Introduction
Two-dimensional (2D) imaging modalities have been used in dentistry since the first intraoral radiograph was obtained in 1896. Since then, significant advances have been made in dental imaging techniques, including the introduction of panoramic imaging techniques and tomography. Advances in digital imaging techniques have led to lower radiation doses and faster processing times without changing the imaging geometry of these intraoral and panoramic technologies. Cone-beam computed tomography (CBCT) is a new medical imaging technique that generates three-dimensional (3D) data at lower cost and lower absorbed doses than conventional computed tomography (CT). The CBCT imaging technique is based on a cone-shaped X-ray beam that is centred on a 2D detector, and the beam performs one rotation around the object, producing a series of 2D images. The images are reconstructed in a 3D data set using a modification of the original cone-beam algorithm developed by Feldkamp et al. in 1984. CBCT images from the craniofacial region are often acquired at a higher resolution than conventional CT. In addition, these systems are more compact than conventional CT systems, which make them more practical for use in dental offices[1]. Increased access to such technology has led to CBCT scanners now finding many uses in dentistry especially in the fields of Implant Dentistry, Endodontics and Orthodontics. The application of CBCT imaging in different dental disciplines can guide diagnosis, treatment and follow-up.
This article presents a systematic review of clinical applications of CBCT in dental practice.
Review
Applications In Oral And Maxillofacial Surgery
CBCT in OMFS has been used to investigate the exact location of jaw pathology[2],[3],[4],[5],[6],[7] in 3D image , to assess impacted teeth , to assess supernumerary teeth and their relation to vital structures[3],[8],[9],[10],[11],[12],[13],[14],[15],[16] to evaluate changes in the cortical and trabecular bone related to bisphosphonate-asociated osteonecrosis of the jaws[17], and to assess bone grafts[18]. CBCT has also been used to investigate paranasal sinuses[3] and to assess obstructive sleep apnea.[19]
Because CBCT images are collected as a combination of several 2D slices, the technique is superior in overcoming superimpositions and calculating surface distances[20]. This advantage has made CBCT the technique of choice for the investigation of mid-facial fractures[5], [21] orbital fracture assessment and management[22], and in inter-operative visualization of the facial bones after fracture[23]. CBCT is largely used in planning orthognathic and facial orthomorphic surgeries[24], [25] which require detailed visualization of the interocclusal relationship to augment the 3D virtual skull model with a detailed representation of the dental surface. With the aid of advanced software, CBCT facilitates the visualization of soft tissue to allow for control of the post-treatment aesthetics) and permits the evaluation of lip and palate bony depressions in cases of cleft palate[26]. The ability of CBCT to detect salivary-gland defects is also under investigation[27]. In addition, one article has reported a tooth autotransplant case where CBCT demonstrated high accuracy, and the information provided allowed the rapid completion of the transplant operation[28].
Endodontics
CBCT is a very useful tool in diagnosing apical lesions.[12],[15],[17],[18],[29],[30],[31],[32],[33]. A number of studies have demonstrated its ability to enable a differential diagnosis of apical lesions by measuring the density from the contrasted images of these lesions, in whether the lesion is an apical granuloma or an apical cyst. [17], [32], [33]. Cotton et al.[12] used CBCT as a tool to assess whether the lesion was of endodontic or non-endodontic origin. CBCT also demonstrated superiority to 2-D radiographs in detecting fractured roots. Vertical and horizontal root fracture detection is described in several clinical cases.[12],[35],[36] It is also agreed that CBCT is superior to peri-apical radiographs in detecting these fractures, whether they are bucco-lingual or mesiodistal.[37],[38] In cases with inflammatory root resorption, lesions are detected much easier in early stages with CBCT compared to conventional 2-D X-ray.[18]. In other cases, such as external root resorption, external cervical and internal resorption, not only the presence of resorption was detected, but also the extent of it. [12], [33],[39]
CBCT can also be used to determine root morphology, the number of roots, canals and accessory canals, as well as to establishing the working length and angulations of roots and canals.[12],[32],[33],[35],[40] It also is accurate in assessing root-canal fillings.[32],[33],[41] Owing to its accuracy, it is very helpful in detecting the pulpal extensions in talon cusps and the position of fractured instruments.[42]
It is also a reliable tool for presurgical assessment of the proximity of the tooth to adjacent vital structures, size and extent of lesions, as well as the anatomy and morphology of roots with very accurate measurements.[12], [32], [33], [34], [35]
Additionally, in cases in which teeth are assessed after trauma and in emergency cases, its application can be a useful aid in reaching a proper diagnosis and treatment approach.[12],[32] Recently, owing to its reliability and accuracy, CBCT has also been used to evaluate the canal preparation in different instrumentation techniques. [43],[44]
Implantology
With increased demand for replacing missing teeth with dental implants, accurate measurements are needed to avoid damage to vital structures. This was achievable with conventional CT. However, with CBCT giving more ac curate measurements at lower dosages, it is the preferred option in implant dentistry today. [16],[45],[46],[47],[48],[49],[50],[51],[52],[53]. The advantages of CBCT in visualizing the alveolus in 3 dimensions and making precise measurements before surgery are obvious in the field of implant dentistry. With new software that constructs surgical guides, damage is also reduced further.[2],[16],[54],[55]. Heiland et al.[56] describe a technique in which CBCT was used inter-operatively in two cases to navigate the implant insertion following microsurgical bone transfer.
