Introduction:
Chronic periodontitis is an infectious disease resulting in inflammation within supporting tissues of the teeth, progressive attachment loss and bone loss.[1] Pregnant women are considered at higher than normal risk of developing gingival and periodontal disease. Thus, it is of prime clinical interest to assess individual woman’s risk for periodontal disease during pregnancy .Some of the studies have reported that sociodemographic variables influence the periodontal disease outcomes in pregnant women by influencing the individuals’ resources to pay for care, access to care, understanding of the importance of oral health, and effective selfcare practices.[11],[12],[13]
In light of these studies, we conducted a study on Pregnant women to evaluate the relationship between various socio-demographic and clinical variables affecting periodontal disease outcomes in them.
Materials And Methods:
The study included 180 pregnant women attending the Gynaecology and Obstetrics outpatient department (OPD) of SGRD Institute of Medical Sciences and Research, Amritsar. An informed consent was taken from all the subjects. A performa was designed for this study to record the patients’ age, socioeconomic status, profession, education level, and place of residence. The professional group was categorized into : working and non – working.Place of residence was categorized as : Urban and Rural.Patients were also enquired about their frequency of dental checkups and brushing. Periodontal maintenance was grouped as frequent if patient had undergone multiple visits in the previous year , infrequent if rare visit was made and never when no dental visit was made ever. Data were also collected about trimester of pregnancy Then, periodontal examination was carried out for each patient.
Periodontal examination and assessment
Periodontal examination was carried out by same examiner in all the patients in order to avoid interexaminer variability.
Following measurements were recorded for each tooth:
(1) Plaque index: Presence of dental plaque was recorded according to the Silness and Loe plaque index[14].
(2) Gingival Index : Presence of gingival inflammation according to Silness and Loe.
(3) Probing depth and recession depth was recorded using William’s calibrated probe.
(4) Clinical attachment level (CAL) was computed from the mean probing depth and recession depth measurements.
Statistical analysis
Mean and standard deviations were calculated for continuous variables and frequency distributions were studied for discrete variables. Analysis of variance (ANOVA) test was used to compare clinical indices between demographic and clinical characteristics and if results were significant, difference betweencategories was tested with the Chisquare test. Probability score of <0.001 was considered as highly significant.
Results:
The sociodemographic characteristics of population are listed in
Table I. The mean age was 26.69 ± 4.39 years, with majority of study population in the 17-25 (59.47%) and 26-30 (33.68%) years old categories. The predominant economicprofession was “non - working (65.6%), followed by “ working ” (34.4%). Most of the women under study were illiterate , 33.9% having no formal education , 31.1% educated up to matric level , 17.2% were graduates , and 17.8% were postgraduates. More than half of the sample (74.4%) lived in urban areas. About 39.4% of the women had never visited dentist, 48.9% visiting dentist rarely and only 11.7% women were regular with their dental check ups.
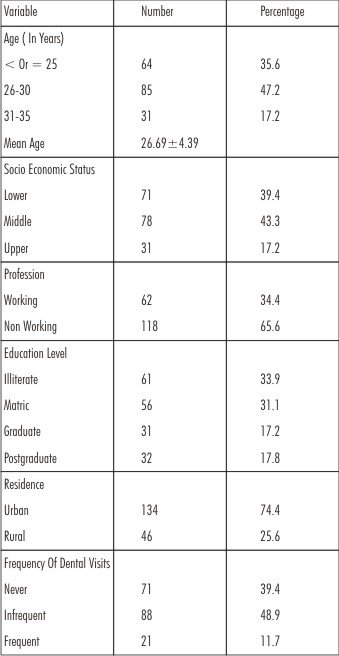 | Table I : Socio Demographic Description Of The Study Population
 |
Table II. Depicts the clinical variables related to pregnancy in the study population. The great majority of participants were in the third trimester (62.2%).
