Introduction
Myoepithelioma is a rare benign tumor of salivary glands and represents 1-1.5% of all salivary gland neoplasms[1]. Myoepithelioma once considered a variant of Pleomorphic adenoma is now considered as a distinct pathological entity[2]. It is composed of various proportions of plasmacytoid, spindle, epitheloid, and clear cells that exhibit myoepithelial differentiation and generally lack ductal differentiation[3]. It occurs mainly in parotid gland and rarely in minor salivary glands[4].
Plasmacytoid myoepithelioma is extremely rare in children and adolescents and to our present knowledge only 7 well documented cases of myoepithelioma in patients below 18 years of age have been reported in the literature.We present this case of plasmacytoid myoepithelioma of the hard palate in a 15-year-oldadolescent because of the rarity of this tumor in this age group with the objective of contribution to the better understanding of this tumor leading to its timely diagnosis and early management. In the case reported herein, we discuss clinical, histopathlogical and immunohistochemical findings along with differential diagnosis and management.
Case Report
A 15-year - old femalereported with a swelling of six months duration in posterior part of the hard palate. The lesion was non tender, firm in consistency, measuring 3x2cm, with normal overlying mucosa w.r.t color, texture & temperature. Deglutition was normal. No regional lymphadenopathy was found. Radiographically, no bone resorption was found. Routine laboratory investigations including complete blood counts were within the normal values. No fluid was found on aspiration of the lesional mass. Fine needle aspiration cytology (FNAC) was done but the results were inconclusive. Incisional biopsy was done under LA and the histopathology report revealed myoepithelioma.
Surgical excision extending down to periosteum and including the overlying mucosa along with a margin of uninvolved healthy tissue was done under general anesthesia (Fig. 1A-D).The operation, as well as the postoperative course under antibiotic cover was uneventful, and the patient was discharged home after 5 days. Histopathological report of the excised tissue confirmed the diagnosis of myoepithelioma. The immuno histochemical analysis was done and was found to be positive for S-100 protein but the results were inconclusive. The patient was followed up regularly for two years and six months with no evidence of tumor recurrence (Fig. 1E).
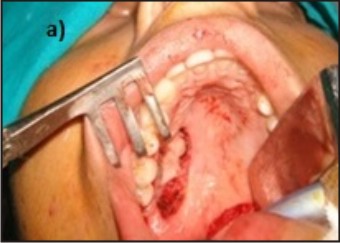 | Fig 1 a) Intraoperative photograph of the patient showing surgical resection
 |
 | Fig 1 b) Intraoperative photograph of the patient showing surgical resection
 |
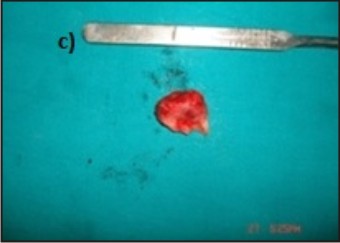 | Fig 1 c) Showing the excised tumor
 |
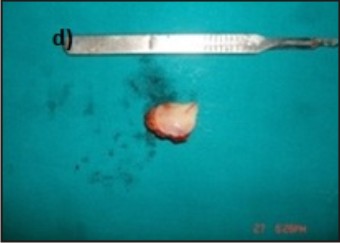 | Fig 1 d) Showing the excised tumor
 |
 | Fig 1 e) Postoperative photograph of the patient after two years and six months with no sign of recurrence
 |
Discussion
Tumors of salivary glands are rare [5] constituting only 3% to 5% of all salivary gland neoplasms in children and adolescents[3]. Myoepitheliomas are located most frequently in parotid gland and less frequently in minor salivary glands of the oral cavity[6]. Myoepitheliomas are most common in the age group of 30 -50 years and very rare in individuals less than 18 years of age.No gender predilection has been reported in literature however male to female (M: F) ratio of 1: 2 was reported by Zelaya et al 4. To our present knowledge, only 7 well documented cases of myoepithelioma of palate in children and adolescents have been reported in literature. (Demographic data presented in Table 1).
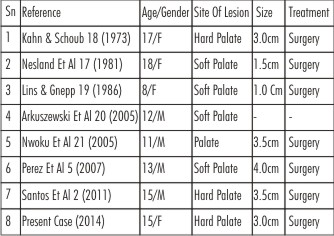 | Table 1 : Reported Cases Of Myoepithelioma Of The Palate In Adolescents.
 |
According to Dardick et al[7] Myoepitheliomas are benign or malignant lesions in which the tumor cells are either spindle shaped or have the range of cytological features seen in the myoepitheliomatous component of typical pleomorphic adenomas[7]. However, in myoepitheliomas there are few (less than 5%) if any luminal epithelial cells forming obvious duct-type structures seen by light microscopy. Tumors in which the ducts comprise of more than 5-10% of the sections under review are classed as pleomorphic adenomas[8]. However, Zelaya et al [4] suggested an alternative diagnostic parameter based on cellular predominance according to which, if myoepithelial predominance is found then it should be named myoepithelioma and if ductal prominence then it should be named pleomorphic adenoma [4].
