Introduction
Myositis ossificans (MO) is a rare disease in which ossification develops in the muscle or soft tissue. MO is divided broadly into myositis ossificans progressiva (MOP) and myositis ossificans traumatica (MOT). MOP is an autosomal dominant disease in which multiple, heterotopic ossifications develop in the systemic muscle, fascia, tendons, and ligaments, sometimes within families.[1],[2] In many cases, MOP occurs in childhood, and the range of motion of the joints gradually becomes restricted, leading to ankylosis. The patient may die of pulmonary complications due to difficulty of movement of the respiratory muscles by 35 to 40 years of age. MOT, also called traumatic myositis ossificans, myositis ossificans circumscripta, localized myositis ossificans, or fibrodysplasia ossificans circumscripta, is a disease in which muscles are ossified after trauma or inflammation. Traumatic myositis ossificans is a benign ossifying pseudotumor mainly found in the extremities of young patients. It is rare in the craniofacial region and there are only few reports on this lesion having occurred in the temporal muscle. Most cases (70%) had a history of local trauma prior to appearance of this lesion. It is reactive in nature, is a self-limiting process and its early stages are easily confused with osteogenic sarcoma.[1] Myositis ossificans traumatica (MOT) is a benign condition involving heterotopic bone formation in muscle as the result of single or repetitive injury. The mechanism of development of MOT is assumed to involve proliferation of the mesenchymal tissue and metaplasia of the fibrous tissue that cause ossification after bleeding from trauma and myonecrosis, but the details are unknown.[3]
Case Report
A 25-year-old man was referred to department of oral and maxillofacial surgery having chief complaint of limited mouth opening. He suffered from a severe trauma 8 weeks ago, that required open reduction and internal fixation of facial fractures. Since then he had a progressive diminution of the mouth opening. Physical examination revealed maximum incisal opening (MIO) of 9 mm and deviation to right side. Radiographic evaluation revealed presence of miniplates in left frontozygomatic, left infraorbital and mandibular symphyseal region. There was no other finding in the radiographs which could define cause of limited mouth opening. The patient was placed on combination of tizanidine-2mg, paracetamol-500 mg & aceclofenac-100 mg two times a day and started on physiotherapy using tongue blades. At this point the preliminary diagnosis was muscle trismus/soreness. The patient’s opening continued to be limited to 8-10 mm after a week. Then patient was manipulated under intravenous sedation, each time showing immediate but temporary improvement in his maximal incisal opening (MIO) of 25 to 30 mm. Despite this increase in MIO, it progressively returned to 8 to 10 mm within 4 to 5 days of manipulation. After about 10 weeks of first manipulation the patient’s MIO further decreased to 4 mm, with deviation to the right side upon protrusion. Based on history and clinical examination provisional diagnosis of myositis ossificans of left temporalis muscle was made. Intraoral coroniodecetomy was done. Intraorally exposed site revealed an abnormally thick and hard temporalis muscle over the cronoid process. The sample was sent for histopathological examination which was consistent with the provisional diagnosis of myositis ossificans of temporalis muscle. Microscopically, Fig. 1 shows areas of hyalinization of collagen fibers (1) along with areas showing ossification (2) of connective tissue. (Haematoxylin and eosin, 4X) and Fig. 2 shows areas of ossification of striated muscle(3) and connective tissue (4) (Haematoxylin and eosin, 20X). Immediate post operative mouth opening was 38mm. Patient was kept on physiotherapy using tongue blades for about one month. Six months post operatively patients mouth opening remained 38mm with no deviation.
