Introduction
Oral leukoplakia is the most common premalignant lesion of the oral mucosa. WHO defines it as “A lesion which has a white patch or plaque on the oral mucosa that cannot be removed by scraping and cannot be classified clinically or microscopically as another disease entity”[1]. Various treatment procedures for oral leukoplakia have been reported i.e. excisional surgery, electroco agulation, cryosurgery, laser surgery and medication [2].
The use of lasers for treatment of intraoral pathologies has evolved over the last 4 decades as the clinical experience and scientific knowledge has increased since its inception. Laser wounds exhibit histological features that confer significant advantages over those created by scalpel and electrosurgery. Laser wounds have been found to contain lower number of myofibroblasts, resulting in minimal degree of wound contraction and scarring and allowing for improved postoperative function particularly in dynamic soft tissues such as tongue, floor of mouth and soft palate [3].
A case of oral leukoplakia characterized by raised plaque like, keratotic, non scrapable white lesion on dorsum of tongue has been described here that proved refractory to conventional therapy but was effectively treated with diode laser with no clinical evidence of recurrence.
Case Report
A 67 year old male patient reported to the Department of Periodontics with the chief complaint of non-scrapable, painless, non inflamed white patch on the dorsal surface of the tongue present for the last 6 months. The lesion had started as a peanut sized white patch and attained the present size of 2cm × 3 cm approximately 1 month back (Fig.1). Personal history of patient suggested that patient was non smoker and non alcoholic but was in the habit of chewing tobacco for the last 10 years. Medical history of the patient revealed him to be a controlled diabetic under medication. Patient was also asthmatic for last 30 years and was taking steroids in the form of inhaler 2-3 times a week since then. Patient was taking antioxidants (Lycopene) once daily and applying kenacort in orabase on the lesion twice daily for the past 1 month but didn’t get any relief. Routine blood investigations revealed no abnormality and all viral markers were negative ruling out the lesion to be oral hairy leukoplakia, one of the manifestations of HIV infection.
 | Fig 1 : Pre-operative
 |
As the white patch was a cause of great discomfort and cosmetic concern to the patient, an attempt was made to treat the lesion on the tongue with Diode laser. Routine protective measures were taken. All personnel wore laser safety glasses. The site of lesion was infiltrated with local anaesthetic (lignocaine 2% with adrenaline 1: 200000). A diode laser light source with a wavelength of 808 nm at 1.5 watt and continuous wave was used to excise the area of lesion extending 2mm beyond the visible margin of the white patch (Fig. 2). The healing process was uneventful with no pain, oedema, scar formation or dysfunction. Patient was kept on regular weekly follow up. At 1 month post operative, surgical area showed some recurrence at margins of operated site. Subsequently laser ablation was performed to clear the margins. During follow up after 2 months wound healing was found to be satisfactory with good granulation tissue formation and no signs of recurrence were seen. Follow up of patient after 3 months revealed complete remission with no signs of recurrence (Fig. 3).
 | Fig 2 : Intra-operative
 |
 | Fig 3 : 3rd Month Follow-up
 |
Histopathology of lesion revealed mild to moderate dysplastic changes in epithelium along with basilar cell hyperplasia, loss of polarity, hyperchromatism and pleomorphism (Fig. 4). After correlating clinical and histopathological findings diagnosis of leukoplakia was confirmed.
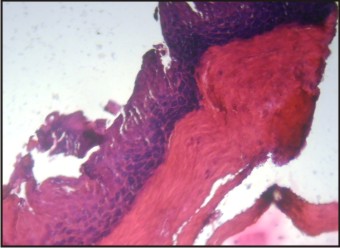 | Fig 4 : Histopathology
 |
Discussion
In 1978, laser surgery for oral leukoplakia was first performed by Ben Bassat [4]. Laser surgery for oral mucosal lesions has been reported to have many advantages and is widely used in the treatment of oral leukoplakia. It has a haemostatic effect which makes it easier to maintain the operative field[2]. It is also able to remove lesions accurately because unlike an electrotome it does not show electocontractility during the operation. The damage to adjacent tissues is minimal which reduces acute inflammatory reactions and post operative pain. Wound healing after laser surgery is excellent and does not produce any scar contracture and dysfunction [2].