The clinical presentation as found in the present case is asymptomatic, slow growing sub mucosal mass[1] with no evidence of ulceration[9],[10].Thus the clinical characteristics and overall biologic behavior of Myoepithelioma is similar to Pleomorphic adenoma[3]. Furthermore, it is also essential to know the biologic behavior of its malignant counterpart. Malignant myoepithelioma of the intraoral minor salivary glands is generally a low grade malignant tumor with little propensity for regional or distant metastasis and low recurrence[11].
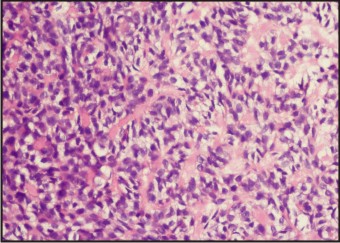
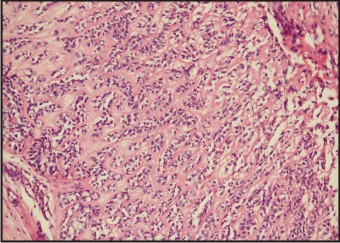
Histopathologically, myoepithelioma is composed almost exclusively of sheets, islands or cords of cells with myoepithelial differentiation that may exhibit spindle, plasmacytoid, epitheloid or clear cytoplasmic features[11]. Plasmacytoid cells are polygonal cells with eccentric nuclei and dense, nongranular or hyaline, abundant eosinophilic cytoplasm. Plasmacytoid cells are found more often in tumors arising in the minor salivary glands than in the parotid gland. These hyaline cells may simulate neoplastic plasma cells, skeletal muscle or “rhabdoid” cells[10]. Although the diagnosis of myoepitheliomas should be made primarily on the basis of their histomorphology, immunohistochemical study can assist in arriving at final diagnosis, as myoepithelial cells are difficult to identify in routine histopathological examination or electron microscopy[6],[7]. In the present case, histopathological examination revealed tumor cells distributed in nests, groups that were separated by myxoid stroma. The individual cells were polygonal to round and had clear to homogeneous eosinophilic cytoplasm, at places showing sheets of plasmacytoid morphology with eccentrically placed nuclei (Fig. 2 & 3).
 | Fig.2 Histopathology Showed Tumor Cells Arranged In Nests And Cords With Intervening Hyalinized Stroma. (H&E × 200)
 |
 | Fig.3 Sheets Of Myoepithelial Cells With Clear Cytoplasm And Occasional Plasmacytoid Cells With Eosinophilic Cytoplasm And Eccentrically Placed Nuclei. (H&E × 400)
 |
The tumor markers recommended for diagnosing myoepithelioma are S-100 protein, Vimentin, α-smooth muscle actin (α-SMA), Cytokeratin 14 (CK14) and Glial fibrillary acidic protein (GFAP)[2],[7]. Normal myoepithelial cells show myogenic differentiation, which is revealed by the presence of actin filaments, as well as filaments of cytokeratin. However, tumoral myoepithelial cells rarely show the same cytoskeleton as normal cells therefore it is suggested that tumor myoepithelial cells might exhibit different stages of differentiation. CK 14 is a useful marker of normal myoepithelial cells that is responsible for the anchorage of myoepithelial cells to the basement membrane. It is usually unexpressed in tumor cells, unless those cells present terminal differentiation so lack of CK14 expression is supposed to be expected[2]. Myoepitheliomas show strong positivity for S-100 protein and is also positive for GFAP[2],[5],[12]. Immunohistochemical expression of vimentin may indicate that myoepithelial cells in tumors such as myoepitheliomas do not reach complete differentiation. The negativity for myogenic markers is expected in plasmacytoid variant so α SMA is negative[2],[7]. In this case report immunohistochemical analysis was found to be positive for S-100 proteinbut the results were inconclusive as these markers are also positive for pleomorphic adenoma. Immunohistochemical staining can assist in diagnosing myoepitheliomas but histopathology still remains the gold standard for diagnosis.
Myoepitheliomas should be differentiated from benign and malignant tumors such as pleomorphic adenoma, adenocarcinoma, nerve sheath tumors, fibrous histiocytoma, nodular fasciitis, synovial sarcoma, leiomyoma, leiomyosarcoma, hemangiopericytoma, solitary fibrous tumor and paraganglioma. Furthermore, myoepitheliomas should be differentiated from malignant neoplasms [13] as the incidence of malignant epithelial salivary gland tumors is almost same as that of benign tumors in children and adolescents[5]. It can be misdiagnosed as a malignant tumor because of the variable architectural pattern with diverse cell types, and frequently increased cellularity and unfamiliar growth patterns [5],[7]. Soft tissue myoepithelial tumors with at least moderate cytologic atypia are clinically malignant [14].
