Introduction
One of the most important factors involved in preventive and interceptive dentistry is the preservation of the primary dentition until the normal time of exfoliation. Owen cited numerous implications of premature primary tooth loss, including permanent arch-length decreases, increased overbite, increased crowding, tooth malposition, impactions, arch asymmetries, occlusal impairment, and disrupted eruption sequences. In the absence of the primary second molar, mesial movement and migration of the permanent molar may occur prior to and during eruption.[1] Retention of a nonvital second primary molar before and during the eruption of the permanent first molar has been advocated for a long time. If, however, the second primary molar is extracted, severe space loss probably would occur (Forrester et al. 1981; Stewart et al. 1982; Goerig and Camp 1983; Mathewson et al. 1987; McDonald and Avery 1987; Pinkham 1988). Even when the prognosis is in doubt, root canal treatment of the infected primary second molar allows the first permanent molar to erupt fully into its normal position after which the second molar can be removed and an appropriate space management technique initiated.[2]
Allen (1979), Wright & Widmer (1979), Camp (1984) mentioned reports about the unsuccessful root canal treatments of nonvital primary molars and the long term effects on the developing occlusion. Starkey felt that delayed eruption of the permanent successors sometimes followed pulpotomy and pulpectomy treatment of primary molars, with some possible deflection in the eruption path. Coil et al. (1985) described 41 nonvital root canal treatments of primary molars in 37 children and reported success to be 80%.Coll and Sadrian, in a retrospective study of pulpectomy outcomes, noted two parameters that were the highest predictors of success. Pretreatment pathologic root resorption, when evident, resulted in a 44.4% prevalence of enamel defects in underlying permanent teeth after their eruption. In the absence of pretreatment pathologic root resorption, the pulpectomy success rate was 91.7%.[2],[3],[4]
Literature Review
Little is mentioned in literature about the unsuccessful root canal treatments of nonvital primary molars and the long term effects on the developing occlusion (Allen 1979; Wright and Widmer 1979; Camp 1984). Coll et al. (1985) and Spedding (1985) described 41 nonvital root canal treatments and reported success to be 80% in 37 children.[2],[5],[6]
Peter Ngan and Henry Fields (1995) described disadvantages of distal shoe appliance as a foreign body and difficulty in its construction. An alternative approach that requires more mechanotherapy and corrective action is a reverse band and loop placed at the time of eruption of first permanent molar which was first described by Gellin (1990).[7]
Case Report
A 5 and a half year old boy name Umed (Fig 1) reported to the Department of Pedodontics and Preventive Dentistry with a chief complaint of decayed tooth since 3-4 months and swelling in the left lower back region of the jaw since 2 weeks. Two weeks prior, another dentist prescribed an antibiotic for the child but provided no dental treatment. There were no significant medical findings. No swellings or mobility of any teeth were noted and no discomfort was reported.
 | Fig 1 : Facial Profile Of Patient
 |
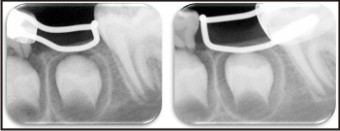
On intraoral examination, it was found that 51 and 61 (Fig 2) were carious. Whereas 75 was pulpally involved (Fig 3) and 64 was previously root canal treated with no associated symptoms. When the radiovisiograph of the area was examined the second primary molar (75) appeared to have carious pulp exposure but no periapical pathosis was noted. So a diagnosis of chronic irreversible pulpitis for tooth no 75 was made.Physiological Root resorption with respect to 64 with 1/3rd of the roots remaining was noted.
 | Fig 2 : Maxillary Arch Showing Carious 51,61 &fig: 64 With Pre-operative Rvg Wrt 64
 |
 | Fig 3 : Mandibular Arch Showing Carious 75 With Pre-operative Rvg Wrt 75
 |
Treatment plan
Based upon the arch analysis and age factor, it was decided to extract 64 and 75 followed by band and loop space maintainer in 64 and reverse band and loop in 75. Reverse band and loop was chosen as first permanent molar was partially erupted into oral cavity ruling out the need for distal shoe space maintainer. As the patient was apprehensive about the treatment, it was decided to perform the procedure under nitrous oxide sedation (Fig 4).
