Introduction
New treatment philosophies with improved clinical techniques and changes in patient’s awareness of malocclusion have resulted in increased demand for orthodontic treatment. The primary motivating factor is to enhance esthetics and desire to improve dental appearance. A successful outcome of orthodontic treatment is largely influenced by the patient’s periodontal status before, during and after active treatment. Patients with periodontal problems seeking orthodontic treatment have to be assessed in an interdisciplinary fashion with orthodontist and periodontist contributing to a comprehensive treatment plan in reconstruction of the occlusion not only to prevent any further progress of the disease, but also to satisfy patient’s functional and esthetic demands. In treatment of such patients, the differences in the anatomic structure and tissue response must be considered prior to treatment.[1]
Pathological tooth migration (PTM) is defined as the change in tooth position resulting from imbalance of tooth retention forces.[2] Prevalence of PTM is 30 to 55% of periodontitis patients.[3] Degrees of migration vary from tooth to tooth, according to periodontal destruction and resultant of forces acting in the teeth.[4]
It is believed that as the periodontal disease begins, the normally tightly adapted gingival tissues loose their tonicity and swelling produces a continuous light load on the tooth surface. This destruction of periodontium along with pressure from inflamed tissues,[5] occlusal factors,[6],[7] oral habits such as bruxism,[8] tongue thrusting,[9] lip forces,[10] loss of teeth without replacement,[11] a labial frenulum,[12] gingival enlargement and iatrogenic factors,[2],[13] can cause disruption in equilibrium in tooth position causing PTM. However, according to the literature, the destruction of tooth supporting structures is the most relevant factor associated with pathologic migration.[3]
Several case reports are mentioned in the literature showing spontaneous correction of PTM after doing periodontal therapy alone, however the treatment of severe cases can be complex, time consuming and improvement is often unpredictable and multidisciplinary approach is often required.[14]
This paper describes combined periodontic and orthodontic treatment of three cases of PTM caused by severe periodontitis.
Case Report I
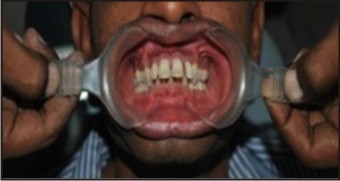
A 28 year old patient was referred to the Deptt. of Orthodontics, after periodontal treatment for severe periodontitis and PTM which included scaling and root planing, followed by periodontal flap surgeries. A period of 3months was given between the periodontal treatment and start of orthodontic treatment. On clinical examination, his maxillary anterior teeth had spaces (8mm), deep bite (80%), increased over jet (8mm), incompetent lips with lip trap with class I buccal occlusion. Patient was interested to improve his appearance but that did not improve at all 3 months after periodontal treatment.
Goal oforthodontic treatment was to retract and intrude maxillary incisors, intrude and align mandibular incisors. Position of pathologically migrated teeth only was corrected. Brackets were placed on maxillary teeth [0.22x0.28inch Mc Laughlin Bennett Trevisi (MBT)]. Alignment wires were .012 Nickel-Titanium (Ni-ti) followed by .016 Niti, .016 x.022 Niti, .016 x .022 Stainless Steel (SS). Space closure was done with very light E-chains, which were changed after every 6weeks. The first molars were continuously ligated with premolars so that it does not get heavy force. Lower bonding was done 3 months after the upper. In the lower arch, after the aligment stage, .017 x .025 Titanium Molybdenum Alloy (TMA) intrusion arch was used for leveling. After one year two months of treatment, case was debonded followed by .0175 multistranded lingual bonded retainers in both upper and lower anteriors, along with upper removable Hawley’s retainer with anterior bite plane.
Periodontal maintenance procedures consisted of oral hygiene instructions, with scaling and root planing performed at 3-month intervals and whenever necessary to prevent further progression of the disease and maintain healthy gingival tissue.
Case Report II
A 55 year old diabetic patient reported with PTM of 21. She was diagnosed with chronic periodontitis and generalized pockets. The treatment plan was periodontal therapy to eliminate cause, tooth movement for alignment of maxillary incisors followed by lingual bonded retainer.
 | Case Report 1.1
 |
 | Case Report 1.2
 |
 | Case Report 1.3
 |
 | Case Report 2.1
 |
 | Case Report 2.2
 |
 | Case Report 2.3
 |
 | Case Report 2.4
 |
 | Case Report 2.5
 |
 | Case Report 2.6
 |
With light forces, upper incisors were retracted, bite opening was done with reverse curve of spee (RCS) wires in lower arch. After achieving retraction of anteriors, anterior bite plane was given along with cross arch elastics for scissor bite correction but patient had to discontinue the treatment for personal reasons. She was given lingual bonded retainers alongwith removable Hawley’s retainer.
Case Report III
A 22 year girl patient reported with complaint of her upper teeth coming outward. On examination it was found that the maxillary incisors were flared and extruded with spaces and deep bite. 27 and 37 were in scissor bite. Apart from malocclusion patient had periodontal pockets in both upper and lower anteriors. Periodontal treatment included scaling and root planing which was followed by flap surgeries of the isolated areas. Following a healing period of 3 months fixed orthodontic treatment was rendered. Hawley’s retainer along with lingual bonded retainers were given.
