Background:
The maxillofacial region is affected by a greater number of cysts than any other part of the body.In 1956, Philipsen separated seven jaw cysts from cholesteatomas occurring in other cranial areas. Because he thought that these were odontogenic cysts and not of inflammatory origin, he coined the term odontogenic keratocyst (OKC)[1] odontogenic keratocyst also known as primordial cystare benign, but locally aggressive, it is generally accepted that they arise from the remnants of the dental lamina which persist in sub-epithelial tissues including bone after the completion of odontogenesis. Usually seen in the jaws, with a predilection for the posterior body and ascending ramus (69% - 83%)of the mandible.[2] OKC represents approximately 4% of all odontogenic cysts. Gorlin-Goltz Syndrome is associated with 5% of these cases. These are more commonly seen in the 2nd and 3rd decades of life and males are more frequently affected than females in the ratio of 2:1. Histologically, the parakeratinized OKC’s have higher recurrence rate as compared to the orthokeratinized OKC’s[3] In 2005, the W.H.O working group considered the parakeratinized variant to be a cystic neoplasm and recommended the descriptive term Keratocystic Odontogenic Tumour[4] The orthokeratinized version is not considered as a tumour.
Clinical Presentation
KCOTs are often asymptomatic and only become clinically evident after bony expansion or a secondary infection has occurred; unlike most other jaw cysts which expand by osmotic pressure, the KCOT expands due to increased epithelial turnover and bony expansion is not a common finding. These are discovered accidentally on radiographs. Radiographically they can be seen as unilocular or multilocular radiolucencies.
When they do cause symptoms these can be in the form of pain, swelling and discharge, often as a result of secondary infection. The majority (over 70%) occur in the mandible and half of all KCOTs occur at the angle of the mandible[5]. Maxillary KCOT’s tend to be diagnosed early as they are more likely to get infected. Bony expansion may be seen in 60% of the cases[3]. One of the clinical features of the KCOTs that cause difficulty in management is their tendency to recur after treatment. Reported rates of recurrence range from 3% to 60%[5].
It has been suggested that recurrences might develop in three different ways: Incomplete removal of the original cyst lining; retention of micro cysts or epithelial islands in the wall of the original cyst; development of new keratocysts from epithelial offshoots of the basal layer of the oral epithelium[6],[7].
Many theories have been proposed to account for the high level of recurrence of these lesions. Firstly, the cyst lining is delicate and remnants can be left behind after surgical removal, satellite cysts (from odontogenic epithelial residues) or daughter cysts (from out pouching’s of the main cyst lining), scalloped margins, multilocular variety, and its location causing difficult access adds to the difficulty in removing the cyst in toto[3] may develop into new cysts after removal.
The treatment of most KCOTs is surgical enucleation (to remove the lesion whole from within the bone). For larger cysts, some surgeons undertake marsupiali sation often later followed by enucleation. However, in relation to the KCOT, due to the lining of the cyst often being delicate and the fact that they frequently recur, this method alone is not sufficient. Adjunctive surgical treatment has been proposed in addition to the surgical enucleation, such as removal of the peripheral bone (ostectomy) or resection of the cyst with surrounding bone (en-bloc) resection[8]. The latter would seem somewhat radical since significant reconstruction might be required for large lesions. Other adjunctive treatments have been proposed most notably cryotherapy (freezing) with liquid nitrogen[9] and the use of the fixative Carnoy’s solution[10] placed in the cyst cavity after enucleation; both of which attempt to address residual tissue to prevent recurrence.
Still, KCOT poses a diagnostic and therapeutic challenge as reflected by the numerous papers that have appeared since the recognition of this lesion as a separate entity.
In this paper, we are discussing two cases of a KCOT, which was located in anterior portion of maxilla involving maxillary sinus, which shows both the buccal and the palatal bone enlargement. Both cysts were treated by Electro-cauterization as adjunctive therapy along with enucleation.