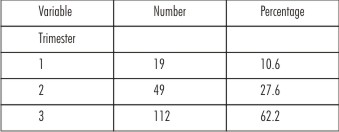 | Table II :Clinical Variables Related To Pregnancy
 |
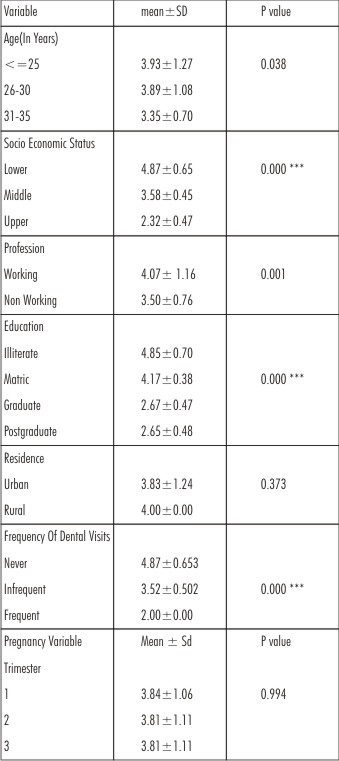
Table III. Shows a plaque index score in relation to various demographic variables and clinical variables related to pregnancy. Highly significant difference was observed in the plaque index scores among various groups of different socioeconomic status (P=0.000) , education level and frequency of dental visits. Plaque index score was significantly high in age group <= 25 years and among “working women” because most of the women belonged to lower socio economic strata and were employed in low – status jobs. No association was found between plaque index scores and place of residence and Trimester of pregnancy.
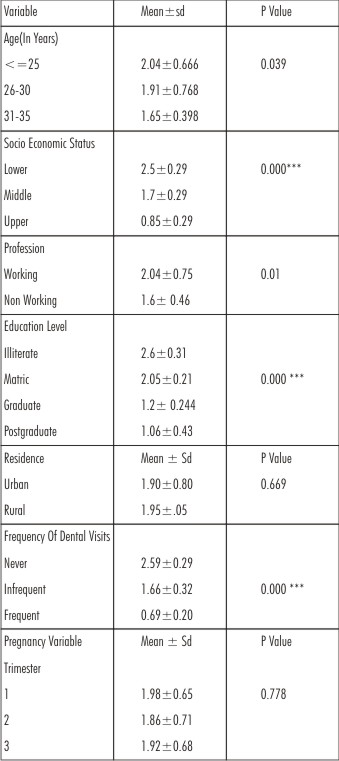 | Table III : Plaque Index In Relation To Socio-demographic Variables
 |
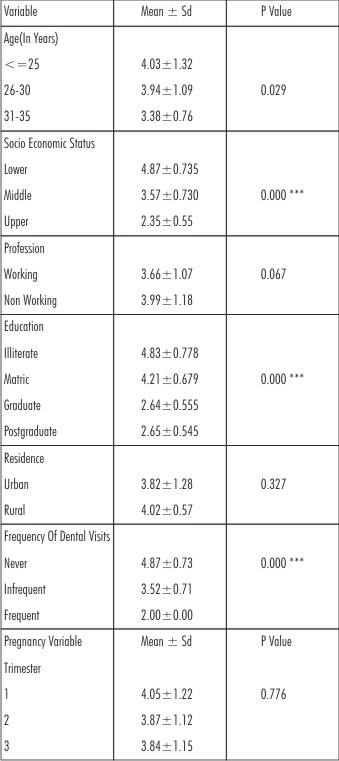
Table IV. Shows gingival index score in relation to various demographic variables and clinical variables related to pregnancy. A highly significant difference was observed in the plaque index scores among various groups of different socioeconomic status (P=0.000) , education level and frequency of dental visits. Gingival index scores were significantly high in “working women” . Non significant association was found between age, place of residence and trimester of pregnancy.
