Introduction
The peripheral giant cell granuloma (PGCG) is a relatively common tumor-like growth of the oral cavity.[1] It accounts for 7% of all benign tumors of the jaw. It originates from the connective tissue of the periosteum or from the periodontal membrane, in response to local irritation or chronic trauma as a result of local irritating factors such as tooth extraction, poor dental restorations, food impaction, ill-fitting dentures, plaque, and calculus.[2] It has a slightly higher prevalence in the 30-70 year-old-age group, and affects largely the mandible than in the maxilla (4:1).[3]
Clinical appearance of PGCG can present as polyploidy or nodular lesion. Primarily bluish red with a smooth shiny surface, pedunculated or sessile base, small and well demarcated. Pain is rare and in most cases the lesion is induced by constant trauma.[2] Lesion can arise on facial and lingual gingival mucosa.
Radiologically, no significant findings can be observed. Rarely, the underlying alveolar bone may show superficial erosion with pathognomonic peripheral cuffing of bone as seen in radiograph.[4] Histological features of PGCG reveal a non-capsulated mass of tissue containing a large number of young connective tissue cells and multinucleated giant cells. Hemorrhage, hemosiderin, inflammatory cells, and newly formed bone or calcified material may also be seen throughout the cellular connective tissue.[5]
Case Report
A 60 year old male patient reported to Department Of Periodontology with chief complain of difficulty in chewing food owing to presence of painless intra-oral swelling in relation to lower right jaw region since 10 month (Fig. 1 & 2). Past dental history revealed excision of same lesion 1 year back followed by recurrence since 10 months. The patient was apparently allright when he again noticed the same lesion 10 months back. To start with, the lesion was peanut in size and slowly progressed to attain the present size. There was no history of any other swelling in any other part of the body. Medical history revealed that patient was known hypertensive and was in control and on regular treatment.
 | Figure 1 : Firm, Smooth And Sessile Swelling, Extending From Distal Of First Molar To Mesial Of First Premolar (Buccal View)
 |
 | Figure 2 : Firm, Smooth And Sessile Swelling, Extending From Distal Of First Premolar To Mesial Of First Molar (Occlusal View)
 |
Clinical Examination
Extra-Oral Examination: Showed slight asymmetry on right lower border of premolar and molar mandibular region because of distension created by intra- oral swelling. Lymph nodes were not palpable.
Intraoral Examination
Inspection: A solitary exophytic nodular lesion visible at right mandibular region extending from first premolar to second molar region, measuring 17×15×20mm in size. The colour was bluish red and surface over lesion was ulcerated (Fig 1 & 2). Oral hygiene status was found to be poor.
Palpation
The inspectory findings regarding number, site, shape and size were confirmed. The lesion was found to be sessile, with broad base, mobile and non- tender.
Radiographic Finding
Intra-Oral Periapical radiograph interpretation revealed well demarcated “Cuffing” like radiolucency extending from distal aspect of first premolar to mesial aspect of second molar (Fig. 3).
 | Figure 3 : Intraoral Periapical Radiograph Of The Patient Showing Well Demarcated Cuffing Like Radiolucency Extending From Distal Of First Premolar To Mesial Of First Molar
 |
Treatment
Treatment plan included physician’s opinion and consent, Phase I therapy to start with and response to Phase I therapy was assessed after 3-4 weeks. The excisional biopsy was done under local anesthesia, ie lignocaine hydrochloride and adrenaline in the dilution of (1:200000). The excision was done in toto with rim of normal tissue and upto the periosteum around the lesion to avoid recurrence (Fig. 4). Then the excised lesion was transferred to bottle containing 10% formalin and sent to Oral Pathology Department for biopsy and histopathological report. The bleeding from the surgical site was controlled with the help of pressure pack and suture. Periodontal dressing (Coe-Pak(R)) was then placed in relation to the same. The patient was given post-operative instructions along with antibiotics, Cap: Amoxycillin 500mg tid for 5 days and analgesics and anti-inflammatory, ie Tab: Ibuprofen 400 mg tid for 3 days. The patient was then recalled after one week for suture removal. No immediate complications were observed at the time of suture removal (Fig. 5). Following removal of suture, the surgical site was profusely irrigated with normal saline and recalled after 3 months for follow up. Upon 3 month follow up, the healing of surgical site was uneventful with no signs of recurrence (Fig. 6). Finally, the patient was referred to the concerned department for rest of the treatment.