CBCT enables the assessment of bone quality and bone quantity.[2],[45],[46],[47] ,[51],[57],[58] This gives the surgeon the ability to anticipate implant placement and even to place implants in a virtual model in terms of bone height, bone width, nerve position and even objective measures of bone quality. This leads to reduced implant failure, as case selection can be based on much more reliable information. This advantage is also used for post-treatment evaluation and to assess the success of bone grafts [50].
Orthodontics
Orthodontists can use CBCT images in orthodontic assessment and cephalometric analysis.[46],[49] Today, CBCT is already the tool of choice in the assessment of facial growth, age, airway function and disturbances in tooth eruption.[59],[60],[61] CBCT is a reliable tool in the assessment of the proximity to vital structures that may interfere with orthodontic treatment.[62] In cases in which mini-screw implants are placed to serve as a temporary anchorage, CBCT is useful for ensuring a safe insertion [63],[64] and to assess the bone density before, during and after treatment . As the images are self-corrected from the magnification to produce orthogonal images with 1:1 ratio, higher accuracy is ensured. CBCT is thus considered a better option for the clinician.113
Orthognathic Surgery
Clinicians have long evaluated the usefulness of 3- dimensional imaging in orthodontics and orthognathic surgery, with a major concern being the correlation between soft tissue and hard tissue changes. Lateral cephalography has been the standard modality for diagnosing skeletal and dental deformities, as well as for use in surgical prediction and treatment planning. As useful as cephalometric analysis can be, its imaging accuracy is inadequate in such deformities as hemifacial microsomia, severe facial asymmetries and occlusal cant. Three-dimensional imaging of the hard and soft tissue makes all of the data available, the clinicians have to understand how best to apply and manipulate that data for more accurate surgery and treatment planning.
Temporomandibular joint disorder
One of the major advantages of CBCT is its ability to define the true position of the condyle in the fossa, which often reveals possible dislocation of the disk in the joint, and the extent of translation of the condyle in the fossa.[50],[33],[66] With its accuracy, measurements of the roof of the glenoid fossa can be done easily.[67] Another advantage of some of the available devices is their ability to visualise soft tissue around the TMJ, which may reduce the need for magnetic resonance imaging in these cases.[68] Owing to these advantages, CBCT is the imaging device of choice in cases of trauma, pain, dysfunction, fibro-osseous ankylosis and in detecting condylar cortical erosion and cysts.[46],[68]. With the use of the 3-D features, the image guided puncture technique, which is a treatment modality for TMJ disk adhesion, can safely be performed.[70]
Periodontics
CBCT can be used in assessing a detailed morphologic description of the bone because it has proved to be accurate with only minimal error margins. The measurements proved to be as accurate as direct measurements with a periodontal probe.[33],[71],[72] Furthermore, it also aids in assessing furcation involvements.[33]
CBCT can be used to detect buccal and lingual defects, which was previously not possible with conventional 2-D radiographs.[33],[73] Additionally, owing to the high accuracy of CBCT measurements, intra-bony defects can accurately be measured and dehiscence, fenestration defects and periodontal cysts assessed.[7],[33],[74] CBCT has also proved its superiority in evaluating the outcome of regenerative periodontal therapy.[73]
Operative Dentistry
Based on the available literature, CBCT is not justified for use in detecting occlusal caries, since the dose is much higher than conventional radiographs with no additional information gained. However, it proved to be useful in assessing proximal caries and its depth. [75]
Forensic Dentistry
Many dental age estimation methods, which are a key element in forensic science, are described in the literature. CBCT was established as a non-invasive method to estimate the age of a person based on the pulp–tooth ratio.[76]
Discussion
CBCT scanners represent a significant advancement in dental and maxillofacial imaging. Since their introduction for dental use in the late 1990s [77], there has been an increased interest in these devices. The number of CBCT-related articles published per year has increased tremendously over the last few years. [78]
The clinical applications of CBCT imaging in dentistry are constantly increasing. The most common clinical applications of CBCT are in OMFS, implant dentistry, and endodontics. CBCT has shown limited use in operative dentistry because of the high radiation dose compared to conventional 2D radiography without any additional benefit.
