Introduction:
Cleft lip and/or palate having an incidence of one in 500 children born in India[1], is the commonest cranio-facial abnormality in man[2]. The treatment of children born with a cleft lip and/or palate necessitates long term involvement of healthcare professionals, often requiring several operations, and multidisciplinary management from Plastic Surgeons, Maxillo-facial Surgeons, ENT Surgeons, Orthodontists, and Speech and Language therapists[2],[3].
The paramount issues involved in the treatment of cleft palate are to achieve normal speech without incurring maxillofacial growth disturbances and to minimize hearing loss and middle ear complications[4].
Though total healing by primary intention is the goal of any palate surgeon, invariably there are occasional failures. Common complications resulting from palatoplasty include an occurrence of oro-nasal fistulae and velopharyngeal incompetence[5].
Oro-nasal fistulae, a failure of healing or a breakdown in the primary surgical repair of the palate[6] is a well-known residual condition that occasionally occurs after cleft palate repair[7], [8] as it fails to achieve the ultimate goal of surgery including normal anatomy and function i.e., speech[4],[6]. These fistulas may occur in the labial vestibule, the alveolus, the hard palate, and at the junction between the hard and soft palate[6], [7],[8].
Multiple etiologic factors have been suggested for the formation of oronasal fistulae, including wound breakdown secondary to closure site tension, infection, postoperative flap trauma, hematoma, and hypoxemia[7],[9], [10].
A fistulae draws attention because of the symptoms which includes leakage of fluid into the nose, lodging of food particles within the fistulae and nasal escape of air during speech[7], [8].
Oro-nasal fistulae can influence speech mainly by means of an extra acoustic component caused by air leakage through the fistulae. It has recently been demonstrated that both small and large oro-nasal fistulae can impair velopharyngeal functions and result in hypernasality[7],[9].
The various factors which may contribute to oro-nasal fistulae occurrence in cleft patients include age at the time of palate surgery, extent of cleft, associated congenital anomalies, operative technique and surgeon factor[4], [6], [7], [8], [9], [10], [11].
Various studies have been conducted to evaluate the effect of these various factors on the fistulae occurrence, which also reveals the success rate of their institution in effectively treating such patients with cleft lip and/or palate.
This study focuses on analyzing the post-operative occurrence of oro-nasal fistulae in terms of, its size, site, the extent ofclefting, type of palatal closure and age at palate closure in patients with unilateral and bilateral cleft lip-palate treated at theK.L.E.S Hospital and Medical Research Centre.
Material and Methods :
This study was conducted on 116 patients treated for unilateral and bilateral complete cleft lip-palate, at the Cleft and Craniofacial Centre in K.L.E.S Hospital and Medical Research Centre, Belgaum.
The previous records of all the patients treated at the centre were analyzed for the general information of patient, initial diagnosis, age at the time of primary palatal closure, sex, type of closure and operating surgeon.
Inclusion Criteria:
1. Patients operated at Cleft and Craniofacial Centre in K.L.E.S Hospital and Medical Research Centre, Belgaum, for primary palate closure.
2. Patients with complete unilateral cleft lip-palate, Veau III (Fig 1)
3. Patients with complete bilateral cleft lip-palate, Veau IV (Fig 1)
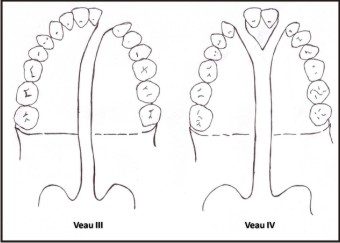 | Fig 1 : Veau Classification Of Cleft
 |
Exclusion Criteria:
1. Patients whose primary palate closure was not performed at Cleft and Craniofacial Centre in K.L.E.S Hospital and Medical Research Centre, Belgaum
2. Patients with incomplete cleft palate and isolated cleft palate.
3. Syndromic Patients.
Procedure :
Patients who followed up at the cleft and craniofacial centre and meet the inclusive criteria were selected. The patient and/or their families were interviewed for a history of leakage of liquids or semisolid foods through the nose and/or speech abnormality.