Periodontal maintenance visits were planned at intervals of 3months.
 | Case Report 3.1
 |
 | Case Report 3.2
 |
 | Case Report 3.3
 |
 | Case Report 3.4
 |
 | Case Report 3.5
 |
 | Case Report 3.6
 |
Discussion
The longR09;term successful outcomes of orthodontic treatment are influenced by the patient’s periodontal status before, during and after active orthodontic therapy. Prior to start of orthodontic treatment in periodontally compromised patients, treatment should be aimed not only to allow any further progress of periodontal disease and but also to free the periodontium from active inflammatory sources. A clinician should assess each patient for periodontal factors that can develop periodontal disease and should monitor carefully who has had periodontal disease before to prevent any outbursts of active disease.
The localized loss of periodontal attachment in patients can present with varying degrees of over eruption, tipping, rotations, migration, and spacing commonly in anteriors with increase in pocket depth. Once this malocclusion has occurred, the traumatic occlusion can further cause breakdown of the periodontal tissue making brushing procedure difficult thereby failing to remove plaque, thus aggravating the periodontal destruction. However, if alveolar bone loss has not yet occurred, it is wise to start periodontal treatment at earliest to prevent spreading of inflammation further into supporting tissues. Force applied on such infected tooth can result in more periodontal breakdown. These teeth are defencelss to bacterial infection and regeneration in such teeth is hindered.[15],[16]
In treatment of such cases, factors to be considered are as follows:
Controlling periodontal disease
Reducing force magnitude
Producing higher moment to force ratio for more translator/Bodily movements.[17]
According to Melson et al (1989) the combination of orthodontic and periodontal treatment can induce generation of new attachment if the patient can maintain good oral hygiene[18]. Brunsvold et al (1997) have reported spontaneous recovery of PTM with only periodontal treatment attributed to elimination of inflammation, regeneration of fresh collagen, reduction of vascular engorgement of tissue and control of bacterial infections.[19]
Conclusion
Orthodontic treatment is no longer a contraindication when bone loss has occurred because of periodontal disease. Periodontally compromised patients can be treated with fixed appliances provided health of periodontal tissues is maintained and mechanics involves use of light forces. A systematic multidisciplinary Orthodontist – Periodontist approach in treating such periodontally compromised patient has not only given analternative to replacement of infected teeth but also hascontributed to promotion of oral health to improve the possibilities of saving and restoring a compromised dentition.
References
1. Kyomen S, Tanne K. Influences of aging changes in proliferative rate of PDL cells during experimental tooth movements in rats. Angle Orthod 1997;67:67R09;72.
2. Chasens A. Periodontal disease, pathologic tooth migration and adult orthodontics. N Y J Dent 1979;49:40-43.
3. Towfighi PP, Brunsvold MA, Storey AT, Arnold RM, Willman DE, McMahan CA. Pathologic migration of anterior teeth in patients with moderate to severe periodontitis. J Periodontol 1997;68:967-972.
4. Melsen B, Agerbaek N. Orthodontics as an adjunct to rehabilitation. Periodontol 2000 1994;4:148-159.
5. Carranza FA Jr. Occlusal trauma. In: Glickman I, Carranza FA Jr (eds). Glickman’s Clinical Periodontology, ed 7. Philadelphia: WB Saunders, 1990:284–306.
6. Southard TE, Behrents RG, Tolley EA. The anterior component of occlusal force. Part 1. Measurement and distribution. Am J Orthod Dentofacial Orthop 1989;96: 493–500.
7. Southard TE, Behrents RG, Tolley EA. The anterior component of occlusal force. Part 2. Relationship with dental malalignment. Am J Orthod Dentofacial Orthop 1990; 97:41–44.
8. Bhaskar SN, Frisch J. Occlusion and periodontal disease. Int Dent J 1967;17: 251–266.
9. Melsen B, Stensgaard K, Pedersen J. Sucking habits and their influence on swallowing pattern and prevalence of malocclusion. Eur J Orthod 1979;1:271–280.
10. Moyers RE. Orthodontic techniques. In: Moyers RE (ed). Handbook of Orthodontics, ed 4. Chicago: Year Book Medical, 1988:546–551.
11. Dersot JM, Giovannoli JL. Posterior bite collapse. 1. Etiology and diagnosis. J Parodontol 1989;8:187–194.
12. Dewel BF. The labial frenum, midline diastema, and palatine papilla: A clinical analysis. Dent Clin North Am 1966;3:175–184.
13. Guilbert PN, Rozanes SD, Tecucianu JF. Periodontal and prosthodontic treatment for patients with advanced periodontal disease. Dent Clin North Am 1988;32: 331–354.
14. Cirelli JA, Cirelli CC, Holzhausen M, Martins LP, Brandao CH. Combined Periodontal, Orthodontic and Restorative Treatment of Pathological Migration of Anterior Teeth: A Case Report. The International Journal of Periodontics & Restorative Dentistry 2006;26(5):501-506.
15. Wennstrom JL, Stokland BL, Nyman S, Thilander B. Periodontal tissue response to orthodontic movement of teeth with infrabony pockets. Am J Orthod Dentofacial Orthop 1993;103:313R09;9.
16. Nakamura Y, Tanaka T, Noda K, Shimpo S, Oikawa T, Hirashita A, et al. Calcification of degenerating tissues in the periodontal ligament during tooth movement. J Periodont Res 2003;38:343R09;50.
17. Burstone CJ, Pryputniewiczr RJ. Holographic determination of centres of rotation produced by orthodontic forces. Am J Orthod 1980;77:396R09;409.
18. Melsen B, Agerbaek N, Markenstam G. Intrusion of incisors in adult patients with marginal bone loss. Am J Orthod Dentofacial Orthop 1989;96:232-41
19. Brunsvold MA, Zammit KW, Dongari Al. Spontaneous correction of pathologic migration following periodontal therapy. Int J Periodontics Restorative Dent 1997;17:182-189.
|