The dental literature on CBCT is promising and indicates that more research is required to explore the benefits of CBCT in forensic dentistry. Although no literature was found on Prosthodontic applications of CBCT, the improved standard of care seen in Prosthodontics treatment can be attributed to applications of CBCT found in other dental specialties and related to Prosthodontics, such as bone grafting, soft tissue grafting, prosthetic-driven implant placement, maxillofacial Prosthodontics and Temporomandibular joint disorders. CBCT images are important in special cases that require the assessment of restorability of multiple teeth.
The newest CBCT systems show higher resolution and lower exposure than previous systems, and the new systems are less expensive and more specific for dental use than their predecessors. One of the most clinically useful aspects of CBCT imaging is the availability of highly sophisticated software that allows the large volumes of acquired data to be broken down, processed and reconstructed[79]. This ability makes data interpretation much more user-friendly, particularly if competent technical and educational training is provided to the dentists and technicians.
CBCT also shows disadvantages such as susceptibility to motion artifacts, low contrast resolution, and limited internal soft-tissue visualization capability. Furthermore, due to the distortion of Hounsfield units, CBCT cannot be used for the estimation of bone density. As far as the radiation dose of CBCT imaging is concerned, it is crucial that a radiation dose As Low As Reasonably Achievable (ALARA) is respected. Although CBCT imaging will certainly improve patient care, dentists must possess the anatomical knowledge and the experience to interpret the scanned data accurately. Dentists must evaluate whether these imaging modalities add to their diagnostic knowledge and raise the standard of dental care or simply place the patient at a higher risk.
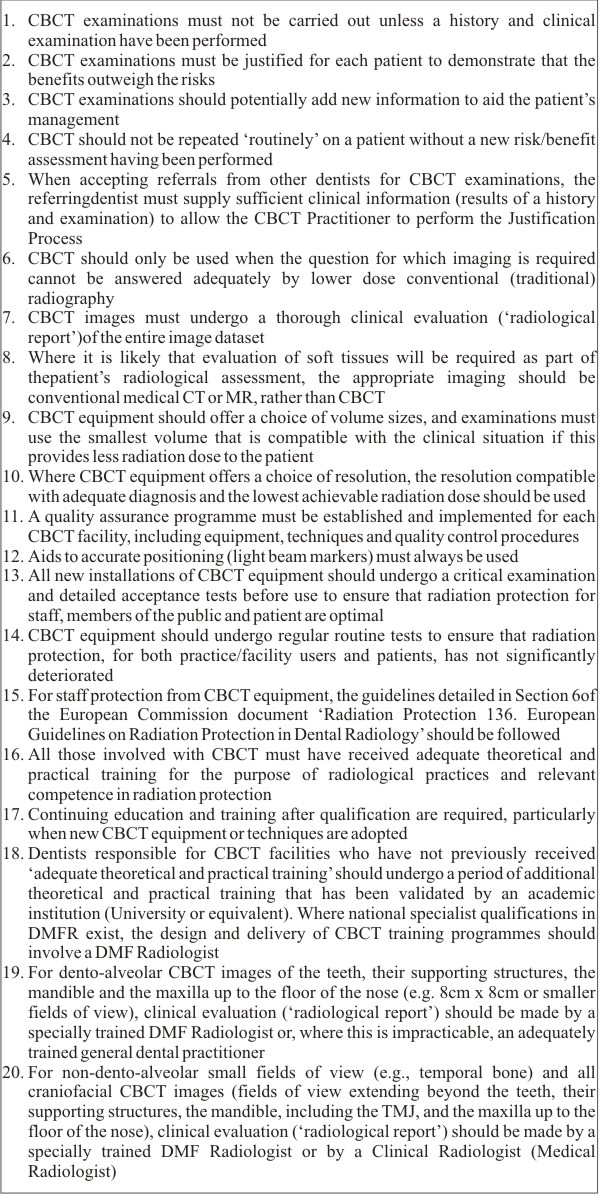 | Basic principles on the use of CBCT in dental applications:
 |
Conclusion
CBCT is a technology with potential for providing the dental profession with a new imaging alternative to conventional IOPA’s/OPG’s and with the added advantages of improved accuracy and 3-D visualisation of anatomical structures in the orofacial complex.The use of CBCT technology in clinical dental practice provides a number of advantages for maxillofacial imaging.