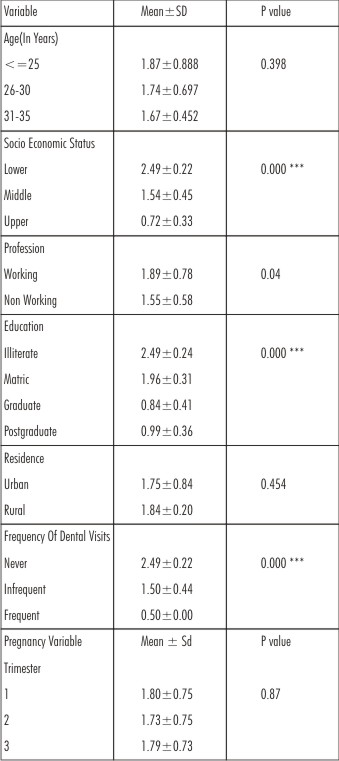 | Table IV : Gingival Index In Relation To Socio Demographic Variables
 |
Table V. Shows mean probing score in relation to various demographic variables and clinical variables related to pregnancy. Highly significant difference was observed in the plaque index scores among various groups of different socioeconomic status (P=0.000) , education level and frequency of dental visits. Probing depth was higher in age group <=25 years and among “ working women”. Non significant association was found between probing depth and place of residence and Trimester of pregnancy.
 | Table V : Probing Depth In Relation To Socio-demographic Variables
 |
Table VI. Shows CAL scores in relation to various demographic variables and clinical variables related to pregnancy. Highly significant difference was observed in the plaque index scores among various groups of different
Socioeconomic status (P=0.000) , education level and frequency of dental visits. CAL was non – significantly associated between professional groups, place of residence and Trimester of pregnancy.
 | Table VI : Clinical Attachment Levels In Relation To Socio Demographic Factors
 |
Discussion:
Since, last two decades, evidence has mounted regarding the association between periodontal infections and gestational complications including pre-term births(< 37 weeks), low birth weight(<2500 g)and or pre-term low birth weight and pre-eclampsia.[2],[3],[4] Periodontal diseases were reported as potential source of maternal infection and inflammation that may induce pre-term birth. Many physiological and hormonal changes occur during pregnancy. It is a well known fact that these changes could alter the oral metabolism. These include alterations in hormonal levels, microbial strains present in the oral cavity, immune response, and cellular metabolism.[5],[6]
The increase in progesterone levels causes loss of keratinization of gingival epithelium, proliferation of fibroblasts, impaired chemotaxis, and phagocytic activity of neutrophils.[7],[8],[9] The prominent microorganism Prevotella intermediaincrease in number because it uses progesterone as a nutrient which is available in GCF[10].
The incidence of gingival inflammation in pregnant women has been reported to range from 36% to 100%[15]. Silness and Löe determined that the correlation between the amount of dental plaque and the severity of gingivitis was higher postpartum than during pregnancy, and concluded that “some other factor” was involved in the etiology of pregnancy
Gingivitis[14]. Hormonal and vascular changes associated with pregnancy can exaggerate the response of the gingiva to bacterial plaque[16]. It has been reported that healthy gingival stays usually unaffected, and thus pregnancy itself does not cause gingivitis, but dental plaque or calculus is required for initiation of gingival changes during pregnancy[17]. Good oral hygiene practices, however, can minimize gingival disease during pregnancy[16],[18]. Therefore, good oral hygiene of patients in study population which is obvious from the low plaque index score could be attributable for low prevalence of periodontal disease in this population.
It is difficult to make comparison of study results with the previous studies because of the differences in study populations and study designs. Our study results are somewhat in accordance with study of Miyazaki et al[19].
They conducted a survey concerning periodontal disease prevalence and treatment needs in pregnant women ranging from 16 to 43 years of age in Kumamoto and Kitakyushu cities, Japan. They used CPITN values for the assessment of periodontal condition, which is quicker, simpler, and very useful for the field of public oral health. In our study, William’s caliberated probe was used to determine pocket depth. In their study, signs of periodontal disease were observed in 95% of the pregnant women and 96% of the nonpregnant women. More sextants showing healthy periodontal conditions were observed in the pregnant than in the nonpregnant women. In our study also most of the pregnant women had good periodontal health except women belonging to low socioeconomic status.
The most frequent age category in the present sample is 26 to 30 years old (47.2%), similar to that reported by Offenbacher et al[24]. That paper also included pregnant adolescents, which might have had a significant effect on the findings, whereas our study did not include any pregnant adolescents.
