Introduction
Diastema is any space or a gap greater than 0.5mm between the central incisors. It is one of the most common forms of incomplete occlusion seen more frequently between the maxillary incisors than the mandibular incisors[1]. Epidemiological studies have shown that the prevalence of midline diastemas is higher in children (during the mixed dentition period) which is physiological and decreases gradually up to 15 years of age. The etiology of maxillary diastema is believed to be multifactorial. They may vary from being physiological (as in children) to various developmental anomalies of teeth and its associated oral tissues, prolonged abnormal oral habits, loss of equilibrium of the oral musculature, maxillary midline pathology, periodontitis and abnormal structure of the maxillary arch. Wide diastemas result in an unaesthetic smile, occasional impairment of phoneticsand difficulty in maintaining oral hygiene.
Based on the etiological factors, midline diastema can be managed either by surgical, orthodontic, periodontal, restorative and prosthetic procedures or by combination of procedures to fulfill patient’s aesthetic and functional demands[2], [3], [4].
Recent advances in direct dental composite resins, gives the dental practitioner an advantage to perform direct bonding procedures with minimal invasive procedures on the tooth. This conservative procedure also called minimally invasive cosmetic dentistry is a chair side procedure which is less time consuming. Inclusion of minimal laboratory procedure to fulfill the aesthetic and functional demands of the patientwill make the restoration more successful[5].
This article presents a case report of management of maxillary midline diastema, with direct composite resin restoration with a minimal laboratory procedure.
Case Report
A 26 year old male patient reported to the department of Prosthodontics, with a chief complaint of dislodged filling in the upper front teeth which he felt was unpresentable.
On clinical examination, a discolored composite restoration splinting the two maxillary central incisors in the midline was seen. This restoration had debonded and the patient was using it as a removable prosthesis. (Fig 1) The interdental papilla between the central incisors was flattened and depressed affecting aesthetics of the patient. It was observed that the anterior guidance was present only on the splinted composite restoration. A diastema of 4mm was noted between 11 and 21, when the debonded composite restoration was removed. (Fig 2).
 | Figure 1. Intraoral view showing stained composite resin restoration splinting maxillary central incisors and depressed interdental papilla
 |
 | Figure 2. Extraoral view showing wide diastema between maxillary central incisors affecting smile
 |
The oral hygiene of the patient was good, and no significant hard and soft tissue findings were found. Angle’s Class I occlusion with normal overjet and overbite was noted. The labial frenum associated with the diastema was normal in size and position. Radiographic examination revealed no significant findings with respect to 11 and 21.
Various treatment modalities (orthodontic, conservative restorative and prosthetic procedures) were discussed with the patient. The patient was neither willing for time consuming orthodontic treatment nor for invasive prosthodontic procedures. Therefore a minimally invasive approach with a direct composite resin restoration was planned to restore the diastema.
Procedure
Maxillary and mandibular diagnostic impressions using irreversible hydrocolloid (Zelgan Plus, Dentsply India) were made and poured with dental stone (Kalstone, Kalabhai India). It was observed that the maxillary central incisors were proportionately smaller compared to the size of right and left lateral incisors and canines. Diagnostic casts were mounted on a semi-adjustable articulator (Hanau Wide Vue II, Whipmix Corp, USA)(Fig 3). There was a scope for increasing the actual width by 1mm on each central incisor which would close the diastema by 2mm. Diagnostic wax-up (Crowax, Renfert GmbH, Gemany) was done on 11 and 21 and the width of 11 and 21 was increased by 1mm each by adding inlay wax on mesial sides of both the teeth which closed the diastema by 2mm.(Fig 4). Remaining 2mm of diastema was closed by further adding inlay wax on mesial sides in such a way that the mesial line angles of both 11 and 21 did not further shift towards the midline, which would otherwise affect aesthetics by changing the proportionality of anterior teeth.(Fig 5). Splinting of the incisors was avoided and emergence profile was maintained to allow space for the interdental papilla to regrow. Protrusive and laterotrusive guidance was assessed such that there was uniform distribution of forces on all the teeth and not on the restoration alone. A putty index (Aquasil, Dentsply, Detrey GmbH,Germany) of the wax-up was used as a guide for the composite build up. Shade selection was done using a (VITA Tooth guide 3D Master) under natural day light. Mesial surface of both the central incisors were roughened using a diamond point. Standard etching and bonding protocol was followed. Incremental layering of direct composite resin restorative material (Venus composites, Heraeus Kulzer, UK) was done on both 11 and 21. Body composite, enamel and translucent shade composites were used in accordance with the enamel gloss and translucency of the adjacent anterior teeth. The index was used throughout the composite build-up procedure. A dental floss was passed between two teeth to confirm the interdental space and embrasure was maintained to allow the inter-dental papilla to grow. Finishing and polishing was done using composite polishing kit (Shofu Inc, Kyoto, Japan) to achieve esthetically pleasing diastema closure (Fig 6 & 7).
