Introduction
Oral cancer represents 2%–5% of all cancers, being one of the 10 most frequent ones.[1] Although its incidence is lower than for other types of cancer, it is a major poblational health problem because of its mortality and severe morbidity.[2],[3],[4],[5],[6] Apart from oral cancer risk factors already described in literature, such as tobacco and alcohol consumption, others emerging risk factors, such as chronic irritation from dental factors has been proposed.[7],[8]
Chronic trauma of the oral mucosa (CTOM) is the result of repeated mechanical irritative action of an intraoral injury agent. Defective teeth (malpositioned or with sharp or rough surfaces because of decay or fractures), ill-fitting dentures (sharp or rough surfaces, lack of retention, stability or overextended flanges) and/or Para functional habits (e.g. oral mucosa biting or sucking, tongue interposition or thrusting), acting individually or together, could all be responsible of this mechanical irritation.[9] CTOM could generate lesions on a healthy mucosa or intensify previous oral diseases.[10]
In this article, we report cases of squamous cell carcinoma of tongue with chronic trauma as precipitating factor.
Case Report 1
A 67 year old female patient visited the department of oral medicine and radiology with chief complaint of pain and ulcer at the posterior lateral border of the tongue for last 4 months. The patient was a non-smoker and did not consume alcohol. Patient gave history of ulcer due to trauma to tongue from teeth while chewing food 4 months back. Patient claimed that the ulcer did not heal after the trauma and persisted. Pain was severe , radiating and decreased on medication. Medical history of patient revealed her to be an epileptic and hypertensive. On Intraoral examination, a well-defined ulcerative lesion 2 × 2.1 cm in size was seen on right posterior lateral border of tongue with respect to 47 and 48. The margins of ulcer were irregular and indurated. Sharp cusps were observed in relation to right maxillary and mandibular 3rd molars causing obvious trauma in the area [Figure 1].
 | Figure 1
 |
Based on history and clinical findings provisional diagnosis of traumatic ulcer was given. Biopsy of lesion was done for diagnosis and to rule out dysplastic changes.
Case Report 2
A 40 year old female patient visited the department of oral medicine and radiology with chief complaint of pain and ulcer at the left posterior lateral border of the tongue for last 5 months. The patient was a non-smoker and did not consume alcohol. Patient gave history of constant trauma to tongue from teeth since 5 months. She gave history of extraction of 37 one month back. Medical history of patient was non relevant.
On Intraoral examination, a well-defined ulcerative lesion 4× 2.5 cm in size was seen on right posterior lateral border of tongue with respect to 47 and 48. The margins of ulcer were raised, irregular and indurated. The floor of ulcer was erythematous and white patch surrounding the ulcer was seen [Figure 2]. Tooth 37 was missing. Provisional diagnosis of traumatic ulcer was given. Biopsy of lesion was done for diagnosis.
 | Figure 2
 |
Case Report 3
A 40 year old male patient visited the department of oral medicine and radiology with chief complaint of pain and ulcer at the left posterior lateral border of the tongue for last 2 months. The patient was a non-smoker and did not consume alcohol. Patient gave history of constant trauma to tongue from teeth since 2 months. Medical history of patient was non relevant .On Intraoral examination, a well-defined ulcerative lesion 2× 1.5 cm in size was seen on left posterior lateral border of tongue with respect to 36 and 37 [Figure 3]. On the basis of history and clinical examination provisional diagnosis of traumatic ulcer was given. Biopsy was advised to rule out dysplastic changes.
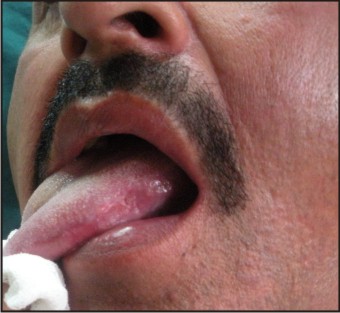 | Figure 3
 |
Histopathologicreportwas moderately differentiated squamous cellcarcinoma in Case 1 and Case 3 and well differentiated squamous cell carcinoma in case 2.