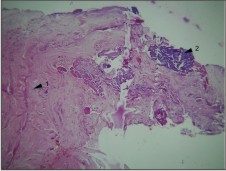 | Fig 1 : Areas Of Hyalinization Of Collagen Fibers (1) Along With Areas Showing Ossification (2) Of Connective Tissue Are Seen. (Haematoxylin And Eosin, 4x)
 |
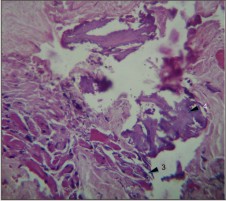 | Fig 2 : Areas Of Ossification Of Striated Muscle (3) And Connective Tissue (4) Are Seen. (Haematoxylin And Eosin, 20x)
 |
Discussion
Myositis ossificans is a disease whose hallmark feature is the ossification in muscle or soft tissue. Broadly, Myositis ossificans diseases (MO) can be classified into 2 forms; myositis ossificans progressive (MOP) and myositis ossificans traumatic (MOT). MOP, is an autosomal dominant disease mesodermal disorder of connective tissue. MOT is rare in the head and neck region, with little more than 50 reported cases, usually affecting the masseter. The major clinical finding is a progressive limitation of motion in the mandible.[2],[3] Although MO is the most common extraskeletal bone-forming lesion, it most commonly involves larger muscles of the legs, but is rarely reported in the muscles of mastication.[4] Furthermore, fewer than 30 cases involving the muscles of mastication have been reported in the literature.[5],[6],[7],[8] Approximately two thirds of these cases involve the masseter muscle, likely because of its repetitive motion during mastication and inherent superficial location, leading to an increased vulnerability to trauma. Furthermore, there are only 5 reported cases in the literature of temporalis muscle involvement. Also unique to this case is the lack of a specific traumatic event that set this reactive process into action. Reports have shown that in as many as 25% of cases of MOT, the patient can identify no specific triggering traumatic event. However, the patient did report a long-term, low-grade inflammation consistent with findings in a case report by Saka et al.[1] In these cases, it is important to take into account other possible etiologies, such as chronic lowgrade infections or repeated, minor, traumatic lesions. It has been reported in the literature that 2 to 4 different variations of MO exist, with MOT and MO progressive (MOP) being the most prominent. The 2 other types cited include atraumatic MO and a specialized variation seen in individuals with neurologic disease. Although the 2 major entities, MOT and MOP, are similar in that they produce an extraskeletal ossification, the pathophysiology, treatment, and prognosis differ significantly. The pathophysiology, as described by Marx and Stern[3], involves the exposure of perivascular mesenchymal cells to bone morphogenic protein. This sentinel event, in the muscles of mastication, may include traumatic etiologies, such as dental extractions, local anesthetic infiltrations, and repeated localized infections. MOT has a relatively good prognosis, unlike MOP, and responds well to complete surgical excision. Surgical excision followed by aggressive physical therapy consistently provides a long-term stable result. The final maximal incisal opening is typically about two thirds to three fourths that of normal. In contrast, MOP is an autosomal dominant genetic condition with manifestations of calcifications throughout the body.[7] Pathologically, these calcifications entail the conversion from fibrous cellular proliferation through the stages of endochondral ossification into mature lamellar bone. This presentation is most commonly seen in preteens and teenagers. These patients characteristically exhibit a stiff gait and severe limited mandibular motion. As MOP progresses, ossification ultimately can involve the intercostal muscles, leading to labored breathing and subsequent respiratory failure, thus a source of decreased longevity in this patient population.[7] The exact mechanism for pathogenesis is unclear, but trauma is universally recognized as the trigger. Carey [8] reported 4 main theories, 1) Displacement of bony fragments into the soft tissue and hematoma with subsequent proliferation, 2) detachment of periosteal fragments into the surrounding tissue with proliferation of osteoprogenitor cells, 3) migration of subperiosteal osteoprogenitor cells into surrounding soft tissue through periosteal perforations induced by trauma, and 4) differentiation of extraosseous cells exposed to bone morphogenic protein (BMP). The last theory is the most widely accepted. Thoma [5] in 1958, theorized that MOT results from calcification and progressive ossification of an intramuscular hematoma after trauma. Tweeddale et al [9] attempted but failed to induce MOT in rats in 1957. Urist [10] had success in the production of ectopic osteogenesis by transplantation of decalcified bone fragments into ordinary connective tissue. The explanation of Urist’s result is the following: some bone fragments scattering into adjacent muscle or hematoma after trauma. Autolysis of the scattered bone fragments causes a release of the BMP, inducing the differentiation of the primitive perivascular mesenchymal cells into the muscular tissue, resulting in a relatively homogenous bony mass.