These include:
1) Rapid Scan Time
2) Beam Limitation
3) Image Accuracy
4) Reduced patient radiation dose compared to conventional CT
5) Interactive display modes unique to maxillofacial imaging
However discretion has to exercised on part of the prescribing dentist. To this end, the European Academy of Dento Maxillofacial Radiology has developed the following basic principles on the use of CBCT in dentistry [80]
References
1. Almog DM, LaMar J, LaMar FR, LaMar F. Cone beam computerized tomographybased dental imaging for implant planning and surgical guidance, Part 1: Single implant in the mandibular molar region. J Oral Implantol. 2006;32(2):77-81.
2. Aranyarachkul P, Caruso J, Gantes B, Schulz E, Riggs M, Dus I, Yamada JM, Crigger M. Bone density assessments of dental implant sites: 2. Quantitative cone beam Computerized tomography . Int J Oral Maxillofac Implants. 2005 May-Jun;20(3):416-24.
3. Bassam H. Reliability of Periapical Radiographs and Orthopantomograms in Detection of Tooth Root Protrusion in the Maxillary Sinus: Correlation Results with Cone Beam Computed Tomography. J Oral Maxillofac Res 2010 (Jan-Mar);1(1):e6.
4. Bianchi A, Muyldermans L, Di Martino M, Lancellotti L, Amadori S, Sarti A, Marchetti C. Facial soft tissue esthetic predictions: validation in craniomaxillofacial surgery with cone beam computed tomography data. J Oral Maxillofac Surg. 2010 Jul;68(7):1471-9.
5. Blessmann M, Pohlenz P, Blake FA, Lenard M, Schmelzle R, Heiland M. Validation of a new training tool for ultrasound as a diagnostic modality in suspected midfacial fractures. Int J Oral Maxillofac Surg. 2007 Jun;36(6):501-6.
6. Cevidanes LH, Bailey LJ, Tucker SF, Styner MA, Mol A, Phillips CL, Proffit WR, Turvey T. Three-dimensional cone-beam computed tomography for assessment of mandibular changes after orthognathic surgery. Am J Orthod Dentofacial Orthop. 2007 Jan;131(1):44-50.
7. Cha JY, Mah J, Sinclair P. Incidental findings in the maxillofacial area with 3-dimensional cone-beam imaging. Am J Orthod Dentofacial Orthop. 2007 Jul;132(1):7-14.
8. Chiandussi S, Biasotto M, Dore F, Cavalli F, Cova MA, Di Lenarda R. Clinical and diagnostic imaging of bisphosphonate-associated osteonecrosis of the jaws. Dentomaxillofac Radiol. 2006 Jul;35(4):236-43.
9. Closmann JJ, Schmidt BL. The use of cone beam computed tomography as an aid in evaluating and treatment planning for mandibular cancer. J Oral Maxillofac Surg. 2007 Apr;65(4):766-71.
10. Cohenca N, Simon JH, Mathur A, Malfaz JM. Clinical indications for digital imaging in dento-alveolar trauma. Part 2: root resorption. Dent Traumatol. 2007 Apr;23(2):105-13.