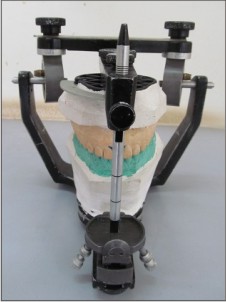 | Figure 3. Hanau wide vue semi adjustable articulator used for doing waxup
 |
 | Figure 4. Initial waxup of 1mm width on both central incisors to reduce the diastema by 2mm
 |
 | Figure 5. Final waxup to completely close the diastema
 |
 | Figure 6. Intraoral view showing esthetically and functionally satisfactory composite resin restoration closing the diastema
 |
 | Figure 7. Extraoral view showing esthetically pleasing smile with closed diastema
 |
Oral hygiene instructions were given to the patient. Finger massaging of gingiva was advised for the mechanical stimulation of inter-dental papilla in the region of midline diastema.
Discussion
Etiology of Midline diastema is multifactorial and sometimes it can also be seen as a part of normal growth and development[2],[3]. Case reports have shown that midline diastema associated with tooth size discrepancies can be corrected by simple restorative procedures.Advances in direct bonding techniques in dentistry has popularized minimally invasive dentistry, especially in correction of smile and enhancing aesthetics. The newer composites have diverse shades and improved physical and mechanical properties[6]. Despite the availability of other treatment options, this case was treated by a least invasive approach yet esthetic demands of the patient and the long term success of the restoration was kept in mind. Clinicians have shown that a diagnostic wax mock-up followed by an index resulted in a satisfactory esthetic outcome of composite restoration [4],[7]. During wax up a customized anterior guidance is very important to protect the posterior occlusion. Dawsonstated that a proper anterior guidance should disclude the posterior teeth in all lateral and protrusive excursions. Smile design principles including golden proportion and esthetic contouring should be considered during the wax up[8], [9]. When the diastema is too wide, it is not aesthetically and functionally correct to splint the two central incisors; rather an illusion has to be created while doing the composite buildup which should not make the central incisors look wider yet diastema should be closed. This illusion is created by not shifting the line angles beyond the optimum proportionality of the anterior teeth. There is enough literature to show that direct composite restorations on anterior teeth last long enough when the aesthetic and the functional principles of the restoration are satisfactorily implemented[4], [6],[7],[8],[9],[10].
Conclusion
The concept of preservation of tooth structure along with maintenance of the health of oral tissues should be the key principle for restorative procedures. Even though direct composite restoration for diastema closure is mainly a chair side procedure, supplementary laboratory procedure to enhance the esthetics, maintain the physiology of gingival tissue and achieve the favorable anterior guidance makes the restoration more successful.
References
1. Keene HJ. Distribution of diastemas in the dentition of man. Am J Phys Anthropol 1963; 21:437-41.
2. Huang JW, Creath JC. The midline diastema: a review of its etiology and treatment. Pediatric Dentistry 1995;17(3): 171-75.
3. Gkantidis N, Kolokitha EO, Topouzelis N. Management of maxillary midline diastema with emphasis on etiology. J Clin Pediatr Dent 2008; 32(4): 265–272.
4. OteoJ. Additive Solution to Diastema Closure by a Combination of Direct andIndirect Techniques. Dentistry 2012; 2(3): 1-5
5. Fahl N, Vnini L, Milnar JK. Minimally invasivedentistry and responsible esthetics: is this a new concept? J Cosmetic Dent 2010; 25(4): 16-26
6. Peyton HJ. Direct restoration of anterior teeth: Review of the clinical technique and case presentation. Pract Proced Aesthet Dent 2002; 14(3): 203-10
7. Reshad M, Cascione D, Magne P. Diagnostic mock-ups as an objective tool for predictable outcomes with porcelain laminate veneers in esthetically demanding patients: a clinical report. J Prosthet Dent.2008; 99(5):333-9.
8. Dawson EP. Functional occlusion from TMJ to smile design. Mosby Elsevier. 2007; 152
9. KleebergerGB. Restoring the worn anterior dentition for function and aesthetics. J Cosmetic Dent 2007; 23(2): 82-92.
10. Ardu S, Krejci I. Biomimetic direct composite stratification technique for the restoration of anterior teeth. Quintessence Int 2006; 37: 167-174.
|