Introduction
Traumatic dental injuries (TDI) is a significant problem in children and adolescents and its incidence is likely to exceed in the coming years due to high levels of violence, traffic accidents, and greater participation of children in sports. Dental injuries result in functional, esthetic and psychological disturbances accompanied by great concern from the child and parent.[1] Social activities such as speaking, laughing and overall confidence can be negatively affected by such injuries.[2],[3],[4] At the same time, treatment of TDIs and the short- or long-term disruption they cause may be financially burdensome.[5] Since the majority of these injuries are preventable, therefore understanding the factors which predispose a tooth to fracture is an essential for developing a concept of prevention.
Traumatic dental and maxillofacial injuries affect worldwide approximately 20 to 30% of the permanent dentition. More than 20% of children experience damage to their permanent dentition by 14 years of age, with men outnumbering women with ratio of 2:1 and peak incidence at 10 years of age. Most injuries occur as a result of falls, during playing, trauma from traffic accidents, risk taking activities, contact sports and violence. Child physical abuse has also been reported as the cause of TDI.[6]
Keeping these factors into consideration, the present study was planned to assess the prevalence, etiology as well as predisposing factors of TDI in children of the region from various schools in and around Baddi, Himachal Pradesh.
Materials and Methods
Sample Selection
A cross-sectional study was carried out on 1000 children (552 boys and 448 girls) in the age range of 7 to 10 years, who were enrolled in 8 private and government schools within 10 km radius from Bhojia Dental College and Hospital, Baddi, Himachal Pradesh. The children examined belonged to the middle- and low-income groups. A letter was sent to the Principals of schools explaining the aim, characteristics, and importance of the study who in turn took permission from parents of the children.Ethical clearance was obtained from the Ethical board committee of the institute. Only the children having consent forms duly signed by the parents were included in the study. Children with any special health care needs or who were physically, mentally and emotionally disturbed were excluded from the study. Those subjects who showed clinical evidence of trauma but could not give a proper history were also excluded from the study.
Clinical examination
The examination was performed in the schools under natural day light, with the aid of mouth mirrors and disposable tongue depressors. The intraoral clinical examination was carried out by a trained single examiner while atrained assistant was made to sit close enough to the examiner to record the data and thefindings were noted on a specially designed proforma. The recording procedure was standardized by repeated session of calibrations between the examiner and supervisor before the actual examination. Social and demographic factors were noted and chronological age as mentioned in school records was the criterion for deciding the age group.
The teeth were dried with cotton before examination to increase the accuracy of the diagnosis. The examination was conducted in a uniform fashion beginning from the maxillary right quadrant to the mandibular in a clockwise direction. Only objective findings at the time of examination were registered as traumatic dental injuries. The data registered were: age, gender, type of injury, tooth involved and treatment taken. Various intrinsic and extrinsic risk factors were recorded such as upper lip coverage, lip seal, over jet, molar relation and cause of injury.
Injuries to permanent teeth were categorized according to classification by Ellis & Davey (1960).[7] This classification has been used earlier in numerous studies for recording TDI and study did not evaluate injuries to the alveolar socket and fractures of the jaws or laceration of the gingival or oral mucosa, and preferred to use this simple classification instead of Andreasen's classification. However, type VI injury was not recorded as dental radiographs were not available for diagnosis in the in-school field conditions.[7]
The proclination or overjet was measured using metallic scale where scale was trimmed from the front edge so that the measurements starts from the calibrations present on the scale. Scale was kept horizontally starting from the labial surface of lower incisors and the distance was measured in millimeters. Lip seal and upper lip coverage were evaluated as by Sutcliff (1968)[8] and Addy et.al. (1987),[9] respectively.
Statistical Analysis
The data were subsequently processed and analyzed using the SPSS statistical Software program. The Chi – Square was employed tofind the significance of the cross-tabulation of counts of two or more variables.