11. Cohenca N, Simon JH, Roges R, Morag Y, Malfaz JM. Clinical indications for digital imaging in dento-alveolar trauma. Part 1: traumatic injuries. Dent Traumatol. 2007 Apr;23(2):95-104.
12. Cotton TP, Geisler TM, Holden DT, Schwartz SA, Schindler WG. Endodontic applications of cone-beam volumetric tomography. J Endod. 2007 Sep;33(9):1121-32. Epub 2007 Jul 19.
13. Danforth RA, Peck J, Hall P. Cone beam volume tomography: an imaging option for diagnosis of complex mandibular third molar anatomical relationships. J Calif Dent Assoc. 2003 Nov;31(11):847-52.
14. de Paula-Silva FW, Santamaria M Jr, Leonardo MR, Consolaro A, da Silva LA. Cone-beam computerized tomographic, radiographic, and histologic evaluation of periapical repair in dogs' post-endodontic treatment. Oral Surg Oral Med Oral Pathol Oral Radiol Endod. 2009 Nov;108(5):796-805.
15. de Paula-Silva FW, Wu MK, Leonardo MR, da Silva LA, Wesselink PR. Accuracy of periapical radiography and cone-beam computed tomography scans in diagnosing apical periodontitis using histopathological findings as a gold standard. J Endod. 2009 Jul;35(7):1009-12.
16. Dreiseidler T, Mischkowski RA, Neugebauer J, Ritter L, Zöller JE. Comparison of cone-beam imaging with orthopantomography and computerized tomography for assessment in presurgical implant dentistry. Int J Oral Maxillofac Implants. 2009 Mar-Apr;24(2):216-25.
17. Estrela C, Bueno MR, Azevedo BC, Azevedo JR, Pécora JD. A new periapical index based on cone beam computed tomography. J Endod. 2008 Nov;34(11):1325-31.
18. Estrela C, Bueno MR, De Alencar AH, Mattar R, Valladares Neto J, Azevedo BC, De Araújo Estrela CR. Method to evaluate inflammatory root resorption by using cone beam computed tomography. J Endod. 2009 Nov;35(11):1491-7.
19. Ogawa T, Enciso R, Shintaku WH, Clark GT. Evaluation of cross-section airway configuration of obstructive sleep apnea. Oral Surg Oral Med Oral Pathol Oral Radiol Endod. 2007 Jan;103(1):102-8.
20. Fortin T. Champleboux G.Bianchi S.Buatois H.Coudert J-L. Precision of transfer of preoperative planning fororal implants based on cone-beam CT-scan images through a robotic drilling machine - An in vitro study. Clinical Oral Implants Research Vol. 13 No. 6 pp 651-656.
21. Heiland M, Schulze D, Rother U, Schmelzle R. Postoperative imaging of zygomaticomaxillary complex fractures using digital volume tomography. J Oral Maxillofac Surg. 2004 Nov;62(11):1387-91.
22. Zizelmann C, Gellrich NC, Metzger MC, Schoen R, Schmelzeisen R, Schramm A. Computer-assisted reconstruction of orbital floor based on cone beam tomography. Br J Oral Maxillofac Surg. 2007 Jan;45(1):79-80.
23. Heiland M, Schulze D, Blake F, Schmelzle R. Intraoperative imaging of zygomaticomaxillary complex fractures using a 3D C-arm system. Int J Oral Maxillofac Surg. 2005 Jun;34(4):369-75.
24. Swennen GR, Mollemans W, De Clercq C, Abeloos J, Lamoral P, Lippens F, Neyt N, Casselman J, Schutyser F. A cone-beam computed tomography triple scan procedure to obtain a three-dimensional augmented virtual skull model appropriate for orthognathic surgery planning. J Craniofac Surg. 2009 Mar;20(2):297-307.
25. Swennen GR, Mommaerts MY, Abeloos J, De Clercq C, Lamoral P, Neyt N, Casselman J, Schutyser F. A cone-beam CT based technique to augment the 3D virtual skull model with a detailed dental surface. Int J Oral Maxillofac Surg. 2009 Jan;38(1):48-57.
26. Wörtche R, Hassfeld S, Lux CJ, Müssig E, Hensley FW, Krempien R, Hofele C. Clinical application of cone beam digital volume tomography in children with cleft lip and palate. Dentomaxillofac Radiol. 2006 Mar;35(2):88-94.
