Introduction
Giant cell tumour (GCT) even when benign, is a locally aggressive neoplasm which comprises 4% to 9.5% of all primary osseous neoplasia.[1] It usually occurs in the third to fourth decade and shows a slight female preponderance.[2] The most common sites of involvement are the ends of long bones, but cranial involvement is unusual. In the skull, sphenoid bone is the most common site followed by temporal bone in rare cases.[3] However, GCT of the jaw bone is extremely rare.[4] The present case report is one such exceptional occurrence.
Case Report
A 22year old male patient presented with a swelling of one month’s duration in the right parotid region with a clinical diagnosis of pleomorphic adenoma of salivary gland. On examination, a soft to firm, well-defined mass measuring 3x2cm was palpable in the right parotid region. FNAC of the lesion yielded a highly cellular smear composed of dual population of mononuclear cells which showed mild pleomorphism , oval bland nuclei , occasional mitoses and many multinucleated osteoclastic giant cells which were seen along the periphery of the cell clusters (Figure 1). A cytologic diagnosis of benign giant cell tumour was offered and a radiological opinion was sought to rule out involvement of the mandible. Serum calcium and phosphorus levels were within normal limits. X-ray confirmed an osteolytic lesion of the ramus of the mandible (Figure 2). Per-operatively, the lesion in the ramus of mandible was seen to erode the cortex, but the temporo-mandibular joint and the parotid gland were spared. Histopathologic examination of the curettage material showed a tumour composed of mononuclear oval to round cells with moderate amount of cytoplasm and oval, bland nuclei. Multinucleated osteoclastic giant cells were uniformly distributed amidst the tumour cells (Figures 3 & 4). Occasional mitoses were seen in the mononuclear cell population. A correlative final diagnosis based on clinical, cytological, radiological, per-operative and histopathological findings of “Benign GCT arising from mandible” was formulated.
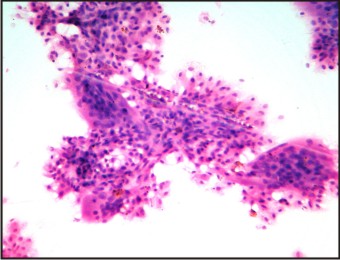 | Figure 1: Cytology smear composed of sheets of benign round to oval stromal cells and multinucleate giant cells around its periphery (X400)
 |
 | Figure 2: X-ray showing an osteolytic lesion in the ramus of mandible
 |
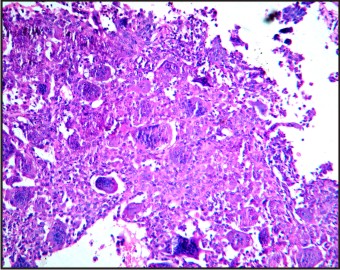 | Figure 3: Tumor composed of mononuclear cells and uniformly distributed multinucleated giant cells (X100)
 |
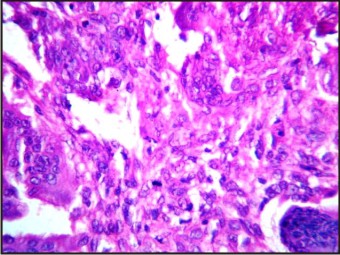 | Figure 4: Round to oval mononuclear cells showing occasional mitosis, giant cells and stromal cells with similar nuclear features (X400)
 |
Discussion
GCT comprises 5% of all biopsied primary bone tumours. About 80% of the patients are in age group of 20-50years.[5] There is a mild female preponderance, which is more pronounced in the younger age group.[6] It chiefly occurs at the ends of long bones, especially in bones around the knee. Involvement of the skull is rare and of the mandible in particular is exceptional.[4] The present case of GCT of the ramus of mandible in a 22year old male is one such.These lesions are seen as osteolytic lesions on radiology as in the present case. Microscopically, GCT consists of plump, spindle shaped or ovoid cells admixed with multinucleated, cytologically benign giant cells. The nuclei are generally hypochromic with inconspicuous nucleoli. Mitotic figures are uncommon.[7] All these features were observed in the present case.
The differential diagnoses considered were, Giant cell reparative granuloma (GCRG), Cherubism Aneurysmal bone cyst and Hyperparathyroidism
GCRGs and GCTs are very similar histologically and the main significant difference is in the larger number of nuclei in the giant cells of GCT.[8], [9] In addition, the stroma in GCRG is relatively acellular and shows osseous metaplasia. The nuclei of giant cells and stromal cells are similar in GCT, whereas they are different in GCRG.[10] The feature which upheld the diagnosis of GCT in the present case was the similarity between the nuclei of the giant cells and the stromal cells.
Cherubism was ruled out considering the absence of bilateral involvement of mandible and also considering that it normally occurs in children between 2 and 4 years of age.
Aneurysmal bone cyst is typically composed of thin-walled, blood-filled spaces which are lined by flattened cells with a row of osteoclasts underneath along with degenerated calcifying fibromyxoid tissue. None of these features were appreciated in the present case.
Hyperparathyroidism was ruled out keeping in view the normal serum calcium and phosphorus levels.
Surgery is the most accepted form of treatment for GCTs which includes simple excision and curettage as was done in the present case. Some clinicians prefer partial jaw resection to ensure avoidance of recurrence. Prosser et.al recommend primary curettage of intra-osseous GCT without adjuvant treatment and more aggressive treatment for tumors with soft tissue extension or with local recurrence.[11]
In conclusion, diagnosis of GCT in unusual locations like skull bones, especially when exceptional sites like mandible are involved may pose unexpected diagnostic dilemmas as in this case which may necessitate a multi-disciplinary approach to ensure appropriate patient management.
References
1. Faisham WI, Zulmi W, Halim AS, Biswas BM, Mutum SS, et al. Aggressive giant cell tumor of bone. Singapore Med J 2006;47:679-683.
2. Christopher D. M. Fletcher. Diagnostic Histopathology of Tumors vol.2, 2nd edn., Elsevier Publication, 2000:1574-1576.
3. Motomochi M, Handa Y, Makita Y, Hashi K. Giant cell tumor of the skull. Surg Neurol 1985;23(1):25-30.
4. Juan Rosai. Rosai and Ackerman’s Surgical Pathology vol.1, 9th edn, Elsevier Publication, 2009:295.
5. Joseph M. Mirra. Bone tumors- Clinical, Radiologic and Pathologic correlations vol.2, Lea and Febiger Ltd.,1989:941-1020.
6. Henderson BTH, Whitwell H. Giant cell tumor of the skull: case report. Neurosurg 1988;23(1):120-122.
7. Wolfe JT, Sheithawer BW, Dahlin DC. Giant cell tumor of the sphenoid bone. J Neurosurg 1983;59:322-327.
8. Auclair PL, Cuenin P, Kratochvil FJ, Slater LJ, Ellis GL. A clinical and histomorphologic comparison of the central giant cell granuloma and the giant cell tumor. Oral Surg Oral Med Oral Pathol 1988;66(2):197-208.
9. Franklin CD, Craig GT, Smith CJ. Quantitative analysis of histologic parameters in giant cell lesions of the jaws and long bones. Histopathology 1979;3(6):511-522.
10. Kiwit JC, Schober R, Nicola N, 9Schirmer M, Wechsler W. Osteoclastomas of the petrous bone. Surg Neurol 1986;26(1):59-62.
11. Prosser GH, Baloch KG, Tillman RM, Carter SR, Grimer RJ. Does curettage without adjuvant therapy provide low recurrence rates in giant cell tumors of bone? Clin Orthop Relat Res 2005;435:211-218.
|