Introduction
An osteoma is a benign osteogenic tumor characterized by compact or cancellous bone proliferation. It may be classified as peripheral, central, or extraskeletal. A peripheral osteoma arises from the periosteum, a central osteoma from the endosteum, and an extraskeletal osteoma in the soft tissue[1],[2],[3],[4]. The pathogenesis of osteomas is not completely known. They are referred to developmental anomalies, true neoplasms, or reactive lesions triggered by trauma, muscle traction, or infection [1],[2],[3], [5].
Osteomas are more commonly found in the cortical plate of long bones but they can also affect the maxillofacial region. It is usually asymptomatic and exhibit continuous growth at adulthood but it can grow into large sizes and cause facial asymmetry or severe dysfunction [6], [7], [8], [9]. In these cases, surgery is usually required.Osteomas can cause facial deformity, limitation or deviation of the mandible on opening, headache, bone pain, dysphagia or exophthalmos.[10], [11]
Case Report
A 28-year old female was referred to the Department of Periodontology with the chief complaint of mild swelling on the left side of the face [Figure 1], She was worried about a slow growing marble [Figure 2], like growth in the mandibular left anterior region which persisted for 2.5 years. The patient gave no history of trauma to the region.
Clinical examination revealed slight extraoral swelling on the left side [Figure 1]. The regional lymph nodes were nonpalpable. Intraoral examination revealed a well-defined, oval, immobile mass on the labial plate of the left anterior mandibular 31 and 32 with labial expansion [Figure 1]. The lesion was bony-hard on palpation. The overlying oral mucosa was normal [Figure 2]. There was no pain, tenderness, or paresthesia.Vitality test with 31 and 32 gave a positive response to electric pulp testing. The mass was clinically measuring 1.3 cm (width) and 0.7 cm (height).
A solitary, oval, well-defined radio-opaque lesion was seen on occlusal radiography [Figure 3].
 | Figure 1: Extraoral photograph showing slight facial skin taught on the left side chin of the mandible.
 |
![Figure 2: Intraoral view showing a well-defined, oval swelling covered by normal oral mucosa on the labial plate of the left side [31, 32].](article-image-3689-FIGURE_2_INTRAORAL_VIEW_SHOWING_A_WELL_DEFINED_AND.jpg) | Figure 2: Intraoral view showing a well-defined, oval swelling covered by normal oral mucosa on the labial plate of the left side [31, 32].
![Figure 2: Intraoral view showing a well-defined, oval swelling covered by normal oral mucosa on the labial plate of the left side [31, 32].](images/article-image-enlarge.jpg) |
 | Figure 3: Occlusal radiograph showing a solitary, well-defined radio-opaque mass extending from the left side mandibular central to lateral root area.
 |
These clinical and radiographic features were sufficiently supportive of the working diagnosis of peripheral osteoma. There were no features of Gardner’s syndrome. Since the lesion had a cosmetic problem and was actively growing and caused facial swelling, the patient was prepared for surgery. Under local anesthesia a crevicular incision was given reflecting a mucoperiosteal flap extending from mesial of 33 to mesial of 43 [Figure 4,5]. The lesion was totally removed followed by osteoplasty using a chisel and rotary instruments [Figure 6]. The flap was approximated and sutured with 3-0 silk sutures [Figure 7]. A periodontal dressing was placed [Figure 8]. The excised lesion [Figure 9] was submitted for histopathological examination [Figure 10].
 | Figure 4: Crevicular incision extending from 33 to 43.
