Case Report:
A 60 year old male patient came to the department with the chief complaint of swelling in the left upper back tooth region since 6 months associated with pain in the same region since 2years.
Patient’s history of present illness revealed that he was assymptomatic 2years back, till he developed pain in the left upper back tooth region. Pain is sudden in onset, pricking, intermittent, moderate in intensity and radiating all along the left half of the face. He noticed swelling adjacent to the left upper back tooth region causing pain and inconvenience while chewing food due to mobility of teeth. Then he visited local dentist where he underwent extraction of the complaining teeth (26, 27). After extraction patient gave the history of moist heat fomentation and smoking bidi on the next day. After that he noticed an increase in the size of swelling on the left side. Patient also gives h/o loss of appetite, weight loss and fever from the past 6 months.
There was no significant past medical history. Patient gives the history extraction of 26, 27 six months back.
Family historywas non contributory.
Patient’s Personal History revealed that he was married and blessed with two children. He used to clean his teeth once daily with finger and native powder. Patient was the beedi smoker since 40 years, 5-6 beedis/day.
On General Physical Examination patient was found to be well built, not anemic, not cyanosed, no signs of organomegaly. Patient’s pulse rate was 70/minute, respiratory rate 18/minute and blood pressure 140/90mm of Hg.
On Extra oral examination, leftl submandibular lymph nodes were found to be enlarged and palpable.
Size: 3×3cms on the left side.
Tender and firm in consistency.
A solitary swelling was present over the left lower third of the face measuring about 4×3cms in size, oval in shape with well defined borders. It was extending anteroposteriorly from 4cms posterior to the chin region upto 1 cm anterior to angle of mandible and superoinferiorly from inferior border of the mandible to 2cms below the inferior border. (Figure 1) On palpation there was no local rise on the temperature, swelling was firm in consistency, non tender, and non compressible.
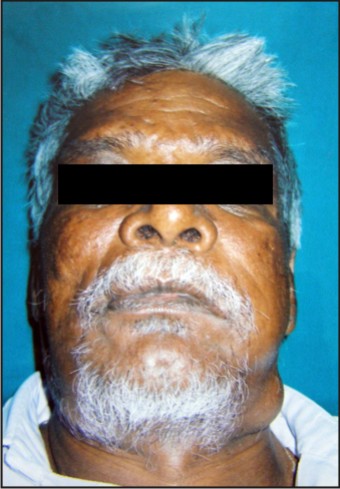 | Fig 1. : Extraoral photograph representing swelling over the left lower third of the face.
 |
Intra oral Examinationrevealed normal mouth opening i.e. 42mms. There was generalized gingival inflammation and recession. There was generalized bleeding on probing. Intraorally also two swellings were present, one in the left upper back tooth region, and 2nd in the right upper back tooth region. (Figure 2).
 | Fig 2. : Intraoral photograph depicting a soft tissue swelling i.r.t. 26,27 region.
 |
Left Upper back swelling: An exophytic, sessile growth measuring about 6×6cms in size extending anteroposteriorly from the left maxillary tuberosity upto the left retrocommissural area and superoinferiorly from the alveolar ridge to 2cms below the level of occlusal plane. Surface appears smooth with grayish black pigmentation interspersed with erythematous areas.
The swelling was soft to rubbery in consistency, non-compressible, non tender, and mobile and tend to bleed on provocation.
Based on the patient’s chief complaint and clinical examination we thought of the Provisional Diagnosis of Malignancy arising from left alveolar ridge i.r.t. 26, 27.
Differential Diagnosisfor the present case can be any Salivary gland neoplasm and Melanoma
After this, patient was subjected to the:
Complete Hemogram
ESR – 45mm/hr
Blood Sugar – 80mg%
Alkaline Phosphatase – 84mg/ml
Creatinine – 0.9mg/ml
FNAC of Right and Left Submandibular lymph nodes, which revealed numerous inflammatory cells and cellular necrotic debris.
Radiographs:
OPG
PNS View
Radiographs demonstrated a localized, well defined soft tissue shadow involving the lt. maxillary tuberosity area, approx. 6x6 cms in size.