Our study results are in accordance with the study of Machuca et al[11]. They evaluated the periodontal status of pregnant women and its relationship to demographic variables in the province of Seville, Spain, and periodontal condition in their study population was related to different sociodemographic variables such as professional level, level of education, and previous periodontal maintenance. In our study also the periodontal status worsened as the socio economic status, education level and frequency of previous dental visits was less. As in their study, majority of our patients also came from lower economic strata, having high rates of unemployment (65.5%) and the remainder were mostly employed in a low status jobs where the treatment of periodontal diseases are not taken seriously.
Tilakaratne et al.[20] studied the effects of pregnancy on the periodontium, in a rural population of Sri Lankan women and their study results showed that pregnancy had an effect only on the gingiva and not on periodontal attachment levels.
In our study, highly significant results were obtained in relation to Plaque index, gingival index , mean probing depth and CAL(clinical attachment levels) in women of lower socioeconomic status, lower education level and in women who have never visited their dentist. It might be an attributed negligence of oral hygiene in women of lower socioeconomic status leading to increased gingival inflammation during pregnancy.
The levels of oestrogens are elevated in pregnancy leading to changes in keratinization of the gingival epithelium and alteration in the connective tissue ground substance. This results in decreased effectiveness of the epithelial barrier. These effects combined with vascular changes caused by elevated hormone levels give rise to aggravated response to the irritant effects of plaque, resulting in overt gingivitis.
Yalcin et al.[21] studied the effect of sociocultural status on periodontal condition in pregnancy in Turkish women by recording clinical measurements including the plaque index, gingival index, and probing depth. They evaluated interaction between these parameters and their sociocultural background. They reported the correlation of clinical index scores with educational level and periodontal care.
Wandera et al.[13] had examined periodontal status and tooth loss in pregnant Ugandan women and assessed the relationship with sociodemographic factors, parity (number of children), dental care, and oral hygiene. The oral condition of pregnant women was characterized by low prevalence of bleeding, high prevalence of calculus deposits, low prevalence of 4-5 mm pockets, and by a moderate prevalence of tooth loss. They concluded that age, social status, oral hygiene, and parity might be the potential risk factors for chronic periodontal disease in their study population. In our study, only the socioeconomic status, education, frequency of dental visits were a potential risk factor in the development of periodontal disease.
Moss et al.[22] emphasized that race is a significant factor governing the incidence and progression of periodontal disease and African Americans were more likely to experience incidence / progression of periodontitis as compared to other races. Jeffcoat et al. published interim results from an ongoing study in Alabama and reported that their population was made up of 83% African Americans, and that these subjects had significantly more periodontal disease. Unfortunately they did not report how much more[23].
Other factors such as socioeconomic status and profession are also important. Most of the patients (43.3%) belonged to category of middle socioeconomic status. Although most of the patients were non working (65.6%), majority of the sample was uneducated, having no formal education (33.9%). In the study of Machuca et al.[11], most of the patients were housewives but majority of them were educated up to primary level.
So, factors such as living area, ethnicity, socioeconomic status, education, and oral hygiene of patients may be responsible for the differences in study results of various studies taking into consideration influence of various sociodemographic factors on periodontal health of pregnant women.
Conclusion:
In the population of pregnant women investigated under this study, the clinical and socioR09;demographic characteristics showed highly significant correlation with socioR09;economic status , education level and frequency of previous dental visits, with gingival index, plaque index, pocket depth and clinical attachment level.Periodontal disease due to accumulation of plaque was the most characteristic periodontal condition in this sample and was related to socio economic status, level of education and previous periodontal maintenaince.Further studies may be required in Indian population to determine the association of periodontal diseases in pregnant women with socioR09;demographic variables.
References:
1. Perry R. Klokkevold. Relationship Between Periodontal Disease and Systemic Health. Carranza’a Clinical Periodontology 2012:11(1): 416.
2. Radnai M, Gorzo I, Nagy E, Urban E, Novak T, Pal A. A possible association between preterm birth and early periodontitis. A pilot study. J Clin Periodontol2004;31(9):736-41.
3. Collin JG, Smith MA, Arnold RR, Offenbacher S. Effects of Escherichia coli and Porphyromonas gingivalis lipopolysaccharide on pregnancy outcome in golden hamsters. Infect Immune 1994; 62(10): 4652-5.