Results
This cross-sectional survey identified the overall prevalence of TDI to the anterior teeth to be 5.1%. The involved gender percentage was higher and approximately two times in boys (6.5%) than in girls (3.3 %) and the difference was statistically significant (p<0.05). Maxillary arch was involved in 96.1% of cases. 84.3% of the subjects had only one tooth involved, two teeth were involved in 13.7% and three teeth were involved in 2% cases. The tooth most prone to trauma was permanent maxillary central incisors in approximately 96 % of cases,out of which the permanent right maxillary central incisor accounted for 55 % of the injuries followed by the permanent left maxillary central incisor with 36.66%.Maximum number of subjects i.e.78.4% had Ellis class I fracture followed by 11.8% subjects with class II fracture, 7.8% subjects showed class III fracture and only 2% of subjects had class IV fracture.
Ten years old children experienced maximum TDI in the selected age range (Figure1). The causative factors of TDI presented a wide range, with falls while playing contributing significantly higher number among all the injuries (Figure2). Predisposing factors such as upper lip coverage, lip seal, overjet and molar relationship also showed varied results as shown in Table-1. None of the subject involved in study had seeked treatment for TDI.
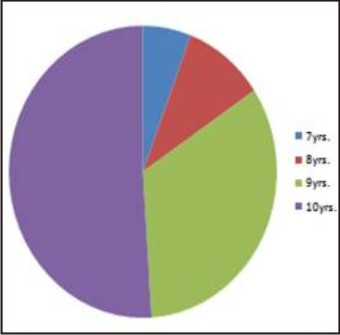 | Fig. 1 : Distribution Of Injuries According To Age Of Children
 |
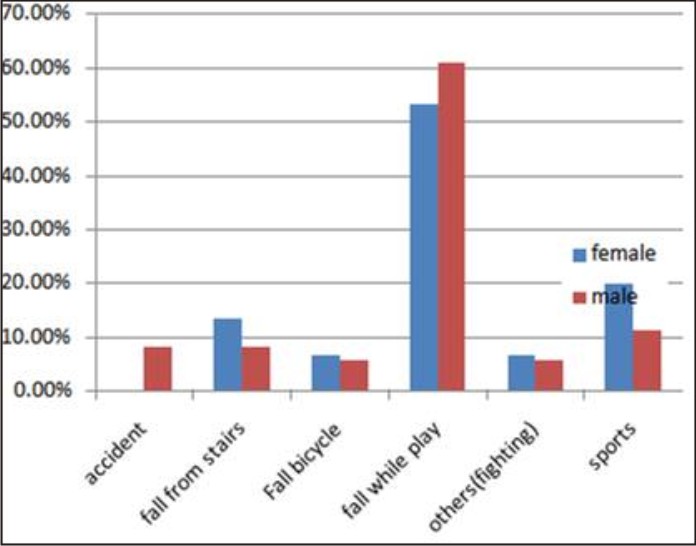 | Fig. 2 : Causes Of Injuries
 |
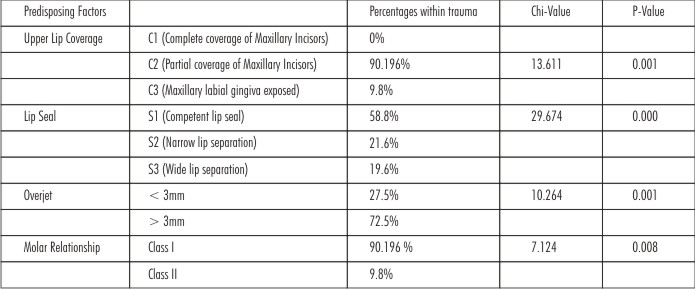 | Table 1 : Predisposing Factors
 |
Discussion
Traumatic dental injuries in children and adolescents have been reported in different parts of the world.[10],[11],[12],[13]Variation in prevalence has been related to many factors, such as type of study, trauma classification, sample and diagnostic criteria, limited age groups, and geographic and behavioral differences between study locations and countries.[14]
The present survey identified the overall prevalence of TDI to the anterior teeth among school children aged 7 to 10 years to be 5.1 %. The results were similar to studies conducted by Gupta S et al. on school children in Baddi-Barotiwala region, Himachal Pradesh.[15] However, the prevalence was relatively less as compared to neighboring state like Punjab. Trauma to anterior teeth in the Asia-Pacific region ranged from 6% to 19%.[16] The prevalence of TDIs among adolescents in the America and Europe ranged from 15 % to 23% and 23% to 35%, respectively.[17],[18] This can be explained by the observations of lack of playgrounds in the hilly area like Himachal Pradesh.