The biological behavior of myoepitheliomas appears to parallel that of the pleomorphic adenoma and, as such, should be treated accordingly[10] .As performed in the current case ,surgical excision is considered the treatment of choice[5]. Most morphologically benign or low-grade myoepithelial neoplasms of soft tissue behave in a benign fashion with a low, but unpredictable risk for local recurrence(approximately20%) [14]. Although these tumors do not present high levels of the recurrence [13] but they can undergo malignant transformation especially in long standing tumors or in tumors with multiple recurrences[15]. In malignant lesions a wider excision must be planned, and lymph node dissection should be considered[16].The possibility of recurrence should be discussed with the patient and parents and regular and long term follow up should be carried out.
References
1. Zormpa MT, Sarigelou AS, Eleftheriou AN, Assimaki AS, Kolokotronis AE. Plasmacytoid myoepithelioma of the palate: case report. Head Neck Pathol. 2011 Jun; 5(2):154-8.
2. Santos EP, Cavalcante DR, Melo AU, Pereira JC, Gomes MZ, Albuquerque RL Jr. Plasmacytoid myoepithelioma of minor salivary glands: report of case with emphasis in the immunohistochemical findings. Head Face Med. 2011 Dec 12; 7:24.
3. Ritwik P, Brannon RB. A clinical analysis of nine new pediatric and adolescent cases of benign minor salivary gland neoplasms and a review of the literature. J Med Case Rep. 2012 Sep 11; 6(1):287.
4. Cuadra Zelaya F, Quezada Rivera D, Tapia Vazquez JL, Paez Valencia C, Gaitán Cepeda LA. Plasmacytoid myoepithelioma of the palate. Report of one case and review of the literature. Med Oral Patol Oral Cir Bucal. 2007 Dec 1; 12(8):E552-5.
5. Perez DE, Lopes MA, de Almeida OP, Jorge J, Kowalski LP. Plasmacytoid myoepithelioma of the palate in a child. Int J Paediatr Dent. 2007 May; 17(3):223-7.
6. Rastogis , Modi M , Dhawan V , Kumar A. Myoepithelioma of palate- A case report and review of literature. J Clin Diagn Res 2008 Oct ;( 2)1095-1099.
7. Dardick I. Myoepithelioma: definitions and diagnostic criteria. Ultrastruct Pathol. 1995 Sep-Oct; 19(5):335-45.
8. Dardick I, Thomas MJ, van Nostrand AW. Myoepithelioma--new concepts of histology and classification: a light and electron microscopic study. Ultrastruct Pathol. 1989 Mar-Jun; 13(2-3):187-224.
9. Sciubba JJ, Brannon RB. Myoepithelioma of salivary glands: report of 23 cases .Cancer 1982 Feb 1; 49(3):562-72.
10. Barnes L, Appel BN, Perez H, El-Attar AM. Myoepithelioma of the head and neck: case report and review. J Surg Oncol. 1985 Jan; 28(1):21-8.
11. Yang S, Li L, Zeng M, Zhu X, Zhang J, Chen X. Myoepithelial carcinoma of intraoral minor salivary glands: a clinicopathological study of 7 cases and review of the literature. Oral Surg Oral Med Oral Pathol Oral Radiol Endod. 2010 Jul; 110(1):85-93.
12. Simpson RH, Jones H, Beasley P. Benign myoepithelioma of the salivary glands: a true entity?. Histopathology. 1995 Jul; 27(1):1-9.
13. Sperandio FF, Giudice FS, Pinto-Junior DD, de Sousa SC. Myoepithelioma of the Soft Palate: a case report giving special attention to the differential diagnosis. J Oral Maxillofac Res 2011 (Jan-Mar); 2(1):e4.
14. Hornick JL, Fletcher CD. Myoepithelial tumors of soft tissue: a clinicopathologic and immunohistochemical study of 101 cases with evaluation of prognostic parameters. Am J Surg Pathol. 2003 Sep; 27(9):1183-96.
15. Cardesa A, Alos L. Myoepithelioma. In: Barnes L, Eveson JW, Reichart P, Sidransky D, editors. World Health Organization Classification of Tumors. Pathology and Genetics of Head and Neck Tumors. Lyon: IARC Press; 2005. p. 259-60.
16. Darvishian F, Lin O. Myoepithelial cell-rich neoplasms: cytologic features of benign and malignant lesions. Cancer. 2004 Dec 25; 102(6):355-61.
17. Nesland JM, Olafsson J, Sobrinho-Simoes M .Plasmacytoid myoepithelioma of the palate -A case report with ultrastructural findings and review of the literature. Journal of Oral Pathology 1981: 10: 14-21.
18. Kahn LB, Schoub L. Myoepithelioma of the palate. Histochemical and ultra structural observations. Arch Pathol. 1973;95:209–12.
19. Lins JE, Gnepp DR. Myoepithelioma of the palate in a child. Int J Pediatr Otorhinolaryngol. 1986; 11:5–13.
20. Arkuszewski P, Przygoński A, Maciuszonek M. Myoepithelioma of palate-case report. Otorhinolaryngol Pol. 2005; 59:875–7.
21. Nwoku AL, Al-Shlash S, Al-Atel A. Pediatric myoepithelioma of the palate. Saudi Med J. 2005; 26:999–1002.
|