Case Description:
Case 1
An 18-year old male patient was referred to the Department of Oral and Maxillofacial Surgery, complaining of intermittent pain and swelling of the right cheek. History revealed that he has been having these complaints for two months,for which he was prescribed antibiotics by a general practitioner. Extra-oral examination revealed a diffused swelling, extends antero - posteriorly from ala of nose to a vertical line 2cm posterior to angle of mouth supero - inferiorly from 1cm above the alar tragus line to a line joining angle of mouth to lobule of ear. Swelling is tender and firm in consistency. Skin overlying the lesion was normal with slight elevation in temperature. The right nasolabial fold is obliterated. Intra orally, the swelling extended from right cuspid to first molar with palatal extension up to midline. Obliteration of the upper buccal vestibule was observed with blanching of over lying mucosa. Swelling was compressible in the centre and borders were diffused. Examination of the teeth showed that all the permanent teeth were present, with impacted third molars. Right cuspid, bicuspid and first molar were nonvital on both thermal and electric pulpal testing. (Fig 1)
 | Fig 1. : Intraoral Photograph Showing Buccal And Palatal Expansion.
 |
A series of radiographs of face and skull including paranasal sinuses were taken. Occlusal radiograph of upper jaw showed bilamellar expansion of right half of the maxilla in relation to cuspid and bicuspids, also extension of the lesion was seen on the palatal side up to midline. Orthopantomogram showed a unilocular circumscribed radiolucency that extended from the right central incisor to the first molar of the same side, Superiorly involving maxillary sinus. The floor of the left nostril was displaced superiorly and medially. Both bicuspids roots were diverged. Subsequently, computerized tomography (CT) scans of the maxilla shows well defined radiolucency between the bicuspids causing the displacement of roots and extending from midline up to the first molar. The involvement of maxillary antrum, perforation of buccal, palatal cortical plate, antero posterior wall of sinus, lateral wall of nose was noticed.(Fig 2)
 | Fig 2. : Ct Of The Lesion.
 |
Aspiration of the lesion revealed yellow colored fluid with cholesterol crystals. H & E stained smear showed the presence of keratin squames in cluster, suggestive of infected KCOT.(Fig 3)
 | Fig 3. : Yellow Aspirated Material Showing Cholesterol Crystals.
 |
Histologically, hematoxylin and eosin stained section showed uniform 4-6 cell thick parakeratinised stratified squamous epithelial lining and fibrous connective tissue wall. The epithelium connective tissue interface was flat. The luminal surface showed parakeratotic epithelium, which exhibited a corrugative tissue with parallel bundles of collagen fibers, fibroblasts, blood vessels and areas of extravasated RBCs, suggestive of KCOT. (Fig 4)
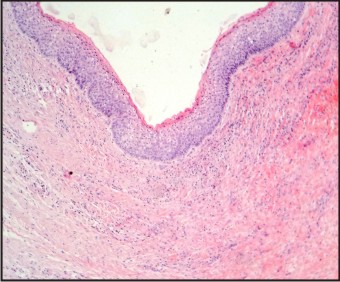 | Fig 4. : Histology
 |
Case 2
A 12 year old female patient reported to the outpatient department with the compliant of swelling in the left side of face since three months which was increasing in size. On examination a diffuse swelling, with nasolabial fold obliteration. Intraorally, right lateral incisor and canine were missing in the arch with retained deciduous canine. Obliteration of buccal vestibule was evident with palatal swelling extending till the midline mucosa was normal.(Fig 5) Palpation revealed both labial and palatal cortical plates were perforated. Ortho pentamogram showed impacted 12 and 13 with radiolucent area which was involving the maxillary sinus.(Fig 6) CT showed there was evidence of lobulated predominantly lytic expansile lesion (CT value of 7-19 HU) of size 4.24 cm mediolaterely, 4.7 cm anterioposteriorly and 8 cm superioinferiorly. There was thining of its wall with break in both inner and outer cortex. The lesion was extending superiorly to involve almost whole of right maxillary sinus causing expansion and thinning of its walls. Mass was extending medially in to nasal cavity. Posteriorly mass was reaching up to root of pterygoid plates however plates were normal. No areas of calcification was evident within the lesion.(Fig 7).