27. Smith MH, Brooks SL, Eldevik OP, Helman JI. Anterior mandibular lingual salivary gland defect: a report of a case diagnosed with cone-beam computed tomography and magnetic resonance imaging. Oral Surg Oral Med Oral Pathol Oral Radiol Endod. 2007 May;103(5):e71-8
28. Honda M, Uehara H, Uehara T, Honda K, Kawashima S, Honda K, Yonehara Y. Use of a replica graft tooth for evaluation before autotransplantation of a tooth. A CAD/CAM model produced using dental-cone-beam computed tomography. Int J Oral Maxillofac Surg. 2010 Jul 12.
29. Estrela C, Bueno MR, Leles CR, Azevedo B, Azevedo JR. Accuracy of cone beam computed tomography and panoramic and periapical radiography for detection of apical periodontitis. J Endod. 2008 Mar;34(3):273-9.
30. Lofthag-Hansen S, Huumonen S, Gröndahl K, Gröndahl HG. Limited conebeam CT and intraoral radiography for the diagnosis of periapical pathology. Oral Surg Oral Med Oral Pathol Oral Radiol Endod. 2007 Jan;103(1):114-9.
31. Nakata K, Naitoh M, Izumi M, Inamoto K, Ariji E, Nakamura H. Effectiveness of dental computed tomography in diagnostic imaging of periradicular lesion of each root of a multirooted tooth: a case report. J Endod. 2006 Jun;32(6):583-7.
32. Patel S. New dimensions in endodontic imaging: Part 2. Cone beam computed tomography. Int Endod J. 2009 Jun;42(6):463-75.
33. Tyndall DA, Rathore S. Cone-beam CT diagnostic applications: caries, periodontal bone assessment, and endodontic applications. Dent Clin North Am. 2008 Oct;52(4):825-41.
34. Simon JH, Enciso R, Malfaz JM, Roges R, Bailey-Perry M, Patel A Differential diagnosis of large periapical lesions using cone-beam computed tomography measurements and biopsy. J Endod. 2006 Sep;32(9):833-7.
35. Nair MK, Nair UP. Digital and advanced imaging in endodontics: a review. J Endod. 2007 Jan;33(1):1-6.
36. Ozer SY. Detection of vertical root fractures of different thicknesses in endodontically enlarged teeth by cone beam computed tomography versus digital radiography. J Endod. 2010 Jul;36(7):1245-9.
37. Hassan B, Metska ME, Ozok AR, van der Stelt P, Wesselink PR. Comparison of five cone beam computed tomography systems for the detection of vertical root fractures. J Endod. 2010 Jan;36(1):126-9.
38. Hassan B, Metska ME, Ozok AR, van der Stelt P, Wesselink PR. Detection of vertical root fractures in endodontically treated teeth by a cone beam computed tomography scan. J Endod. 2009 May;35(5):719-22.
39. Patel S, Dawood A. The use of cone beam computed tomography in the management of external cervical resorption lesions. Int Endod J. 2007 Sep;40(9):730-7.
40. Michetti J, Maret D, Mallet JP, Diemer F. Validation of cone beam computed tomography as a tool to explore root canal anatomy. J Endod. 2010 Jul;36(7):1187-90.
41. Garcia de Paula-Silva FW, Hassan B, Bezerra da Silva LA, Leonardo MR, Wu MK. Outcome of root canal treatment in dogs determined by periapical radiography and cone-beam computed tomography scans. J Endod. 2009 May;35(5):723-6.
42. Tsurumachi T, Honda K. A new cone beam computerized tomography system for use in endodontic surgery. Int Endod J. 2007 Mar;40(3):224-32.
43. Moore J, Fitz-Walter P, Parashos P. A micro-computed tomographic evaluation of apical root canal preparation using three instrumentation techniques. Int Endod J. 2009 Dec;42(12):1057-64.
44. Nagaraja S, Sreenivasa Murthy BV. CT evaluation of canal preparation using rotary and hand NI-TI instruments: An in vitro study. J Conserv Dent. 2010 Jan;13(1):16-22.
45. Hatcher DC, Dial C, Mayorga C. Cone beam CT for pre-surgical assessment of implant sites. J Calif Dent Assoc. 2003 Nov;31(11):825-33.
