Introduction
Electrosurgery has been used in the field of dentistry for several decades. It has been defined as the intentional passage of high frequency waveforms, or currents through the tissues of the body to achieve a controllable surgical effect[1].Tissues are naturally resistant to high frequency waveforms; when these waveforms pass through it, intense intracellular heat is produced within the tissues contacted by the active electrode. This heat volatises cells, and as the electrode is guided through the tissue, it leaves a path of cell destruction in the form of an incision or surface coagulation[1].
Adverse healing responses, including necrosis of soft tissue and sequestration of alveolar bone, have been reported sparsely following the use of electrosurgery[2],[3]. Hence, we report such a rare case of gingival and alveolar bone necrosis following gingivectomy using electrocautery.
Case Report
An 18year old female patient came to us with a complaint of deposits on her teeth as well as a desire to get her teeth cleaned. She claimed to be systemically healthy and with no known drug allergy in the past. This was patient’s first dental visit. On extraoral examination, no abnormalities were detected.
On intraoral examination, patient’s oral hygiene was good. The labial gingiva irt 13-23 and 33-43 was observed to be enlarged, firm and resilient in consistency and pseudopockets were observed in the same area. Localized recession irt 41 which was labially placed and deep bite, cross bite in relation to 12,42 was also noticed. (Fig 1, 2). Her routine blood investigation reports were normal. The case was diagnosed with localized chronic inflammatory enlargement of the upper and lower anteriors.
 | Fig 1 : 1st Visit Intraoral View
 |
 | Fig 2: 1st Visit Lower Arch View
 |
Consultation from the Orthodontist was taken to treat the deep bite as well the crowding in relation to lower anteriors. The orthodontist was of the opinion to treat the gingival condition first and then to proceed with the orthodontic correction. The treatment plan for the patient was to perform scaling in the phase I therapy and to evaluate for further requirement of surgical therapy for correction of the enlargement.
Scaling was performed and oral hygiene instructions were given and evaluated after one month. All areas responded to phase 1 therapy except in the maxillary and mandibular anteriors which showed persistent enlargement. Hence gingivectomy and gingivoplasty was planned using electrocautery. After providing infiltration anesthesia, transgingival probing revealed the gingival biotype to be thick. Pocket marking was done using Crane Kaplan pocket marker. The incisions were provided with small loop tip of the Sensimatic electrosurge 500 SE unit (Parkell,USA) at low power setting(cut and coagulate). Adequate cooling of the tissues were provided with saline irrigation during the incision procedure. Gingivoplasty was performed to achieve a harmonious contour. Adequate hemostasis was achieved. Periodontal dressing was placed and the patient was dispensed with amoxicillin 500 mg , 3 times daily for a period of 5days and analgesics (Acecloren 100mg bd) (Fig 3,4,5).
 | Fig 3 : Pocket Marking Being Done Using Pocket Marker
 |
 | Fig 4 : Bleeding Points After Pocket Marking
 |
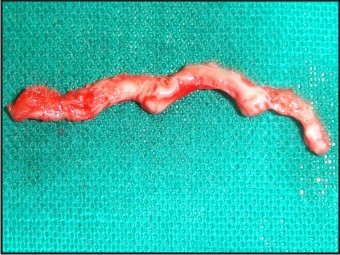 | Fig 5 : Excised Fibrous Tissue
 |
At the 1st week recall the periodontal dressing was removed. On examination of the gingival condition there was pseudomembrane formation of the gingival tissues in the surgical site (11,12,13,21,22,23) and loss of interdental papilla irt 12,22 (Fig 6). Patient was asymptomatic. The necrotic area was debrided using cotton pellets dipped in 3% hydrogen peroxide. The areas were curetted to induce fresh bleeding. Patient was dispensed with instructions to use a soft brush to clean the area and to use 3% of hydrogen peroxide mouthwash twice daily. She was also prescribed vitamin supplements and asked to continue the antibiotics for 1 more week and instructions to follow up 1 week later.
 | Fig 6 : 1 Week Postoperative Showing Pseduomembrane In The Surgical Area
 |
She reported 15days later and on examination of the gingiva, there was a clear erythmatous line demarcating the necrosed tissue from the healthy. Bone necrosis was observed in relation to 12,22 (Fig 7). The areas were again debrided with cotton pellets dipped in 3% hydrogen peroxide mouthwash. Oral hygiene instructions were reinforced and to follow up a week later. But the patient missed this follow up appointment and reported to us only a month later.
 | Fig 7 : 15days After 1st Follow Up
 |
At this appointment the patient was again evaluated. It was seen that inflammation persisted in relation to 12,22. Bony sequestrum was visible in the area of 12 (Fig 8). The bony sequestrum was removed using a curette under local infiltration (Fig 9). The area was irrigated with saline. Deplaquing was performed using ultrasonics. Patient was asked to continue with the oral hygiene practices. Remarkable healing of the gingiva was observed in the subsequent visit. Gingivectomy and gingivoplasty was performed for the lower anteriors using conventional technique and healing was uneventful (Fig 10). Patient is kept on maintenance and has been referred to orthodontist for correction of deep bite.
 | Fig 8 : 1 Month After 1st Follow Up Showing Sequestrum
 |
 | Fig 9 : After Removal Of The Sequestrum Irt 12
 |
 | Fig 10 : 3 Months After The 1st Follow Up
 |
Discussion
Electrosurgery has several applications in almost all branches of dentistry. We decided to use electrosurgery as it has the advantages of providing clean tissue separation , adequate hemostasis, planing of soft tissue, healing discomfort and scar formation are minimal. Chair time and operator fatigue are reduced, with technique being pressureless and precise[1].