4. Canakci V, Canakci CF, Canakci H. Periodontal disease as a risk factor for pre-eclampsia:a case control study. Aust NZJ Obstet Gynaecol 2004;44(6):568-73.
5. Amar S, Chung KM. Influence of hormonal variation on the periodontium in women. Periodontol 2000 1994; 6:79-87.
6. Jonsson R, Howland BE, Bowden GH. Relationships between periodontal health, salivary steroids, and Bacteroids intermedius in males, preganant and non – pregnant women. J Dent Res 1988; 67:1062-9.
7. Miyagi M, Aoyama H, Morishita M, Iwamoto Y. Effects of sex hormones on chemotaxis of human peripheral polymprphonuclear leukocytes and monocytes. J Periodontol 1992;63:28-32.
8. Willershausen B, Lemmen C, Hamm G. Modulation of gylcosaminoglycan - and collagen synthesis by human gingival fibroblasts by progesterone. Dtsch Zahnarztll Z 1991; 21:549-58.
9. Zachariasen RD. The effect of elevated ovarian hormones on periodontal health : Oral contraceptives and pregnancy. Women health 1993;20:21-30.
10. Kornman KS, Loesche WJ. The subgingival microflora during pregnancy. J Periodontol Res 1980;15:111-22.
11. Machuca G,Khoshfeiz O, Lacalle JR, Machuca C, Bullon P. The influence of general health and socio-cultural variables on the periodontal condition of the pregnant women. J Periodontol 1999;70:779-85.
12. Alwaeli HA, AL- Jundi SH. Periodontal disease awareness among pregnant women and its relationship with socio-demographic variables. Int J Dent Hyg 2005;3:74-82.
13. Wandera M, Engebretsen IM, Okullo I, Tumwine JK, Astrom. AN;PROMISE-EBF Study group. Socio-demographic factors related to periodontal status and tooth loss of pregnant women in Mbale district, Uganda. BMC Oral Health 2009;9:18-29.
14. Silness J, Loe H. periodontal disease in pregnancy.II. Correlation between oral hygiene and periodontal condition. Acta Odontol Scand 1964;22:121-35.
15. AL Habashneh R, Guthmiller JM, Levy S, Johnson GK, Squier C, Dawson DV. Factors related to utilization of dental services during pregnancy. JClin Periodontol 2005;32:815-21.
16. Raber-Durlacher JE, van Steenbergen TJ, Van der VeldenU, de Graaf J, Abraham- Inpijn L. Experimental gingivitis during pregnancy and post-partum: Clinical , endocrinological, and microbiological aspects. J clin periodontal 1994;21:549-58.
17. Gursoy M, Pajukanta R, Sorsa T, Kononen E. Clinical changes in periodontium during pregnancy and post-partum. J Clin Periodontol 2008;35:576-83.
18. Silness J, Loe H. Periodontal disease in pregnancy. . Response to local treatment. Acta Odontol Scand 1966;24:747-59.
19. Miyazaki H, Yamashita Y, Shirahama R, Goto – Kimura K, Shimada N, Sogame A. Periodontal condition of pregnant women assessed by CPITN. JClin Periodontol 1991; 18:751-4.
20. Tilakaratne A, Soory M, Ranasinghe AW, Corea SM, Ekanayake SL, de Silva M. Periodontal disease status during pregnancy and 3 months post-partum, in a rural population of Sri Lankan women. J Clin Periodontol 2000; 27:787-92.
21. Yalcin F, Eskinazi E, Soydinc M, Basegmez C, Issever H, Isik G. The effect of socio cultural status on periodontal conditions in pregnancy. J Periodontol 2002;73:178-82.
22. Moss KL, Beck JD, Offenbacher S. Clinical risk factors associated with incidence and progression of periodontal conditions in pregnant women. J Clin Periodontol 2005;32:492-8.
23. Jeffcoat MK, Geurs NC, Reddy MS, Cliver SP, Goldberg RL, Hauth JC. Periodontol infection and preterm birth: Results of a prospective study . J Am Dent Assoc 2001;132:875-880.
24. Offenbacher S, Katz V, Fertik G. Periodontal infection as a possible risk factor for preterm low birth weight. J Periodontol 1996;67:1103-13.
|