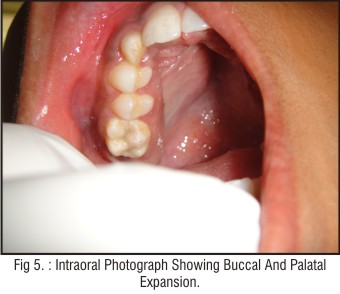 | Fig 5. : Intraoral Photograph Showing Buccal And Palatal Expansion.
 |
 | Fig 6. : Opg, Showing Involvement Of Maxillary Sinus And Impacted Tooth.
 |
 | Fig 7. : Ct Of The Lesion.
 |
Aspiration of the lesion revealed yellow coloured fluid with cholesterol crystals. H & E stained smear showed the presence of keratin squames in cluster, suggestive of keratinized cyst.
Treatment
Both the cases were treated with Enucleation of the lesion and electro-cauterization. Under general anesthesia,a crevicular incision extending from right central incisor to second molar on right side with two vertical realising incisions were given and mucoperiosteal flap elevated. The flap elevation showed a cystic lesion with a bony perforation in the buccal cortical plate as a part of anterior and lateral wall of maxillary antrum was eroded and thinned out by the cyst. The lesion was well encapsulated and contained cheesy keratinous material. After enucleation of the cyst, inspection of the defect showed that the maxillary roof and floor were intact. Electrocautery tip was moved all over the defect to make sure the remaining epithelial lining was cauterised. Defect was irrigated and complete haemostasis achieved before primary closer of the wound done with 3-0 silk.(Fig 8, 9, 10).
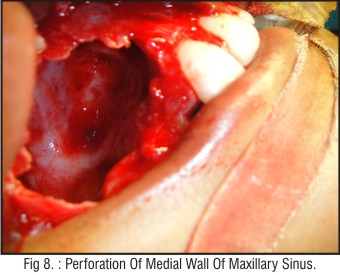 | Fig 8. : Perforation Of Medial Wall Of Maxillary Sinus.
 |
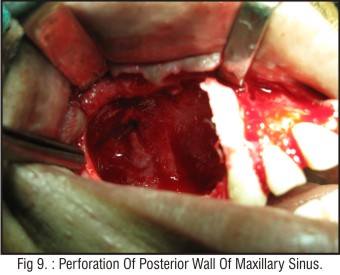 | Fig 9. : Perforation Of Posterior Wall Of Maxillary Sinus.
 |
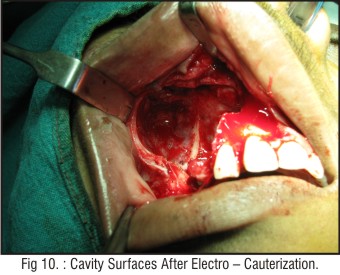 | Fig 10. : Cavity Surfaces After Electro – Cauterization.
 |
Treatment Followed For
Both cases were followed for three years, with no sign of recurrence, both clinically and radiological till date.
Discussion:
The treatment of the KCOT remains controversial. There are pros & cons for all the treatment options. The main goal is to eradicate the lesion with whatever means that might be applicable to the particular lesion according to the site, size & location.
The most characteristic clinical aspect of KCOTs is the high frequency of recurrence. The mechanism of recurrence is thought to be related to residues of cyst epithelium and an intrinsic growth potential following excision. Reported recurrence rates vary from 0% to 62.5%. [11],[12],[13]
Enucleation alone is associated with the highest recurrence rates (range, 17% to 56%), especially when the cyst is removed in fragmented fashion.[14] Various adjunctive therapies have been advocated to decrease recurrence potential; these include peripheral ostectomy or treating the surgical site with Carnoy’s solution, electrocautery, or cryotherapy.[15],[16],[17],[18] Marsupialization has also been reported but is associated with recurrences in the range of 25% to 100%.[19] Successful treatment by marsupialization alone or by marsupiali zation followed by enucleation has been reported.[20] Nakamura et al.[21] and Myoung et al.[22] found that KCOTs in the angle-ramus region of the mandible had a higher tendency to recur than those in the mandibular body. They explained this difference because of the difficulty in removing OKCs from the ramus.
It is thought that possible epithelial remnants in the lingual area may potentially give rise to untreatable recurrences in the soft tissues[23],[24],[25] In cases of lingual perforations,where vital structures are present, electro-cauterization is usually used.