46. Howerton WB Jr, Mora MA. Advancements in digital imaging: what is new and on the horizon? J Am Dent Assoc. 2008 Jun;139 Suppl:20S-24S.
47. Hua Y, Nackaerts O, Duyck J, Maes F, Jacobs R. Bone quality assessment based on cone beam computed tomography imaging. Clin Oral Implants Res. 2009 Aug;20(8):767-71
48. Lofthag-Hansen S, Gröndahl K, Ekestubbe A. Cone-beam CT for preoperative implant planning in the posterior mandible: visibility of anatomic landmarks. Clin Implant Dent Relat Res. 2009 Sep;11(3):246-55.
49. Macleod I, Heath N. Cone-beam computed tomography (CBCT) in dental practice. Dent Update. 2008 Nov;35(9):590-2, 594-8.
50. Palomo JM, Kau CH, Palomo LB, Hans MG. Three-dimensional cone beam computerized tomography in dentistry. Dent Today. 2006 Nov;25(11):130, 132-5.
51. Scott D. Ganz, CT Scan Technology An Evolving Tool for Avoiding Complications and Achieving Predictable Implant Placement and Restoration. INTERNATIONAL MAGAZINE OF ORAL IMPLANTOLOGY 1/2001.
52. Sforza NM, Franchini F, Lamma A, Botticelli S, Ghigi G. Accuracy of computerized tomography for the evaluation of mandibular sites prior to implant placement. Int J Periodontics Restorative Dent. 2007 Dec;27(6):589-95.
53. Van Assche N, van Steenberghe D, Guerrero ME, Hirsch E, Schutyser F, Quirynen M, Jacobs R. Accuracy of implant placement based on pre-surgical planning of three-dimensional cone-beam images: a pilot study. J Clin Periodontol. 2007 Sep;34(9):816-21.
54. Nickenig HJ, Eitner S. Reliability of implant placement after virtual planning of implant positions using cone beam CT data and surgical (guide) templates. J Craniomaxillofac Surg. 2007 Jun-Jul;35(4-5):207-11.
55. Sato S, Arai Y, Shinoda K, Ito K. Clinical application of a new cone-beam computerized tomography system to assess multiple two-dimensional images for the preoperative treatment planning of maxillary implants: case reports Quintessence Int. 2004 Jul-Aug;35(7):525-8.
56. Heiland M, Pohlenz P, Blessmann M, Werle H, Fraederich M, Schmelzle R, Blake FA. Navigated implantation after microsurgical bone transfer using intraoperatively acquired cone-beam computed tomography data sets. Int J Oral Maxillofac Surg. 2008 Jan;37(1):70-5.
57. Smith TB. Cone-beam volumetric imaging in dental, oral, and maxillofacial medicine: fundamentals, diagnostics, and treatment planning. J Prosthodont. 2010 Jul;19(5):419.
58. Song Y., Jun S., Kwon J. Correlation between bone quality evaluation by conebeam computerized tomography and implant primary stability. Int. Journal of Oral and Maxillofacial Implants Vol. 24 No. 1 pp 59-64.
59. King KS, Lam EW, Faulkner MG, Heo G, Major PW. Predictive factors of verti cal bone depth in the paramedian palate of adolescents. Angle Orthod. 2006 Sep;76(5):745-51.
60. Shi H, Scarfe WC, Farman AG. Three-dimensional reconstruction of individual cervical vertebrae from cone-beam computed-tomography images. Am J Orthod Dentofacial Orthop. 2007 Mar;131(3):426-32.
61. Müssig E, Wörtche R, Lux CJ. Indications for digital volume tomography in orthodontics. J Orofac Orthop. 2005 May;66(3):241-9.
62. Peck JL, Sameshima GT, Miller A, Worth P, Hatcher DC. Mesiodistal root angulation using panoramic and cone beam CT. Angle Orthod. 2007 Mar;77(2):206-13.
63. SH, Choi YS, Hwang EH, Chung KR, Kook YA, Nelson G. Surgical positioning of orthodontic mini-implants with guides fabricated on models replicated with cone-beam computed tomography. Am J Orthod Dentofacial Orthop. 2007 Apr;131(4 Suppl):S82-9.