All the patients were referred to cancer institute for further treatment.
Discussion
More than 90% of all oral malignancies are squamous cell carcinomas.[11] SCC of the tongue is seen most frequently (27.6%), followed by cancer of the oropharynx (22.8%), lip (16.5%), floor of the mouth (14%), gingival (9.1%) hard palate (4.1%), and buccal mucosa (3.5%) in a report covering the years between 1983 and 1993 in America.[11] National Cancer Institute. Surveillance epidemiology and end results program (SEER), 1983–1993.[12] The most common site of intraoral carcinoma involvement is the tongue, usually the posterior lateral and ventral surfaces.[7] In our three patient, SSC of posterior lateral border of the tongue was diagnosed.
As with so many carcinomas, the risk of intraoral cancer increases with increasing age, especially for males. In the past, the prevalence was much higher in males, but the male to female ratio has dramatically decreased in recent years to approximately 2:1 because of the increased number of female who smoke.
Early lesions are often asymptomatic and slow-growing. As the lesion develops, the borders become diffuse and ragged, and induration and fixation ensue. If the mucosal surface becomes ulcerated, the most frequent oral symptom is that of a persistent sore or irritation. Not uncommonly, patients may report numbness or a burning sensation, swelling, or difficulty in speaking or swallowing. Lesions can extend to several centimetres in diameter if treatment is delayed; this delay permits large lesions to invade and destroy vital osseous structures. Persons with oral squamous cell carcinoma are most often older men who are aware of an alteration in oral cancer site for 4–8 months before seeking professional help. There is minimal pain during the early growth phase, and this may explain the delay in seeking professional care.[7] Likewise, the patient had applied to the clinic, after having five - six month lesions. It is generally recognized that the diagnosis of SSC of the oral cavity is not difficult when the patient complains of intraoral pain and dysfunction.[13] Dentists have the best opportunity to discover early lesions of the oral cavity. It is their responsibility to examine the oral cavity carefully and to refer the patient with suspicious lesions for proper evaluation and possibly biopsy.[14] The lesions in the case reports were initially described by the patients as a dental trauma but were proven to be SCC on histopathologic evaluation.
The causative role of CTOM on oral carcinogenesis is controversial. Some authors proposed it as a cause or oral cancer; on the other hand, others suggest it is a result of the increase in volume of the tumor [7].
Lockhart did not have statistically significant results for association between oral cancer and dental factors, including tooth loss, defective teeth and denture use.[15]
Velly and Rosenquist studies establish a relationship between denture as a traumatic factor and oral cancer. Rosenquist work also establishes an association between defective teeth and oral cancer risk, even though it does not specify the criteria to determine defective teeth.
Furthermore, experimental studies on hamsters showed that CTOM produced ulcerated lesions in a similar way to a chronic traumatic ulcer in humans. These lesions also determine several consequences: site of appearance of the malignant tumor, an increase in frequency, higher malignancy grade and shortening of latency period.
The mechanism by which CTOM is thought to contribute to carcinogenesis is not clearly identified. It has been proposed that the wound of the oral mucosa may facilitate the absorption of other chemical carcinogens.[16] Experimental studies of CTOM in animals together with evidence of inflammation related cancers, suggest that CTOM could work by at least other two mechanisms. One consists in the mitosis increase produced to repair tissue injury, which put cells at risk of DNA damage by other agents, initiating carcinogenesis[17]. The other mechanism possibly involved could be because of the chronic inflammation which happens in the site affected by CTOM, through release of chemical mediators and/or oxidative stress . This could induce genetic and epigenetic changes, damage DNA, inhibiting its repair, altering transcription factors, preventing apoptosis and stimulating angiogenesis; therefore, it could contribute in all stages of carcinogenesis.[18]
In the present report, all the patients did not report of any deleterious habits. Past medical history and family history were not significant. The elucidating factor in this patient was the history of chronic trauma due to sharp edges of the molars which may be considered as one of the possible mechanism of her tongue cancer. Chronic mechanical trauma due to sharp remaining teeth, less than ideal fillings, badly fitting dentures or unsuitable denture-bearing tissue, and loose anchoring attachments in the etiology of oral squamous cell carcinoma has been reported in literature.[7] In this regard Monkman et al carried out a review of the literature relating cancer to trauma and found no evidence to suggest that single uncomplicated trauma can cause cancer. However they concluded that trauma in combination with other factors may act as a co-carcinogen and that there was adequate evidence suggesting that metastatic spread of malignant tumour can be affected by trauma.[19]
Consequently, early recognition of this entity as well as a multidisciplinary management may help in the prognosis of these cases. The dentists should have adequate knowledge about the disease with regard to the patients who visit the dentist first
References
1. Parkin DM, Pisani P, Ferlay J. Estimates of the worldwide incidence of 25 major cancers in 1990. Int J Cancer 1999; 80: 827–41.