Using Carnoy’s solution as adjunctive therapy resulted in reducing the reoccurrence rate. Handling of Carnoy’s solution is difficult and cannot be used near vital structures as this can cause permanent damage to the structures. Electro-cauterization is probably more effective in eliminating these possible epithelial remnants as its cauterizing effect reaches deeper than Carnoy’s solution. It is easy to use and we can have control over depth of penetration,when compared to Carnoy’s solution.
Electrocautery, also known as thermal cautery, refers to a process in which a direct or alternating current is passed through a resistant metal wire electrode, generating heat. The heated electrode is then applied to living tissue to achieve hemostasis or varying degrees of tissue destruction.[26] Electrocautery is a safe and effective method of hemostasis during cutaneous surgery.[27] It is also useful in the treatment of various small benign skin lesions,[26],[28] although only lesions that do not require histological review should be treated with electrocautery. There are no absolute contraindications to electrosurgery. Each electrocautery device can deliver heat at a single temperature or range of temperatures, between 100o C and 1200o C. A common principle of all electrosurgical procedures is to use the least amount of power possible to achieve the desired effect, limiting damage to the adjacent tissue.[29]
Transmission Of Infection
The 3 potential modes for infection transmission in these procedures during treatment could be due to electrode, surgical smoke, and aerosolized blood microdroplets. During procedures, aerosolized blood droplets can be propelled a distance of up to 30 cm and can be infectious if inhaled.[30] Surgical smoke can also contain viable viruses and bacteria, in addition to hazardous chemicals and carcinogens.[31]
To prevent the risks of infection transmission, a smoke-evacuating system should be used, along with facial masks, protective eye wear, and surgical gloves. Disposable or sterilized electrodes should be used.
Conclusion:
Electro cauterization can be used as one of the good adjunct for enucleation of KCOT lesions.
It is probably more effective in eliminating the possible epithelial remnants of the lesions. It is easy to use and we can have good control over depth of penetration when compared to Carnoy’s solution.
References
1. Wright J M. (1981) The odontogenic keratocyst. orthokeratinized variant. Oral Surg, 51: 609-618. 1
2. Neville BW, Damm DD, Allen CM, Bouqout JE.(2002) Oral and maxillofacial pathology. 2nd ed. Philadelphia: Saunders. 2
3. Shear M: Odontogenic keratocysts: Natural history and Immunochemistry. Oral and Maxillofacial Surgery Clinics of North America, 2003; 15 suppl 3:347-362. 2
4. Philipsen HP. Keratocystic odontogenic tumor. In: Barnes L, Eveson JW, Reichart P, Sindrasky D, editors. WHO Classification of Tumors. Pathology and Genetics of Head and Neck Tumors. Lyon: IARC Press; 2005. p. 306-307. 4
5. Shear M, Speight PM. Odontogenic keratocyst. In: Shear M, Speight PM editor(s). Cysts of the Oral and Maxillofacial Regions. 4th Edition. Oxford: Blackwell Munksgaard, 2007:6–58. 3
6. Bell RB, Dierks EJ: Treatment options for recurrent Odontogenic Cyst. Oral and Maxillofacial Surgery Clinics of North America, 2003; 15 suppl 3:429-446.
7. Pitak-Arnop P, Chaine A, Oprean N, Dhanuthai K, Bertrand JC, Bertolus C: Management of OKC of the Jaws : A 10 year experience with 120 consecutive lesions. Journal of Craniomaxillofacial Surgery, 2010; 38 suppl 5:358-364.
8. Ghali GE, Connor MS. Surgical management of the odontogenic keratocyst. Oral and Maxillofacial Surgery Clinics of North America 2003;15 suppl 3:383–92.
9. Schmidt BL. The use of liquid nitrogen cryotherapy in the management of the odontogenic keratocyst. Oral and Maxillofacial Surgery Clinics of North America 2003;15 suppl 3: 393–405.
10. Stoelinga PJ. The treatment of odontogenic keratocysts by excision of the overlying, attached mucosa, enucleation, and treatment of the bony defect with carnoy solution. Journal of Oral and Maxillofacial Surgery 2005;63 suppl 11:1662–6.