 | Figure 4 : Surgically Excised Round And Well Encapsulated Lesion With Smooth Surface Texture
 |
 | Figure 5 : Post- Operative View One Week After Surgery
 |
 | Figure 6 : Post- Operative View Three Months After Surgery
 |
Histopathological Examination
On gross examination, the excised nodule was red in colour measuring 17×15×20 mm in maximum dimension. Histologically, microscopic features showed parakeratinized squamous epithelium, overly fibrocellular stroma. Connective tissue showed predominant giant cells with 10-15 nucleus within cells. Stroma showed plump to spindle fibroblasts and dense bundle of collagen fibrils. Predominant endothelial lined blood vessels with extravasated RBCs were seen. Patchy inflammatory cells were evident (Fig 7 & 8).
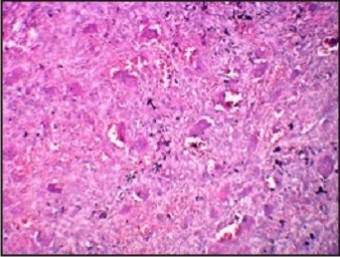 | Figure 7 : Under Higher Magnification The Giant Cells Are Showing 8-25 Nuclei And Are Scattered Throughout The Cytoplasm
 |
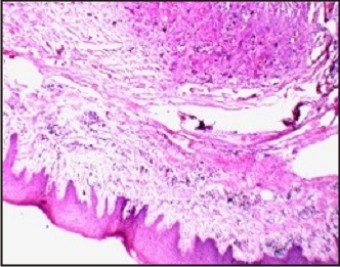 | Figure 8 : Hematoxylinand Eosin Stained Section Showing Parakeratotic Stratified Squamous Epithelium Overlying Connective Tissue Stroma.
 |
Discussion
PGCG is a uncommon benign lesion of the oral mucosa which originates from the gingiva or mucoperiosteum of alveolar bone and is caused by local irritation and chronic trauma. The preferential location of the lesion according to Pindborg isthe premolar and molar zone, though Shafer and Giansanti suggestthat it generally occurs in the incisor and canine region.[6] Clinically, PGCG is smooth, nodular brown, red or bluish nodule which is sessile or pedunculated.[5] Radiographic features are generally nonspecific. However, sometimes they reveal superficial destruction of the alveolar margin or crest of the interdental bone when the granuloma is seen associated with the teeth. In cases where the granuloma is associated with the edentulous ridge, it characteristically exhibits superficial erosion of the bone with peripheral "cuffing" of the underlying bone.[7] There are no pathognomonic clinical features whereby these lesions can be differentiated from other forms of gingival enlargement. Microscopic examination is required for definitive diagnosis.[8] Histologically, PGCG is identified as a non-encapsulated mass of tissue compiled of a reticular and fibrillar connective tissue stroma containing profuse young connective tissue cells of ovoid or fusiform shape and multinucleated giant cells. The microscopic appearance of PGCG is distinctive mainly due to the large number of multinucleated giant cells that are disseminated in the connective tissue stroma.[9] The differential diagnosis of PGCG includes central giant cell granulomas, which are located within the jaw itself and exhibit a more aggressive behavior,[10] pyogenic granuloma, fibrous epulis, peripheral ossifying fibroma, inflammatory fibrous hyperplasia, peripheral odontogenic fibroma, hemangioma caverosum and papilloma,[11] thebrown tumors of hyperparathyroidism, in which changes in blood chemistry confirm the diagnosis.[12] The surgical resection with elimination of the entire base of the lesion and removal of the underlying etiologic factors has yielded successful results in the treatment for PGCG. The superficial resection may lead to recurrence of the growth.[13] When the adjacent teeth are periodontally involved, their extraction may prove necessary to ensure full resection, though this is initially contraindicated[14].There has been reported wide variation of 5% to 70.6% in the recurrence rate of PGCG.[15], [16]
Conclusion
Etiology of PGCG is not clearly established. Low socioeconomic status of the patients and unfavorable oral hygiene seem to be predisposing factors. Excision down to periosteum along with elimination of etiologic factors is the line of treatment to prevent the recurrence.