It has been observed that non smoking related oral leukoplakia lesions are more frequent on tongue than smoking related lesions. These lesions also show epithelial dysplasia more frequently than lesions at other sites [5]. This case report is in confirmation to this fact as the lesion was present on dorsal surface of tongue in a non smoker and histopathologically showed mild to moderate dysplastic changes. The cause may be attributed to long term use of tobacco chewing in this case. The risk of malignant transformation varies directly with the duration of a lesion. Several additional reports have suggested that leukoplakia regardless of histologic grade may become malignant if left untreated for 36 months [6].
Diode lasers are used for soft tissue procedures only and their wavelength is well absorbed by pigmented lesions providing good hemostasis and effective cutting of tissues. Recurrence and/or malignant transformation of oral leukoplakia have occasionally been observed following laser surgery. It is reported that rate of recurrence was 7.7%-38.1% while malignant transformation was 2.6-9%[2]. The rate of recurrence has no association with the location or the epithelial dysplasia although it differed with the treatment procedures. The rate of recurrence in laser surgery was found to be approximately 29%[7]. Moreover an adequate resection margin may reduce the risk of recurrence[8].
Although laser wounds heal excellently and exhibit minimal scarring, they may take a longer time to heal as compared to scalpel wounds. It is also not uncommon for patients to exhibit increase in pain 4 to 7 days postoperatively[9].
Histologically, Oral epithelial dysplasia currently is the most important prognostic indicator for determining the malignant transformation risk of oral leukoplakia[10]. Laser excision is suitable for leukoplakia lesion on non keratinized epithelia i.e. the tongue and buccal mucosa while laser vaporization is suitable for gingival lesions. Laser excision not only prevents recurrence and malignant transformation but also postoperative dysfunction. In addition, postoperative oral fluid and nutritional intake is improved which decreases the potential need for hospitalization, thereby reducing the overall treatment cost.
Lesions with higher grade histology are generally believed to have a greater risk of malignant transformation. The ability to screen, diagnose, treat and monitor these lesions is imperative if we are to improve the morbidity and mortality from oral cancer.
References:
1. Kramer IR, Lucas RB, Pindborg JJ, Sobin LH. Definition of leukoplakia and related lesions: an aid to studies on oral precancer. Oral Surg Oral Med Oral Pathol. 1978 Oct; 46(4):518-39.
2. Ishii J, Fujita K, Komori T. Laser surgery as a treatment for oral leukoplakia. Oral Oncology 2003; 39: 759-69.
3. Zeinoun T, Nammour S, Dourov N, Aftimos G, Luomanen M,. Myofibroblasts in healing laser excision wounds. Lasers Surg Med 2001; 28(1): 74-9.
4. Cafaro A, Albanese G, Arduino PG, Mario C, Massolini G,Mozzati M, Broccoletti R. Effect of low-level laser irradiation on unresponsive oral lichen planus: early preliminary results in 13 patients. Photomed Laser Surg. 2010; 28(2): S99–S103.
5. Freitas MD, Blanco-Carrión A, Gándara-Vila P, Antúnez-López J, García-García A, Gándara Rey JM. Clinicopathologic aspects of oral leukoplakia in smokers and nonsmokers. Oral Surg Oral Med Oral Pathol Oral Radiol Endod. 2006 Aug; 102(2):199-203.
6. Lumerman H, Freedman P, Kerpel S: Oral epithelial dysplasia and the development of invasive squamous cell carcinoma. Oral Surg Oral Med Oral Pathol. 1995; 79: 321.
7. Ishii J, Fujita K, Munemoto S, Komori T. Management of oral leukoplakia by laser surgery: relation between recurrence and malignant transformation and clinicopathological features. J Clin Laser Med Surg. 2004 Feb; 22(1):27-33.
8. Kuribayashi Y, Tsushima F, Sato M, Morita K, Omura K. Recurrence patterns of oral leukoplakia after curative surgical resection: important factors that predict the risk of recurrence and malignancy. J Oral Pathol Med. 2012 Oct; 41(9):682-8.
9. Wlodawsky R. N, Strauss R. A. Intraoral laser surgery. Oral and Maxillofacial Surg Clin N Am. 2004; 16: 149-63
10. Wei Liu, Yu-Feng Wang, Hai-Wei Zhou, Peng Shi, Zeng-Tong Zhou, Guo-Yao Tang. Malignant transformation of oral leukoplakia: a retrospective cohort study of 218 Chinese patients. BMC Cancer 2010; 10: 685.
|