Our finding of a greater frequency of TDI in boys than in girlsi.e. 2:1 corroborates the findings by Altun,[12] Cavalcanti,[19] David,[10] Dua and Sharma.[20] This might be explained by observations that boys participate in more aggressive type of games and contact sports. Also, the girls are less prone to TDI as the Indian social set up is overprotective thus not allowing them to be liberally involved in vigorous outdoor activities.
Falls(58.8%) was the main cause of injury in the present study, which was in accordance with Rai and Munshi,[7],[21],[22],[23],[24] Dua and Sharma[20] and Shipra et al,[15] which can be explained by the fact that age range chosen for the study was most commonly involved in playing and sports activities.
The present study showed predilection for maxillary teeth over the mandibular teeth to TDI which is generally supported by the existing literature.[20] The most frequently affected teeth were maxillary central incisor which was found to be similar with the studies done by Ozen B, David J, Ferreira JMS, Dua and Sharma.[15]This probably relates to the vulnerable position of the maxillary central incisors. In addition, these teeth are frequently protruded and may have inadequate lip coverage. The most common type of injury noted was class I fracture. This was in accordance with earlier studies.[1], [20]
In this study, cases with Class I type 1 molar relation, exhibited large number of the traumatic injuries which is in contrary to other studies showing the predilection of patients with Class II div 1more prone to dental trauma.[20]
This study showed a significant association between the presence of dental trauma and overjet. Individuals with overjet greater than or equal to 3 mm were more at risk compared to individuals who had less than 3mm, corroborating the assertion that the frequency of dental trauma increases proportionally in relation to an increased overjet. Also increased overjet means increased exposure of teeth which predisposes to trauma. The relationship between overjet and dental traumatic injury has been investigated by different authors. Previous studies by Altun[12] and Cavalcanti[19] showed that individuals with an overjet greater than 3 mm were two and a half times more at risk compared with individuals who had a normal overjet.
A large number of children who sustained accidental damage to their maxillary incisors in this study had incompetent lips i.e lips with S2 and S3 categories. This could be due to the fact that lips cushion the impact of colliding materials with anterior teeth thus minimizing the possibility of a fracture. Similarly children with inadequate lip coverage i.e.C2 (90.2%) andC3 (9.8%) were more likely to have TDI than children with C1 category.Hence, inadequate upper lip coverage and lip competence was identified as the most important and an independent risk predictor for traumatic injuries to permanent anterior teeth.
None of the cases of traumatized teeth had undergone treatment. This indicates a low level of awareness among the parents about the importance of treatment. Another reason could be that on suffering any injury, the people usually rush to a nearby medical practitioner or hospital where dentists are not available or else the fear of the dentist keep them away. Socioeconomic status of the patients also may be an other factors, due to which people do not seek immediate dental treatment.
Conclusion
Fall still remains the leading cause of TDI, the role of sport and violence cannot be neglected in the etiology of TDIs. There is a need to implement educational and preventive strategies aimed at minimizing the menace of fall, sport and violence related accidents and the benefits of seeking immediate treatment of fractured teeth. Children should be supervised while they are playing to minimize the rate at which they fall and sustain TDIs and use of mouth guards is also recommended for children who are participating in contact sports. Further studies on a larger sample are recommended. Also, the interruptive strategies should be implemented with the aim of providing effective dental care in the public health set up to the children with TDI.
References:
1. Ingle NA, Naveen B, Zohar C.Prevalence and Factors Associated with Traumatic Dental Injuries (TDI) to Anterior Teeth of 11-13 Year Old School Going Children of Maduravoyal, Chennai J Oral Health Comm Dent. 2010;4(3):55-60.
2. Trabert J, Peres MA, Blank V, Böell Rda S, Pietruza JA. Prevalence of traumatic dental injury and associated factors among 12-year-old school children in Florianópolis, Brazil. Dental Traumatol. 2003;19:15-8.
3. Cortes MIS, Marcenes W, Sheiham A. Impact of traumatic injuries to the permanent teeth on the oral health-related quality of life in 12-14-years-old children. Community Dent Oral Epidemiol. 2002;30:193-8.