11. Bataineh AB, al Qudah M: (1998) Treatment of mandibular odontogenic keratocysts. Oral Surg Oral Med Oral Pathol Oral Radiol, 86:42.
12. Dammer R, Niederdellmann H, Dammer P, et al: (1997) Conservative or radical treatment of keratocysts: A retrospective review. Br J Oral Maxillofac Surg, 35:46.
13. Voorsmit RA, Stoelinga PJ, van Haelst UJ: (1981) The management of keratocysts. J Macillofac Surg, 9:228.
14. Hodgkinson DJ, Woods JE, Dahlin DC, et al: (1978) Keratocyst of the jaw Clinicopathologic study of 79 patients. Cancer, 41:803.
15. Forsell K, Forsell H, Kahnberg KE: (1988) Recurrence of keratocysts. A long-term follow-up study. Int J Oral Maxillofac Surg, 17:25.
16. Stoelinga PJW: (2001) Long-term follow-up on keratocysts treated according to a defined protocol. Int J Oral Maxillofac Surg, 30:14.
17. Schmidt BL, Pogrel MA: (2001) The use of enucleation and liquid nitrogen cryotherapy in the management of odontogenic keratocysts. J Oral Maxillofac Surg, 59:720.
18. Hsun-Tau C: (1998) Odontogenic keratocyst. A clinical experience in Singapore. Oral Surg Oral Med Oral Pathol Oral Radiol Endod, 86:573.
19. Irvine GH, Bowerman JE: (1985) Mandibular keratocysts: Surgical management. Br J Oral Maxillofac Surg, 23:204.
20. Waldron CA. (1995) Odontogenic cysts and tumors. In Oral and Maxillofacial Pathology, Neville BW, Damm DD, Allen CM, Bouquot JE eds, W.B.Saunders, Philadelphia, 493-540.
21. Nakamura N, Mitsuyasu T, Mitsuyasu Y, Taketomi T, Higuchi Y, Ohishi M. (2002) Marsupialization for odontogenic kerarocysts: long-term follow-up analysis of the effects and changes in growth characteristic.Oral Surg Oral Med Oral Pathol Oral Radiol Endod, 94, 543-553.
22. Myoung H, Hong SP, Hong SD, Lee JI, Lim CY, Choung PH, et al. (2001) Odontogenic keratocyst: review of 256 cases for recurrence and clinicopathologic parameters. Oral Sur Oral Med Oral Pathol Oral Radio and Endod, 91:328-333.
23. Worral SF. (1992) Recurrent odontogenic keratocyst within the temporalis muscle. Br J Oral Maxillofac Surg, 30: 59–62.
24. Emerson TG, Whitlock RIH, Jones JH. (1972) Involvement of soft tissue by odontogenic keratocysts (Primordial cysts). Br J Oral Surg, 9: 181–185.
25. Van Der Wal KGH. (1985) Development of a keratocyst in the facial soft tissues. J Oral Maxillofac Surg, 14: 146–152.
26. Pollock SV. Electrosurgery. In: Bolognia JL, Jorizzo JL and Rapini RP. Dermatology. 2nd edition. Mosby Elsevier; 2008:Ch140
27. Lane JE, O'brien EM, Kent DE. Optimization of thermocautery in excisional dermatologic surgery.Dermatol Surg. May 2006;32 suppl 5:669-75.
28. Soon SL, Washington CV. Electrosurgery, electrocoagulation, electrodesiccation, electrofulguration, electrosection, electrocautery. In: Robinson JK, Hanke CW, Siegel DM, et al. Surgery of the Skin. 2ndedition. Elsevier; 2010:Ch 9.
29. Massarweh NN, Cosgriff N, Slakey DP. Electrosurgery: history, principles, and current and future uses. J Am Coll Surg. Mar 2006;202 suppl 3:520-30.
30. Lewin JM, Brauer JA, Ostad A. Surgical smoke and the dermatologist. J Am Acad Dermatol. Sep 2011;65 suppl 3:636-41.
31. Berberian BJ, Burnett JW. The potential role of common dermatologic practice technics in transmitting disease. J Am Acad Dermatol. Nov 1986;15(5 Pt 1):1057-8.
|