Introduction
Osteomas are benign tumours composed of mature compact or cancellous bone. These are essentially restricted to the craniofacial skeleton and very rarely if ever, are diagnosed in other bones.[1],[6]. These still are under question whether these are a true neoplasm or lesions representing end stage of an injury or inflammatory process or the end stage of a hamartomatous process, such as fibrous dysplasia.[3]. Osteomas are completely benign, and patients do not experience malignant change. Recurrence after excision is extremely rare.[1],[2],[4].
Case Report
An eighteen year old female nursing student reported to us with the chief complaint of dull pain in the right side of lower jaw from past 4 - 5 months. There was no other symptom and patient never underwent any dental treatment before this. Patient gave no history of any kind of paraesthesia. On inspection mild facial deformity was observed. On palpation mild tenderness was present at right angle of the mandible which was not associated with any discharge, fluctuancy or bleeding.
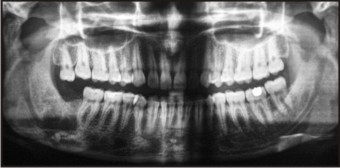
Intraoral periapical radiograph was taken for the clinically missing 48. Radiopaque lesion was incompletely seen distal to 47 which was clinically and radiographically normal (Fig 1).
 | Fig 1. Pre Operative Diagnostic Panoramic View.
 |
Panoramic view showed a large, irregular, cloud shaped, radiopaque mass at right angle of the mandible which was associated with an impacted third molar lying inferior to the radiopaque mass almost at the inferior border of mandible just sparing about 1 mm of bone (Fig.1).
Based on this a provisional diagnosis of odontome, cacifying fibroosseous lesion or an osteoma was made.
As medical history was not significant excisional biopsy was done under local anaesthesia after routine haematological tests and strict sterile conditions. Preanaesthetic medication was prescribed for mild sedation so that the patient was comfortable during the surgery. The complete mass was excised by sectioning along with the extraction of the third molar (Fig 2.). There was a doubt whether complete removal of tooth was achieved or not as the risk of exploring into the extreme lower border of mandible inducing pathological fracture was not worth taking. The complete excised specimen was sent for histopathological examination along with the tooth. Hemostasis was achieved and wound was closed for secondary healing method.
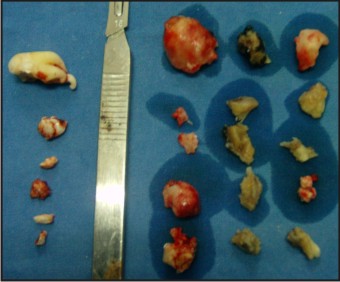 | Fig 2. Excised Specimen With Tooth Segments On Left And Excised Lesion On Right Side.
 |
Initially the patinet was called every third day for regular irrigations and wound care and patient gave good co-operation and followed all instructions. Post operative panoramic view showed complete excision of the lesion and the tooth. Histopathological diagnosis was given as osteoma.
Patient gave a good follow up after surgery upto one year and undertook all routine dental treatment as deemed necessary and is still under follow up.(Fig 3).
 | Fig 3. One Year Follow Up Panoramic View.
 |
Discussion
Osteomas are benign osteogenic lesions characterized by proliferation of either cancellous or compact bone and can be central, peripheral or extraskeletal. These may arise in medullary bone[2],[9],[4]. Clinically peripheral osteoma is usually asymptomatic and can be found during a routine radiographic examination.[2],[7]. Osteomas usually have a slow growth rate, but it can produce swelling and can cause asymmetry. The radiographic appearance is well circumscribed radiopaque lesion.[2],[5]. Patients with multiple osteomas should be evaluated for Gardner’s Syndrome. The triad of colorectal polyposis, skeletal abnormalities, and multiple impacted supernumerary teeth is consistent with this syndrome.[2],[10],[5].
So complete assessment of the patient for other systemic symptoms should be done. When assymetry is present surgical removal of the lesion is mandatory as these lesions rarely recur once completely removed.[2],[6],[8].
In this case lesion was surgically excised as it was symptomatic along with the removal of the associated deeply impacted tooth. Osteomas rarely recur when treated surgically.[2],[6].
References
1. Neville, Damm, Allen, Bouquot Oral and Maxillofacial PathologyThird ed. 650-655
2. Terra E.R ,Ramos F.M, Gomes P.P, Passeri L.A, Boscolo F.N. Peripheral osteoma of the mandible: Clinical Case, Braz J Oral Sci April/june 2005,vol 4, No.13.
3. Chaudhry M., Kulkarni M. Osteoid osteoma of mandible. J. of Oral and Maxillofacial pathology Dec 2007, 11, 2.
4. Ramesh V, Lakshmi S, Osteoma of mandible – a case report. Annals and Essences of Dentistry 2011,3,3 78-80.
5. Pieterse A.S, Roberts B., Paterson D., Cornish B., Lewis P. Osteoid osteoma transforming to aggressive ( low grade malignant) osteoblastoma: a case reportand literature review. J. of British Division of the International Academy of Pathology – histopathology 1983,7,5, 789-800.
6. Kerchhaet A., Wolvius E., Vanderwall K., Oosterhuis J. A giant osteoma of the mandible: case report.J of Cranio- maxillofacial Surgery, Aug 2005, 33,4, 282.
7. Johann A.,Freitas J.,Aguiar M.,Araujo N., Mesquita R., Peripheral osteoma of the mandible case report and review of the literature, J. of Cranio-maxillofacial surgery, Aug 2005,33,4,276-281.
8. Swanson A., GuttuR.,Giganticosteoma of mandible – Report of a case, J of Oral and maxillofacial surgery ,June 1992, 50, 6, 635- 638.
9. CutilliB.,Quinn P., Traumatically induced peripheral osteoma –Report of a case, Oral surgery, Oral Medicine, Oral Pathology, June 1992, 73,6,667-669.
10. Ogbureke K.,Nashed M., Ayoub A., Huge peripheral osteoma of mandible – A case report and review of literature, Pathology – Research and Practice, March 2007,203,3, 185 – 188.
|