factor in human extraction wound healing. J Oral Surg 1977; 35 :193-7.
13. Dewan RG, Kochhar R, Bhandari PP, Tyagi N.Regenerative Endodontics In The Light Of Recent Research 2013;5(2):132-135.
14. Nakashima M, Akamine A. The application of tissue engineering to regeneration of pulp and dentin in endodontics. J Endod 2005;31: 711
15. Demarco FF, Conde MCM, Cavalcanti BN, Casagrande L, Sakai VT, Nor JE. Dental pulp tissue engineering. Braz Dent J 2011;22(1):3-14.
16. Hargreaves KM, Cohen S. Cohen’s pathways of the pulp. 10th edition. Elsevier: Mosby;2011:452-503,602-619.
17. Sloan AJ, Waddington RJ. Dental pulp cells: what, where, how? Int J Paediatr Dent 2009;19:61-70.
|