 |
 | Figure 5: Mucoperiosteal flap reflected from 33 to 43; showing the bony mass
 |
 | Figure 6: Osteoplasty showing smoothened bony surface
 |
 | Figure 7: Approximation of the Flap and Suturing
 |
 | Figure 8: Periodontal Pack in place
 |
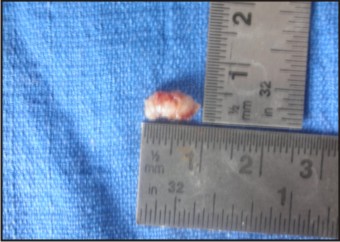 | Figure 9: Bony lesion-1cm/.6cm
 |
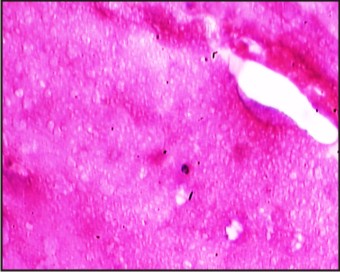 | Figure 10: Histopathology
 |
Postoperatively, the patient received systemic antibiotic, analgesic, along with oral hygiene measures.Periodontal dressing was removed after 24 hours; signs of healing were seen with minimal discomfort. Suture removal was done a week later [Figure 11], and the healing was progressing towards normal at 14 days [Figure 12]. 1 month and 6 months follow- up of the patient showed no post-operative complications [Figure 13].
 | Figure 11: 14 day Post-operative view
 |
 | Figure 12:1month post-operative view
 |
 | Figure 13: 6 months post- operative view
 |
Tissue specimens were fixed in 10% formaldehyde and then decalcified in 8% formic acid solution. They were processed routinely and paraffin embedded. Tissue blocks were cut with 6μ thickness and slides were stained with hematoxylin and eosin. The histopathologic diagnosis confirmed the clinical diagnosis of peripheral compact osteoma with dense lamellae with minimum marrow spaces [Figure 10].
Discussion
Peripheral osteoma occurs most frequently in the frontal, ethmoid, and maxillary sinuses but are not common in jawbones.[12],[13]. In the literature, publishing osteomas in the mandible include 23 cases located in the body [4 cases in the anterior region and 19 cases in the posterior region] followed by the condyle [18 cases], angle [9 cases], ascending ramus [7 cases], coronoid process [5 cases] and sigmoid notch [1 case][14],[15]. In the mandible,The possibility of a reactive mechanism, triggered by trauma or infection, has also been suggested because peripheral osteomas are generally located on the lower border or buccal aspect of the mandible, which are areas susceptible to trauma. It is possible that muscle traction (i.e., masseter, medial pterygoid, temporalis) plays a role in the development of peripheral osteomas [16]. However, in the present case, we have no information on the possible cause because there was no history of previous trauma.
In the present case, the radiological appearance with the clinical aspects such as absence of symptoms, slow growth rate and the location of the lesion are compatible with peripheral osteoma [17]. The lesion may be sessile and attached to the cortical plates with a broad base. If a peripheral osteoma is pedunculated, a narrow contact area can be seen between the lesion and the compact bone [18]. In our case the lesion consisted of dense, uniformly opaque compact bone with a very narrow contact. Sometimes, depending on the location and size of the lesion, it may cause swelling, facial asymmetry, deviation of the mandible on opening, bone pain, headache or exophthalmos and functional impairment [19],[20],[21],[22],[23],[24],[25]. In our case, the increasing size and facial asymmetry was a matter of concern to the patient though without any other clinical symptoms. Recurrence of peripheral osteoma after surgical excision is extremely rare. There are no reports of malignant transformation of peripheral osteoma in the literature [10],[26].
Conclusion
Osteomas can rule out the presence of Gardner's syndrome, which is characterized by a triad of colorectal polyposis, skeletal abnormalities (with multiple osteomas of the skull and face) and multiple impacted supernumerary teeth. Since the osteomas develop before the colorectal polyposis, early recognition of the syndrome is very important to the prognosis of the disease. Recurrence of compact osteoma after surgical excision is rare however Periodic follow up was performed after surgery.
References
1. N. Larrea-Oyarbide, E. Valmaseda-Castellón, L. Berini-Aytés, and C. Gay-Escoda. Osteomas of the craniofacial region. Review of 106 cases.Journal of Oral Pathology and Medicine.2008; 37: 38–42.
2. I.Kaplan, Z. Nicolaou, D. Hatuel, S. Calderon, Solitary central osteoma of the jaws: a diagnostic dilemma. Oral Surgery, Oral Medicine, Oral Pathology, Oral Radiology and Endodontology.2008; 106:22–29.
3. I.Kaplan, S. Calderon, A. Buchner, Peripheral osteoma of the mandible: a study of 10 new cases and analysis of the literature. Journal of Oral and Maxillofacial Surgery.1994; 52:467–470.