4. Soriano EP, Caldas Ade F Jr, Diniz De Carvalho MV, Amorim Filho Hde A. Prevalence and risk factors related to traumatic dental injuries in Brazilian schoolchildren. Dent Traumatol. 2007;23:232-40.
5. Levin L, Samorodnitzky GR, Schwartz-Arad D, Geiger SB. Dental and oral trauma during childhood and adolescence in Israel: occurrence, causes, and outcomes. Dent Traumatol. 2007;23:356-9.
6. Gutmann JL, Gutmann MS. Cause, incidence and prevention of trauma to teeth. Dent Clin North Am1995;39:1-13.
7. Rai SB, Munshi AK. Traumatic injuries to the anterior teeth among South Kanara school children--a prevalence study. J Indian Soc Pedod Prev Dent. 1998;16:44-5.
8. Sutcliffe P. Chronic anterior gingivitis. An epidemiological study in school children. Br Dent J. 1968; 125: 47-55.
9. Addy M, Dummer PMH, Hunter ML, Kingdom A, Shaws WC. A study of the association of fraenal attachment, lip coverage and vestibular depth with plaque and gingivitis. J Periodontol.1987; 58: 752-757.
10. David J, Astrøm AN, Wang NJ. Factors associated with traumatic dental injuries among 12-year-old schoolchildren in South India. Dent Traumatol. 2009;25:500-5.
11. Adekoya-Sofowora CA, Adesina OA, Nasir WO, Oginni AO, Ugboko VI. Prevalence and causes of fractured permanent incisors in 12-year-old suburban Nigerian schoolchildren. Dent Traumatol. 2009;25:314-7. JIJ;’
12. Altun C, Ozen B, Esenlik E, Guven G, Gürbüz T, Acikel C, et al. Traumatic injuries to permanent teeth in Turkish children, Ankara. Dent Traumatol. 2009;25:309-13.
13. Ferreira JM, Fernandes de Andrade EM, Katz CR, Rosenblatt A. Prevalence of dental trauma in deciduous teeth of Brazilian children. Dent Traumatol. 2009;25:219-23.
14. Glendor U. Aetiology and risk factors related to traumatic dental injuries-a review of the literature. Dent Traumatol. 2009;25:19-31.
15. Gupta Shipra ,Jindal SK, Bansal Mohit, Singla Anshu. Prevalence of traumatic dental injuries and role of incisal overjet and inadequate lip coverage as risk factors among 4-15 years old government school children in Baddi-Barotiwala Area, Himachal Pradesh, India.Med Oral Patol Oral Cir Bucal. 2011;16 (7):960-5.
16. Dearing SG. Overbite, overjet, lip-drape and incisor tooth fracture in children. N Z Dent J. 1984;80:50-2.
17. Marcenes W, Alessi ON, Traebert J. Causes and prevalence of traumatic injuries to the permanent incisors of school children aged 12 years in Jaraguá do Sul, Brazil. Int Dent J. 2000;50:87-92.
18. Soriano EP, Caldas AF Jr, Góes PS. Risk factors related to traumatic dental injuries in Brazilian schoolchildren. Dent Traumatol. 2004;20:246-50.
19. Cavalcanti AL, Bezerra PK, de Alencar CR, Moura C. Traumatic anterior dental injuries in 7- to 12-year-old Brazilian children. Dent Traumatol. 2009;25:198-202.
20. Sharma Sunila, Dua Rohini.Prevalence, causes, and correlates of traumatic dental injuries among seven-to-twelve-year-old school children in Dera Bassi.Contemp Clin Dent. 2012 Jan-Mar; 3(1): 38–41.
21. Navabazam A, Farahani SS. Prevalence of traumatic injuries to maxillary permanent teeth in 9 to 14 year old schoolchildren in Yazd, Iran.Dent Traumatol. 2009;26:154-7.
22. Rocha MJ, Cardoso M. Traumatized permanent teeth in Brazilian children at the Federal University of Santa Catarina, Brazil. Dent Traumatol 2001;17:245-49.
23. Glender ulf. Aetiology and risk factors related to traumatic dental injuries- a review of the literature. Dent Traumatol 2009;25:19-31.
24. Perez R, Berkowitz R, Mciveen L. Forrester D. Dental trauma in children: A survey. Endod Dent Traumatol 1991;7:212-13.
|