 | Fig 4 : Patient Was Done Under N2o Sedation And 54 And 75 Were Extracted
 |
Space Maintenance
Fourdays after the extraction the maintainer was inserted (Fig 5 & Fig 6). This maintainer was used for one year and six months (Fig 7) because it took that long for the first permanent molar to erupt completely. The maintainer was removed and replaced with a band and loop space maintainer cemented on the first permanent molar (Fig 8 & Fig 9). After this the patient didn’t report back for any follow up.
 | Fig 5 : Post-operative Maxillary Arch, Band And Loop Space Maintainer Wrt 64 Delivered
 |
 | Fig 6 : Post-operative Mandibular Arch, Reverse Band And Loop Space Maintainer Wrt 75 Delivered
 |
 | Fig 7 : After 6 Months, Note The Eruption Of First Permanent Molar Into Oral Cavity
 |
 | Fig 8 : Shift The Space Maintainer From 74 To 36
 |
 | Fig 9 : Follow Up After 1 Year And 6 Months With Change In Space Maintainer From Reverse Band And Loop To Band And Loop.
 |
Discussion
One of the most frustrating problems of managing the developing dentition is the premature loss of the primary second molar prior to the eruption of the permanent first molar. An erupting tooth adjacent to an edentulous area has a greater potential for space loss than fully erupted ones, indicating that clinical intervention should be considered. Without timely intervention, molar relations can alter resulting in impaction of premolars.[1]
Questions can be asked about the treatment procedures used to manage this case. If the parents would have reported at an earlier age, the emergency treatment could have been performed and tooth could be saved. But the parents reported when treatment options were limited to extraction only. An immediate space maintainer should have been inserted because space loss can occur immediately after the premature loss of a mandibular second primary molar (Northway et al. 1984). Distal shoe or its modifications could be used at the time of extraction but the limitations in its fabrication and partial eruption of first permanent molar prohibited its use (Hicks 1973; Kapala 1980; Barber 1982; Mathewson et al. 1982; McDonald et al. 1987). A third alternative would have been to extract the mandibular primary second molar and do nothing else. Because this extraction would occur before the eruption of the permanent first molar severe space loss probably would occur. As previously noted, the retention of a nonvital second primary molar is advocated before and during the eruption of the first permanent molars. Even when the prognosis is in doubt, the objective is to allow the first permanent molar to erupt fully using the distal surface of the crowned second primary molar as a guide, then to extract the second primary molar and use appropriate space management procedures. However, if this alternative is not selected and the second primary molar is extracted at a young age, severe loss of mandibular arch circumference might require complex orthodontic treatment. The fact that some clinical procedures can fail, as noted in this report, emphasizes the need to inform parents about treatment sequence and to impress on them that even if they are compliant treatment can fail. Therefore, alternative methods of treatment may be indicated at an additional cost.
References
1. Dhull KS, Bhojraj N, Yadav S & Prabhakaran SD: Modified distal shoe appliance for the loss of a primary second molar: A case report. Quintessence Int 2011;42:829-33.
2. Gillen ME & Spedding RH: Space management required after unsuccessful root canal therapy of a mandibular second primary molar: case report.Pediatr Dent 1990: 12(4):253-256.
3. Ng YL, Mann V, Rahbaran S, Lewsey J & Gulabivala K. Outcome of primary root canal treatment: systematic review of the literature – Part 1. Effects of study characteristics on probability of success. International Endodontic Journal 2007: 40, 921–939.
4. Ingle JL, Beveridge EE, Glick DH, Weichman JA (1965) Modern endodontic therapy. In: Ingle JL, Bakland LK, eds. Endodontics, 4th edn. Baltimore, MA: Williams and Wilkins 1994, pp. 27–53.
5. Coll JA, Josell S, Casper JS: Evaluation of a one-appointment formocresol pulpectomy technique for primary molars. Pediatr Dent 7:123-29, 1985.
6. Spedding RH: Incomplete resorption of resorbable zinc oxide root canal fillings in primary t eeth: report of two cases. ADCJ Dent Child 52:214-16, 1985.
7. Ngan P & Fields H. Orthodontic Diagnosis and treatment planning in the primary dentition. Journal of Dentistry for children 1995: 25-33.
8. Kapala JT: Interceptive orthodontics and managemenotf space problems, in Textbook of Pediatric Dentistry, Braham RL, Morris ME eds. Baltimore: Williams and Wilkins, 1980, p 347.
|