Incisional Biopsy of the exophytic growth was made under general anaesthesia.
Sections revealed proliferating tumour cells in large solid sheets. Tumour cells were mostly polygonal and occasionally appearing columnar in shape, in sheets and peripherally as strands. The infilterating cells revealed varying degrees of atypia. Many cells revealed certain degree of pleomorphism with hyperchromatic and vesicular nuclei and nucleoli appeared to be prominent. The cytoplasm of many cells appeared to be clear with granular eosinophillic cytoplasm. (Figure 3).
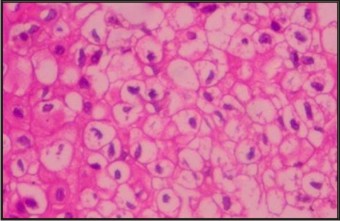 | Fig 3. : Histpathologically showing cellular atypia with hyperchromatic nulei and clear cells.
 |
Overall features suggested of Clear Cell Carcinoma.
Excision of the swelling was planned and the patient was put on injection Augmentin 1.2gms and Inj. Dexona 8mg i.v. as the prophylactic premedication.
Discussion
Clear cell carcinoma is also referred to as hydropic SCC. It was first described by Kuo[1] in 1980 as a variant of SCC with extensive hydropic change. The hydropic degeneration of neoplastic cells and the accumulation of intracellular fluid, not the accumulation of glycogen, lipid, or mucin, results in its clear cell appearance.
The clear cell odontogenic tumor, first described by HANSEN et al, in 1985, is a rare intraosseous tumor[2] characterized histologically by sheets of cells with clear cytoplasm lying in a fibrous stroma. The tumor has recently been classified as a benign but locally invasive odontogenic tumor in the current WHO odontogenic tumor classification.[3]
Odontogenic neoplasms composed entirely or predominantly of clear cells are exceptionally rare.[4] Examples include the clear cell variants of calcifying epithelial odontogenic tumor[5] and of ameloblastoma and clear cell odontogenic carcinoma.[6],[7] Consequently, terms such as clear cell odontogenic tumor and clear cell ameloblastoma seem inappropriate to identify this rare entity, and most authors now agree that these tumors should be called clear cell odontogenic carcinomas, even if showing occasional ameloblastoma-like histologic patterns.[8], [9], [10]
A search of the English literature, using clear cell and odontogenic tumor, odontogenic carcinoma, and ameloblastoma as key words, identified 27 unequivocal cases of clear cell odontogenic carcinoma. Owing to the limited numbers of such tumors reported so far, only incomplete data are available on their clinical, immunohistochemical, and prognostic features.[4]
Clear cell carcinoma occurs most commonly in elderly white men with a history of excessive sun exposure. In contrast with the case being reported where the lesion occurred in the posterior region of the maxilla, studies have shown that the anterior portions of the jaws especially the mandible are most frequently affected.[11] Clinically, it appears as a nodule or mass that may occasionally be ulcerated. Of the six cases reported, four were noted to have rapid growth.
Generally, the histologic feature is that of solid epithelial islands and nests and strands of clear and basaloid cells with scanty eosinophylic cytoplasms that are separated by septae of fibrous connective tissue. They are unencapsulated and show aggressive infiltration of the surrounding tissues.[12] Three histomorphologic patterns have been described with the commonest a biphasic tumor characterized by oval and linear nests of clear cells intermixed with smaller islands of polygonal cells with eosinophylic cytoplasm. Occationally these two cell-types co-exist in a tumor nest yielding a “glomeruloid” appearance. The second variant is represented by islands that show only the clear cell phenotype whereas the third and least common variant is comprised of clear cell nests with a tendency for ameloblastoid palisading around the periphery.[7]
It is noteworthy that ultrasound evaluations of the liver, kidneys and spleen did not reveal any metastatic lesions because tumors with clear cell component in the head and neck region could originate from odontogenic epithelium and salivary glands or even as metastasis from distant locations like the kidneys. Even additional special staining for mucin is recommended to rule out mucoepidermoid carcinoma. Furthermore, CCOC can be distinguished from the clear cell variant of calcifying epithelial odontogenic tumor because it lacks the characteristic calcification and amyloid deposition.