Disadvantages of electrosurgery includes odor of burning tissue, cannot be used on patients with pacemakers that are not shielded against external interference[1]. The number of advantages outweigh the number of disadvantages of electrocautery and hence is used overwhelmingly in periodontics for curettage, gingivectomy procedures. Adverse healing responses, including necrosis of soft tissue and sequestration of alveolar bone, have been reported following the use of electrosurgery for intraoral incisions[2],[3],[4]. These responses are usually attributed to excessive heat accumulation during the surgical procedure[2],[3].
When the active electrode tip contacts the tissue, the electrode itself does not produce any significant heat rather the intense heat that is required for the electrosurgical effect is generated within the tissues that are contacted by the electrode tip. While this intracellular heat causes disruption of cells at the line of incision and/or coagulation, some of it also spreads to the adjacent cell layers. This heat is called lateral heat[1]. Any alterations which occur during healing are a result of tissue denaturation secondary to collection of lateral heat[5].
Lateral heat caused coagulation necrosis is minimal, and any unwanted tissue destruction is caused by excess lateral heat.It is influenced by factors like size and type of active electrodes. The thicker the electrode the greater amount of heat. In the present case the necrosis could have been because we used a loop electrode instead of a needle type electrode. Thicker electrode also require a high power setting , which inturn will produce increased lateral heat. Successive applications on the tissues should have a time gap of 10-15sec interval. This interval allows the heat to dissipate and prevents overheating of the tissues[1]. Moist tissue maintenance is also essential. In the present case, the mentioned precautions were taken.
Reports of histological evaluation of healing following electrosurgery have been conflicting. While some investigators have demonstrated healing following electrosurgical incisions to be similar to that following surgical blade incisions, others have noted considerable differences[5]. In the present case, conventional gingivectomy performed in the lower anteriors healed uneventfully when compared to the maxillary anteriors which showed adverse and delayed healing.
Coelho showed that although there is a loss of tissue soon after electrosurgery, 70%-100% of the tissues are regained over a period of months[1]. A similar type of healing was observed in the present case in just about 2 months. Though gingival recession has been reported as a complication in the present case no recession was observed[1], [7].
Bone and cementum are two dense oral tissues that can be detrimentally affected by contact or close proximity with an electrosurgery electrode. Dense tissue has less of a potential to dissipate heat as compared to soft tissue. Electrosurgery can increase bone destruction, osteoclastic bone resorption, acute inflammatory response and adverse wound healing with sequestration[6]. A similar mechanism can be proposed for the tissue destruction which we have observed in the present case.
Conclusion
Electrosurgery has several applications in almost all branches of dentistry. This case report throws some light on the adverse effects of usage of electrosurgery on the periodontal tissues including necrosis of soft tissue and sequestration of alveolar bone. Strict adherence to the clinical guidelines for the use of electrocautery should be followed .The use of newer advances which have the advantage of minimal lateral heat production should be encouraged.
References
1. Johnson David Gnanashekar, Yousef Saleh Al. Electrosurgery in dentistry. Quintessance International 1998; 29(10):649-654
2. Kenneth L. Kalkwarf,Robert F. Krejci, Allen R. Edison, Richard A. Reinhardt.Lateral heat production secondary to electrosurgical incisions. Oral Surg Oral Med Oral Pathol. 1983 Apr;55(4):344-8
3. Jimbu Yoshinori, Akasaka Yoko, Naito Hiromi. A Case of Gingival and Alveolar Bone Necrosis Probably Caused by Electorosurgery. Journal of the Japanese Stomatological Society 2001; 50(4):256-258
4. Kenneth L. Kalkwarf,Robert F. Krejci, Allen R. Edison, Richard A. Reinhardt. Subadjacent heat production during tissue excision with electrosurgery. J Oral Maxillofac Surg. 1983;41:653-57
5. Kenneth L. Kalkwarf,Robert F. Krejci, Allen R. Edison, Richard A. Reinhardt. Epithelial and connective tissue healing following electrosurgical incisions in human gingiva. J Oral Maxillofac Surg 1983; 41: 80-85
6. Russell Dylla. Electrosurgery.J of Minnesota dental association.2005;84(3)
7. Krejei RF, Kalkwarf KL, Krause- Hohenstein U : Electrosurgery – a biological approach. J Clin Periodontal 1987; 14 : 557- 63.
|