4. N. B. Sayan, C. Üçok, H. A. Karasu, Ö. Günhan. Peripheral osteoma of the oral and maxillofacial region: a study of 35 new cases. Journal of Oral and Maxillofacial Surgery. 2002; 60;1299–01.
5. K. U. E. Ogbureke, M. N. Nashed, A. F. Ashraf. Huge peripheral osteoma of the mandible: a case report and review of the literature. Pathology Research and Practice.2007; 203:185–188.
6. White SC, Pharoah MJ. Oral radiology. Benign tumors of the jaws. 2009.
7. Mittal A, Nageshwar I. Large peripheral osteoma of the mandible. Oral Radiol. 2008; 24:39-41.
8. Kerckhaert A, Wolvius E, van der Wal K, Oosterhuis JW. A giant osteoma of the mandible: case report. J Craniomaxillofac Surg. 2005; 33:282.
9. Ogbureke K, Nashed M, Ayoub A. Huge peripheral osteoma of the mandible: a case report and review of the literature. Pathol Res Pract. 2007; 203:185-8.
10. Longo F, Califano L, Maria, Ciccarelli R. Solitary osteoma of the mandibular ramus: report of a case. J Oral Maxillofac Surg. 2001; 59:698-700.
11. De Chalain T, Tan B. Ivory osteoma of the craniofacial skeleton. J Craniofac Surg. 2003; 14:729-35.
12. Kashima K, Rahman OI, Sakoda S, Shiba R. Unusual peripheral osteoma of the mandible: Report of 2 cases. J Oral Maxillofac Surg. 2000; 58:911–3.
13. Bodner L, Gatot A, Sion-Vardy N, Fliss DM. Peripheral osteoma of the mandibular ascending ramus. J Oral Maxillofac Surg. 1998; 56:1446–9.
14. Whaites E. Differential diagnosis of lesions of variable radiopacity in the jaws. 2007.
15. Lanes SR, Borges HO, Machado RA, Cancino CM, Gerhardt OM. Radiographic image of osteomas. Rev Bras Patol Oral. 2005; 4:23-6.
16. Woldenberg Y, Nash M, Bodner L. Peripheral osteoma of the maxillofacial region. Diagnosis and management: A study of 14 cases. Med Oral Pathol Oral Cir Bucal 2005;10 Suppl 2: E139-42.
17. Neville BW, Damm D, Allen CM, Bouquot JE. Patologia oral e maxilofacial. 2004.
18. Durighetto AF, Ramos FM, Rocha MA, Perez DE. Peripheral osteoma of the maxilla: report of a case. Dentomaxillofac Radiol. 2007; 36:308-10.
19. Roy I.D. Peripheral Osteoma of Mandible. MJAFI 2008; 64; 4: 385-86.
20. An SY, An CH, Choi KS. Giant osteoma of the mandible causing breathing problem. Korean J Oral Maxillofac Radiol 2006; 36:217-20.
21. Cautley AJ, Ferguson JW. Cancellous osteoma of the mandibular ramus: a case report. N Z Dent J. 1985; 81:123-4.
22. Bosshardt L, Gordon RC, Westerberg M, Morgan A. Recurrent peripheral osteoma of mandible: report of case. J Oral Surg. 1971; 29:446-50.
23. Cutilli BJ, Quinn PD. Traumatically induced peripheral osteoma: report of a case. Oral Surg Oral Med Oral Pathol. 1992; 73:667-9.
24. Schneider LC, Dolinksky HB, Grodjesk JE. Solitary peripheral osteoma of the jaws: report of a case and review of literature. J Oral Surg. 1980; 38:452-5.
25. Johann AC, de Freitas JB, Ferreira de Aguiar MC, de Araujo NS, Mesquita RA. Peripheral osteoma of the mandible: Case report and review of the literature. J Cranio-Maxillofac Surg 2005; 33:276-81.
26. Ida M, Kurabayashi T, Takahashi Y, Takagi M, Sasaki T. Osteoide osteoma in the mandible. Dentomaxillofac Radiol. 2002; 31:385-7.
|