[11] Aro et al [12] studied inflammatory cell reaction in rabbits after an injury. They found that microinjury and subsequent muscle necrosis caused an invasion of macrophages and release of osteogenic growth factors. Diagnosis is difficult and is often confused with osteosarcoma. An accurate history & biopsy is essential, as up to 75% of the cases have a history of direct trauma. In diagnostic imaging, ossification is difficult to detect in many cases in plain radiography because it is superimposed on the cranial bones. Some cases that require differentiation from osteogenic tumors, CT may be useful. Imaging by 3-dimensional CT provides a better view of the shape and position of the ossification, which may be more useful in planning operations as well as in diagnosis. Although some reports revealed the usefulness of MRI. No laboratory abnormalities have been linked to MOT. The differential diagnosis for bone forming lesions includes MO, nodular fascitis, juxtacortical osteoma, osteochondroma, osteoblastoma, chondroma, sarcoma, chondrosarcoma, and a venous hemangioma with multiple phleboliths.[13],[14] Osteochondromas, when occurring in the head and neck region, occur predominantly on the condylar head and coronoid process. The key differentiation between osteochondroma and MO is the presence of cartilaginous capping of the lesion, which was absent from the specimen in the present case. Also, osteochondromas are most commonly seen in young individuals (average age, 22 yr). Chondromas are purely cartilaginous, with little to no calcification clinically or radiographically. Sarcomas and chondrosarcomas, owing to their malignant behavior, will show extension into and destruction of surrounding structures. Often, this leads to paresthesias and lymph node involvement. Also, osteosarcomas most frequently arise from an intramedullary, not juxtacortical, origin.[15],[16] The region where MOT most frequently occurred was the masseter muscle, which may be attributed to the fact that the masseter muscle is on the outside of the mandible and is likely to receive external force directly.[17],[18] Many MOT lesions in the medial pterygoid muscle were caused by local anesthesia injection of the mandibular foramen, pericoronitis of the mandibular third molars may also play a role in the etiology of MOT of the medial pterygoid[19]. Most MOT lesions in the lateral pterygoid muscle or the temporal is muscle developed simultaneously with lesions in other muscles. In many cases, the lesions are detected as abnormal calcification in radiographs obtained at the time of the postoperative follow-up. Typical histologic findings of MO includes the zone phenomenon composed of the inner zone consisting of undifferentiated cells and hemorrhagic and necrotic muscular tissue; the middle zone consists of osteoblasts and immature osteoid formation, and the outer zone consists of a mature bone with collagenous fibrous stroma. The histologic features of the ossification of our patient included areas of ossification of striated muscle and connective tissue. All cases of reported MOT, with the exception of two, have shown normal laboratory values of calcium, alkaline phosphatase, phosphorus, ionized calcium, parathyroid hormone, and growth hormone.[20] The two cases reported by Mulherin and showl[21] and Nizel and Priggel[22] showed elevated serum alkaline phosphatase levels. Elevated alkaline phosphatase levels seem to occur during evolution of MOT as a result of progress of the disease. Treatment of MOT of the head and neck is usually accomplished via surgical excision. MOT of the masticatory muscles usually requires early intervention due to pain and trismus. Alternatively non-surgical treatment in combination with surgical excision of the calcified mass, may be useful[6] Steidl and Ditmar[7] used local injections of magnesium sulfate and oral administration magnesium lactate under the theory that the hypermagnesemia may retard development of calcifications, and reported a 74% cure rate. In addition, low-dose radiation, non steroid antiinflamatory drugs, biphosphonates, corticosteroids, indometacin, warfarine and retinoids are others alternatives attempted in MO treatment. Treatment options for MOT in the literature are variable, with the one constant being complete surgical excision for a localized lesion followed by aggressive physical therapy.[23],[24] One of the most challenging aspects is obtaining accurate diagnosis as to the cause of progressive limited opening, pain, and possible swelling. Periodic CTs every 2 to 3 months can be used to evaluate the progression and confirm the cessation of the ossification process.[3] Early management with home physiotherapy instituted little benefits. It is important that the patient and family members understand that myositis ossificans traumatica is a very rare clinicopathological entity and that early interventions should be done to prevent the disease.
Acknowledgements: A special thanks to Dr. Prof. Nageshwar Iyer, Dean & Principal , for providing constant encouragement.
