Introduction
Giant cell granuloma lesions (peripheral and central) are benign, non-odontogenic, moderately rare tumors of the oral cavity. They develop peripherally (within gingiva) or centrally (in bone).[1] These are classified under reactive gingival lesions which also include peripheral ossifying fibroma (POF), parulis, hemangioma and pyogenic granuloma. They resemble tumorous lesions and are usually localized to the gingiva (especially the interdental gingiva) or the alveolar mucosa.[2]
Peripheral giant cell granuloma (PGCG) is one of the most frequent giant cell lesions of the jaws and originates from the connective tissue of the periosteum or the periodontal membrane.[3] It is also known as giant cell epulis, giant cell reparative granuloma, osteoclastoma or giant cell hyperplasia.[4] It is not a true neoplasm but rather a benign hyperplastic reactive lesion.[3] It is often found to be associated with irritants such as plaque, calculus, poor dental restorations, ill-fitting dentures, trauma or tooth extraction; however, the etiology of PGCG is still not precisely known.[2]
PGCGs may present itself as polypoid or nodular lesions, predominantly bluish red with a smooth shiny or mamillated surface. They are variable in size and are generally soft or rubbery to touch. They are basically asymptomatic, unless they interfere with occlusion, in which case they may ulcerate and become infected. They are more frequent in women than in men, with a slightly higher prevalence in the 30- to 70-year-old age group. The predominant sites to be affected are premolar and molar regions of the mandible. Histologically, it is characterized by the presence of multinucleate giant cells in a stroma showing varying degrees of inflammation and vascularization.[5]
Case Report
A 10 year old male patient reported to the Department of Oral Medicine & Radiology with the chief complaint of swelling in the left lower back teeth region since one month. The swelling started gradually and was smaller in size which later grew to attain the present size. Intraoral examination revealed a single well defined swelling in relation to 34 to 36 region extending superioinferiorly from marginal gingiva to buccal vestibule measuring approximately 2 x 2.5 cm in size, slightly oval in shape, pale pink in color with few erythematous areas. Buccal vestibule was not obliterated and 35 was displaced lingually (Fig 1). On palpation, the swelling was well demarcated, firm in consistency and non-tender.
 | Fig 1:- Intraoral Photograph Showing Well Defined Swelling In The Left Lower Posterior Teeth Region
 |
On the basis of history and clinical examination, a provisional diagnosis of peripheral giant cell granuloma was made. Considering a favorable prognosis, the entire lesion was excised under local anesthesia and sent for histopathological examination. Grossly, the specimen measured about 2.5 cm x 2 cm in size, irregular in shape, soft to firm in consistency and pinkish in color.
Microscopically, the haematoxylin and eosin stained sections revealed hyperparakeratinized epithelium overlying connective tissue stroma (Fig 2). The highly cellular connective tissue stroma showed the presence of dense collagenous matrix, numerous blood vessels and multinucleated giant cells (Fig 3). Presence of chronic inflammatory infiltrate was also evident. Evidence of recurrence was not observed even after six months of follow up after treatment.