References
1. Neville BW, Damm DD, Allen CM, Bouquot JE. Soft Tissue Tumors. In Neville BW, Damm DD, Allen CM, Bouquot JE, eds. Oral and Maxillofacial Pathology 3rd ed. St. Louis: Saunders; 2009: 507-563.
2. Pour MAH, Rad M, Mojtahedi A. A Survey of Soft tissue Tumor-Like Lesions of Oral Cavity: A Clinicopathological Study. Iranian Journal of Pathology 2008; 3: 81-87.
3. Aslan M, Kaya GS, Day E, Demirci E. A Peripheral giant cell granuloma in early age (case report). Ataturk Univ Dis HekFakDerg 2006; 16 (3): 61-64
4. Subarnbhesaj A. Peripheral Giant Cell Granuloma: A Case Report and Review of Literature. KhonKaen Dental J 2005; 8:125-30
5. Shafer WG, Hine MK, Levi BM. Tratado de patologìaBucal. eds. 4th. Rio de Janeiro: Guanabara-Koogan; 1987
6. Etoz OA, Demirbas AE, Bulbul M, Akay E. The Peripheral giant cell granuloma in edentulous patients: report of three unique cases. Eurpenjournol of dentistry 2010; 4:329-33
7. Reichart PA, Philipsen H. Atlas de Patologìa Oral.eds.1 Masson; 2000. p. 164
8. Subarnbhesaj A. Peripheral Giant Cell Granuloma: A Case Report and Review of Literature. KhonKaen Dental J 2005; 8:125-30
9. Shafer WG, Hine MK, Levy BM. A Textbook of Oral Pathology. 4 th ed Philadelphia, W B Saunders Company; 1983. p. 144-6.
10. Giansanti JS, Waldron CA. Peripheral giant cell granuloma: A review of 720 cases. J Oral Surg 1969; 27:787-91
11. Pindborg JJ. Atlas deenfermedades de la Mucosa Oral. 5 th ed. Barcelona: EdicionesCientificasTecnicas; 1994.p. 186.
12. Katsikeris N, Kakarantza-Angelopoulou E, Angelopoulos AP. Peripheral giant cell granuloma:Clinicopathologic study of 224 new cases and review of 956 reported cases. Int J Oral MaxillofacSurg 1988; 17:94-9
13. Bodner L, Peist M, Gatot A, Fliss DM. Growth potential of peripheral giant cell granuloma. Oral Surg Oral Me Oral Pathol Oral Radiol Endod 1997; 83:548-51
14. Neville BW, Damm DD, Allen CM, Bouquot JE. Oral and Maxillofacial Pathology. Pennysylvania: W B Saunders Company; 2004. p. 449-50.
15. Erkan Ozcan, Serkan Bodur, Galip Erdem.Peripheral Giant Cell Granuloma A Case Report. Pakistan Oral & Dental Journal, June 2011, Vol 31, No. 1, 171-172
16. Osman A. Etoz, Ahmet EminDemirbas, Mehmet Bulbul, and EbruAkay. The Peripheral Giant Cell Granuloma in Edentulous Patients: Report of Three Unique Cases. Eur J Dent. 2010 July; 4(3):329–333.
|