Ethical approval: Not required
References
1. B. Saka, G. Stropahl, K. K. H. Gundlach. Traumatic myositis ossificans (ossifying pseudotumor) of temporal muscle. Int. J. Oral Maxillofac. Surg. 2002; 31: 110–111.
2. Sarac A, Sennaroglu L, Hosal A, Sozeri B. Myositis ossificans in the neck. Eur Arch Otorhinolaryngol 1999:256:199-201.
3. Conner GA, Duffy M. Myositis ossificans: a case report of multiple recurrences following third molar extractions and review of the literature. J Oral Maxillofac Surg 2009: 67: 920–926.
4. Thangavelu A., Vaidhyanathan A., Narendar R.Myositis ossificans traumatica of the medial pterygoid Int. J. Oral Maxillofac. Surg. 2011; 40: 545–558.
5. Thoma KH: Oral Surgery (3rd ed). St. Louis, MO, Mosby, 1958, p 1568
6. Manzano D, Silván A, Saez J, Moreno J. Myositis Ossificans of the temporalis muscle. Case report. Med Oral Patol Oral Cir Bucal 2007;12:E277-80.
7. Steidl L, Ditmar R: Treatment of soft tissue calcifications with magnesium. Acta Univ Palacki Olomuc Fac Med 130: 273, 1991.
8. Carey EJ: Multiple bilateral parosteal bone and callus formations of the femurs and left innominate bone. Arch Surg 8:592, 1924
9. Tweeddale DN, Higgins GM, Wakim KG: Attempts to produce myositis ossiticans in the rat. Lab Invest 6:346, 1957
10. Urist MR: Bone: Formation and autoinduction. Science 150:893, 1965
11. Arirna R, Shiba R, Hayashi T.Traumatic myositis ossificans in the masseter muscle. J Oral Maxillofac Surg. 1984 Aug;42(8):512-526.
12. Aro HT, Viljanto J, Aho HJ, et al: Macrophages in traumainduced myositis ossificans. APMIS 99:482, 1991.
13. Mevio E, Rizzi L, Bernasconi G: Myositis ossificans traumatica of the temporal muscle: A case report. Int J ORL Head Neck Surg 28:345, 2001
14. Dhanrajani P, Jonaidel O: Trismus: Aetiology, differential diagnosis and treatment. Dent Update 29:88, 2002
15. Aoki T, Naito H, Ota Y, Shiik K: Myositis ossificans traumatica of the masticatory muscles: Review of the literature and report of a case. J Oral Maxillofac Surg 60:1083, 2001 8.
16. Aliko A, Ciancaglini R, Alushi A, et al: Temporomandibular joint involvement in rheumatoid arthritis, systemic lupus erythematosus and systemic sclerosis. Int J Oral Maxillofac Surg 40:704, 2011
17. Uematsu Y, Nishibayashi H, Fujita K, et al: Myositis ossificans of the temporal muscle as a primary scalp tumor. Neurol Med Chir (Tokyo) 45:56, 2005 13.
18. Rattan V, Rae S, Vaiphei K: Use of buccal pad of fat to prevent heterotopic bone formation after excision ofmyositis ossificans of the medial pterygoid muscle. J Oral Maxillofac Surg 66:1518, 2008
19. Debency-Bruyerre C, Chikhani L, Lockhart R, et al: Myositis ossificans progressiva: Five generations where the disease was exclusively limited to the maxillofacial region. Int J Oral Maxillofac Surg 27:299, 1998
20. Goodsell JO: Traumatic myositis ossificans of the masseter muscle: Review of the literature and report of a case. J Oral Surg Anesth Hosp D Ser 20: 116, 1962
21. Mulherin D, Schow CE: Traumatic myositis ossiticans after genioplasty. J Oral Surg 38:786, 1980
22. Nizel A, Prigge EK: Trismus due to myositis ossifmans traumatica: Report of a case. J Oral Surg 4:93, 1946
23. Conner JM, Skirton H, Lunt PW: A three generation family with fibrodysplasia ossificans progressiva. J Med Genet 30:687, 1993
24. Gilmer WS, Anderson LD: Reactions of soft somatic tissue which may progress to bone formation: Circumscribed (traumatic) myositis ossificans. South Med J 52:1432, 1959
|