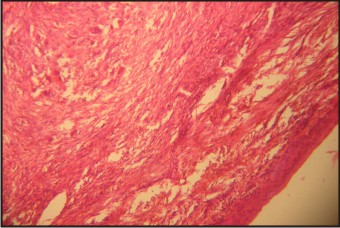 | Fig 2:- Photomicrograph Showing Hyperparakeratinized Epithelium Overlying Connective Tissue Stroma
 |
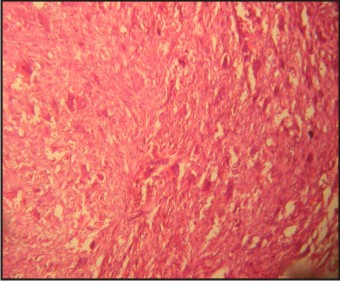 | Fig 3:- Photomicrograph Showing Dense Collagenous Connective Tissue Matrix, With Numerous Blood Vessels And Multinucleated Giant Cells
 |
Discussion
Giant cell granuloma as (peripheral and central) is benign, non odontogenic, moderately rare tumors of the oral cavity. PGCG is a relatively frequent benign reactive lesion of the oral cavity, originating from the periosteum or periodontal membrane following local irritation or chronic trauma.[6] They are seen in the young as well as in the elderly population with highest incidence in the 4th and 6th decades of life, however, 20-30% of cases manifest in the 1st and 2nd decades of life.[7] It is more common among females (60%) predominantly affecting the mandible.[8] PGCG arise interdentally or from the gingival margin, occur most frequently on the labial surface, and may be sessile or pedunculated. They vary in appearance from smooth, regularly outlined masses to irregularly shaped, multilobulated protuberances with surface indentations. There are no pathognomic clinical features whereby these lesions can be differentiated from other forms of gingival enlargement.[6] Histologically, PGCG is identified as a non-encapsulated mass of tissue compiled of a reticular and fibrillar connective tissue stroma containing plump, ovoid and fusiform fibroblasts and multinucleated giant cells.[1] The giant cells may contain only a few nuclei or upto several dozen of them. Nuclear pleomorphism may vary from large, vesicular to small, pyknotic nuclei. The origin of giant cells is unknown. Ultrastructural and immunological studies have shown that giant cells are derived from osteoclasts.[8]
The fibrocellular reaction is akin to that of other reactive lesions such as fibrous hyperplasia and peripheral ossifying fibroma. The calcified material or newly formed bone may also be seen all over the cellular connective tissue, and some of the lesions may be either woven bone or lamellar bone produced by the mononuclear stromal cells, which might be similar to latent proliferative osteoblasts or osteoprogenitor cells.[1] The differential diagnosis of PGCG includes pyogenic granuloma, fibrous epulis, peripheral ossifying fibroma and papilloma all of which present with similar clinical and radiographic findings. Thus, in such cases a definitive diagnosis can be established through histopathological examination.
The treatment of PGCG comprises surgical resection with elimination of the entire base of the lesion and suppression of the etiologic factor. If resection is only superficial, the growth may recur. Most lesions respond satisfactorily to thorough surgical resection, with exposure of all the bone walls. When the periodontal membrane is affected, extraction of the adjacent teeth may prove necessary to ensure full resection though this is initially contraindicated.[3] The reported recurrence rate of PGCG being about 10-15%, close follow-up is recommended.[4]
Early detection and treatment of gingival lesions is important to reduce bone loss or displacement of teeth. Hence, precise diagnosis of PGCG on the basis of clinical, radiological and histopathological examinations, allows conservative management with a less risk of damage to teeth and adjacent bone.
References
1. Etoz OA, Demirbas AE, Bulbul M, Akay E. The peripheral giant cell granuloma in edentulous patients: report of three unique cases. Eur J Dent (2010), 4: 329-333.
2. Ozalp N, Sener E, Songur T. Peripheral giant cell granuloma and peripheral ossifying fibroma in children: two case reports. Med Princ Pract (2010), 19: 159-162.
3. Shadman N, Ebrahimi SF, Jafari S, Eslami M. Peripheral giant cell granuloma: a review of 123 cases. Dent Res J (2009), 6(1): 47-50.
4. Mannem S, Chava VK. Management of an unusual peripheral giant cell granuloma: a diagnostic tool. Contemp Clin Dent (2012), 3(1): 93-96.
5. Rey JMG, Carneiro JLPM, Vila PG, Carrion AB, Garcia AG, Grana PM et al. Peripheral giant cell granuloma. Review of 13 cases. Medicina Oral (2002), 7: 254-9.
6. Ozcan E, Bodur S, Erdem G. Peripheral giant cell granuloma- a case report. Pakistan Oral & Dental Journal (2011), 31(1): 171-172.
7. Adlakha VK, Chandna P, Rehani U, Rana V, Malik P. Peripheral giant cell granuloma. J Ind Soc Pedo Prev Dent (2010), 28(4): 293-296.
8. Tandon PN, Gupta SK, Gupta DS, Jurel SK, Saraswat A. Peripheral giant cell granuloma. Contemp Clin Dent (2012), 3(1): S118-S121.
|