There are no definite universal treatment protocols for CCOC in the literature probably due to the recurrences and/or metastasis that have been recorded following aggressive surgery. Hence, CCOC should be regarded as a low-grade malignancy with capacity for sinister biologic behavior. Treatment should be by wide surgical resection with at least 1cm of tumor-free margins. In addition, elective neck dissection and adjuvant radiotherapy is suggested.
Gardner[13] addressed the question of the possible relationships between an ameloblastoma that exhibits clear cells and a CCOC. They may be part of a histopathologic spectrum and not separate entities, but this matter remains unresolved. We find little evidence to support such a contention and recommend that these lesions be regarded as distinct entities.[4]
A recent review of literature of the 43 cases reported so far[14] showed that the male: female ratio was 3:1, mean age at presentation was 58 years (range 17–89 years), the average period of follow-up was 5.5 years (range 0.5–21 years), mandible was the most favored location (84%). The overall recurrence rate for these tumors was 55% and local recurrence rates were higher (80%) for curettage alone than for resection alone (43%).
References
1. Kuo T. Clear cell carcinoma of the skin: a variant of the squamous cell carcinoma that stimulates sebaceous carcinoma.Am J Surg Pathol. 1980; 4: 573-583.
2. Hansen LS, Eversole LR, Grien TL, Powell NB. Clear cell odontogenic tumor - a new histological variant with aggressive potential. Head Neck Surg 1985: 8: 115-23.
3. Kramer IRH,Pindborg JJ, Shear M. World Health Organization international histological classification of tumours, Histological typing of odontogenic tumours, 2nd edn, Berlin: Springer-Verlag, 1992: 16.
4. Maiorano E, Altini M, Favia G. Clear cell tumours of the salivary glands, jaws and oral mucosa. Semin Diagn Pathol. 1997;14:203-212.
5. Schmidt-Westhausen A, Philipsen HP, Reichart PA. Clear cell calcifying epithelial odontogenic tumour: a case report.Int J Oral Maxillofac Surg. 1992;21:47-49.
6. Odukoya O, Arole O. Clear cell ameloblastoma of the mandible (a case report). Int J Oral Maxillofac Surg. 1992; 21:358-359.
7. Eversole LR, Duffey DC, Powell NB. Clear cell odontogenic carcinoma: a clinicopathologic analysis. Arch Otolaryngol Head Neck Surg. 1995;121:685-689.
8. Miyauchi M, Ogawa I, Takata T, et al. Clear cell odontogenic tumour: a case with induction of dentin-like structures? J Oral Pathol Med. 1998;27:220-224.
9. de Aguiar MCF, Gomez RS, Silva EC, et al. Clear cell ameloblastoma (clear cell odontogenic carcinoma): report of a case. Oral Surg Oral Med Oral Pathol Oral Radiol Endod.1996;81:79-83.
10. Eversole LR. Malignant epithelial odontogenic tumours.Semin Diagn Pathol. 1999;16:317-324.
11. Braunshtein E, Vered M, Taicher S, Buchner A. Clear cell odontogenic carcinoma and clear cell ameloblastoma: a single clinicopathologic entity? A new case and comparative analysis of the literature. J Oral Maxillofac Surg 2003; 61(9): 1004-1010.
12. Li TJ, Yu SF, Gao Y, Wang EB. Clear cell odontogenic carcinoma: a clinicopathologic and immunocytochemical study of 5 cases. Arch Pathol Lab Med 2001; 125(12): 1566-1571.
13. Gardner DG. Some current concepts on the pathology of ameloblastomas. Oral Surg Oral Med Oral Pathol Oral Radiol Endod. 1996;82:660-669.
14. Ebert CS, Dubin MG, Hart CF, Chalian AA, Shockley WW. Clear cell odontogenic carcinoma: a comprehensive analysis of treatment strategies. Head Neck. 2005;27:536–542. doi: 10.1002/hed.20181.
|