2. La Vecchia C, Tavani A, Franceschi S, Levi F, Corrao G, Negri E. Epidemiology and prevention of oral cancer. Oral Oncol 1997; 33: 302–12.
3. Morelatto RA, López de Blanc SA. Oral cancer mortality in the province of Cordoba, Argentine Republic in the period 1975–2000. A comparative study with other populations. Med Oral Patol Oral Cir Bucal 2006; 11: E230–5.
4. Barasch A, Safford M, Eisenberg E. Oral cancer and oral effects of anticancer therapy. Mt Sinai J Med 1998; 65: 370–7.
5. Gaziano JE. Evaluation and management of oropharyngeal Dysphagia in head and neck cancer. Cancer Control 2002; 9: 400–9.
6. Allison PJ, Locker D, Wood-Dauphinee S, Black M, Feine JS. Correlates of health-related quality of life in upper aerodigestive tract cancer patients. Qual Life Res 1998; 7: 713–22.
7. Thumfart W, Weidenbecher M, Waller G, Pesch HJ. Chronic mechanical trauma in the aetiology of oropharyngeal carcinoma. J Maxillofac Surg 1978; 6: 217–21.
8. Warnakulasuriya S. Causes of oral cancer-an appraisal of controversies. Br Dent J 2009; 207: 471–5.
9. Grinspan D. Enfermedades de la boca. Buenos Aires: Editorial Mundi, 1973; 792–823.
10. Lanfranchi HE. Estomatologia y PTR. In: Alvarez CantoniH, FassinaNA, eds. Prótesis total removible: Fundamentos, técnicas y clínica en rehabilitación bucal, Tomo 2, 1 edn. Buenos Aires: Hacheace, 2002; 395–449.
11. B. Neville, Oral and maxillofacial pathology (1st ed.), WB Saunders Co, Philadelphia (1995) p. 295–304.
12. National Cancer Institute. Surveillance epidemiology and end results program (SEER), 1983–1993.
13. A. Mashberg, J. Morrissey and L. Garfinkel, A study of the appearance of early asymptomatic oral squamous cell carcinoma, Cancer 32(1973) (1–6), pp. 1436–1445.
14. J. Rosai, Ackermans surgical pathology (8th ed.), Mosby Co, Philadelphia (1989) p. 223–57.
15. Lockhart PB, Norris CM Jr, Pulliam C. Dental factors in the genesis of squamous cell carcinoma of the oral cavity. Oral Oncol1998; 34: 133–9.
16. Dayal RR, Anuradha BK. Malignant potential of oral submucous fibrosis due to intraoral trauma. Indian J Med Sci2000; 54: 182–7.
17. Perez MA, Raimondi AR, Itoiz ME. An experimental model to demonstrate the carcinogenic action of oral chronic traumatic ulcer. J Oral Pathol Med2005; 34: 17–22.
18. Eduardo David Piemonte, Jerónimo Pablo Lazos, Mabel Brunotto. Relationship between chronic trauma of the oral mucosa, oral potentially malignant disorders and oral cancer. Journal of Oral Pathology & Medicine 2010; 39, 7: 513–517.
19. Randhawa T, Shameena PM, Sudha S,NairRG. Squamous cell carcinoma of tongue in a 19-year-old female. Indian Journal of Cancer. July–September 2008 ; 45 : 3.
|