64. Poggio PM, Incorvati C, Velo S, Carano A. "Safe zones": a guide for miniscrew positioning in the maxillary and mandibular arch. Angle Orthod. 2006 Mar;76(2):191-7.
65. Tantanapornkul W, Okouchi K, Fujiwara Y, Yamashiro M, Maruoka Y, Ohbayashi N, Kurabayashi T. A comparative study of cone-beam computed tomography and conventional panoramic radiography in assessing the topographic relationship between the mandibular canal and impacted third molars. Oral Surg Oral Med Oral Pathol Oral Radiol Endod. 2007 Feb;103(2):253-9.
66. Tsiklakis K, Syriopoulos K, Stamatakis HC. Radiographic examination of the temporomandibular joint using cone beam computed tomography. Dentomaxillofac Radiol. 2004 May;33(3):196-201.
67. Kijima N, Honda K, Kuroki Y, Sakabe J, Ejima K, Nakajima I. Relationship between patient characteristics, mandibular head morphology and thickness of the roof of the glenoid fossa in symptomatic temporomandibular joints. Dentomaxillofac Radiol. 2007 Jul;36(5):277-81.
68. Honda K, Matumoto K, Kashima M, Takano Y, Kawashima S, Arai Y. Single air contrast arthrography for temporomandibular joint disorder using limited cone beam computed tomography for dental use. Dentomaxillofac Radiol. 2004 Jul;33(4):271-3.
69. Honda K, Larheim TA, Johannessen S, Arai Y, Shinoda K, Westesson PL. Ortho cubic super-high resolution computed tomography: a new radiographic technique with application to the temporomandibular joint. Oral Surg Oral Med Oral Pathol Oral Radiol Endod. 2001 Feb;91(2):239-43.
70. Honda K, Bjørnland T. Image-guided puncture technique for the superior temporomandibular joint space: value of cone beam computed tomography (CBCT). Oral Surg Oral Med Oral Pathol Oral Radiol Endod. 2006 Sep;102(3):281-6.
71. Misch KA, Yi ES, Sarment DP. Accuracy of cone beam computed tomography for periodontal defect measurements. J Periodontol. 2006 Jul;77(7):1261-6.
72. Vandenberghe B, Jacobs R, Yang J. Diagnostic validity (or acuity) of 2D CCD versus 3D CBCT-images for assessing periodontal breakdown. Oral Surg Oral Med Oral Pathol Oral Radiol Endod. 2007 Sep;104(3):395-401.
73. Compact computed tomography system for evaluating the outcome of regenerative therapy: a case report. J Periodontol. 2001 May;72(5):696-702.
74. Naitoh M, Yamada S, Noguchi T, Ariji E, Nagao J, Mori K, Kitasaka T, Suenaga Y. Three-dimensional display with quantitative analysis in alveolar bone resorption using cone-beam computerized tomography for dental use: a preliminary study. Int J Periodontics Restorative Dent. 2006 Dec;26(6):607-12.
75. Tetradis S, Anstey P, Graff-Radford S. Cone beam computed tomography in the diagnosis of dental disease. J Calif Dent Assoc. 2010 Jan;38(1):27-32.
76. Yang F, Jacobs R, Willems G. Dental age estimation through volume matching of teeth imaged by cone-beam CT. Forensic Sci Int. 2006 May 15;159 Suppl 1:S78-83.
77. Arai Y, Tammisalo E, Iwai K, Hashimoto K, Shinoda K. Development of a compact computed tomographic apparatus for dental use. DentomaxillofacRadiol 1999: 28: 245–248.
78. W. De Vos, J. Casselman, G.R.J. Cone-beam computerized tomography (CBCT) imaging of the oral and maxillofacial region: A systematic review of the literature. Int. J. Oral Maxillofac. Surg. 2009; 38: 609–625
79. Patel S, Dawood A, Ford TP, Whaites E. The potential applications of cone beam computed tomography in the management of endodontic problems. Int Endod J 2007: 40: 818–830.
80. Horner K, Islam M, Flygare L, Tsiklakis T, Whaites E. Basic Principles for Use of Dental Cone Beam CT: Consensus Guidelines of the European Academy of Dental and Maxillofacial Radiology. Dentomaxillofac Radiol 2009; 38: 187-195.
|