A careful visual inspection of the original line of cleft for oro-nasal fistulas was carried out using a dental unit lamp, a mouth mirror, and a blunt probe. A series of standard photographs (Frontal, Lateral, Worm’s eye view and intraoral cleft and fistula site) were recorded for each patient.
Making Of Impression:
All visible oronasal fistulas were packed with threaded Vaseline gauze, to prevent overflowing of the impression material in to nasal floor through the fistulae. An alginate impression is made with the Vaseline gauze in place.
Dental casts were prepared from the alginate impressions and were trimmed and polished. All the casts were assessed for the occurrence of Oro-Nasal Fistulae, their location and size.
Evaluation Of The Cast
Location of Fistulae:
Location of fistulae were noted and classified as (Fig 2)
1. Nasoalveolar fistulae (Fig 3a)
i. Prealveolar fistulae.
ii. Alveolar fistulae.
iii. Postalveolar fistulae
2. Hard palate fistulae (Fig 3b, 3c)
i. Anterior hard palate fistulae.
ii. Posterior hard palate fistulae.
3. Fistulae occurring at the junction of hard and soft palate (Fig 3d)
4. Soft palate fistulae (Fig 3e)
i. Fistulae in soft palate.
ii. Uvula.
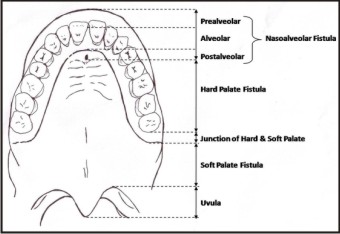 | Fig 2 : Location Of Postoperative Cleft Palate Fistulas
 |
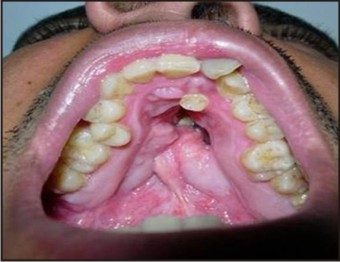
 | Fig 3a : Nasoalveolar Fistulae
 |
 | Fig 3b : Anterior Hard Palate Fistulae
 |
 | Fig 3c : Posterior Hard Palate Fistulae
 |
 | Fig 3c : Posterior Hard Palate Fistulae
 |
 | Fig 3e : Fistulae Of Soft Palate
 |
Size of Fistula:
The maximum anteroposterior and lateral diameter of the fistulae were measured using caliper (Fig 4) and the larger of either were considered as the size of fistula and they were further classified as small, medium, large.
1. Small – A small fistula less than or equal to 5 mm in size. (Fig 5a)
2. Medium – A fistulae measuring 6-10 mm in size. (Fig 5b)
3. Large – A fistulae greater than 10 mm in size. (Fig 5c)
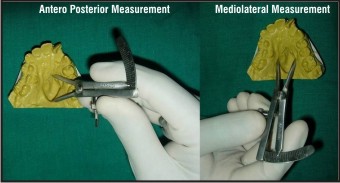 | Fig 4 : Measuring Of Fistulae
 |
 | Fig 5a : Small Sized Fistulae
 |
 | Fig 5b : Medium Sized Fistulae
 |
 | Fig 5c : Large Sized Fistulae
 |
Statistical Analysis
All results were calculated using the mean value and standard deviation for each of the parameters considered and checked for statistical significance using Mann-Whitney U test. Patients developing post-operative Oro-Nasal Fistulae were then compared with those without Oro-Nasal Fistulae. Multiple Logistic regression analysis was used to determine whether there was a significant association between the development of a postoperative fistula and type of cleft palate closure, the severity of cleft, the operating surgeon, the patient’s gender, and the age at cleft palate repair.
Observations And Results
The study sample consisted of 116 patients who followed up at the cleft and craniofacial centre and meet the inclusive criteria out of which 69 (59.5%) are male and 47 (40.5%) are female. 75 (64.6%) out of 116 patients were operated at age of 1-3 yrs, 7 (6%) patients were operated at age of 4-5 yrs, 21 (18.1%) patients were operated at 6-15 yrs, 12 (10.3%) patients were operated at above 15 yrs of age.
Out of 116 operated patients 26 (22.4%) patients had right sided cleft lip and palate, 66 (56.9%) patients had left sided cleft lip and palate and 24 (20.7%) were of bilateral type. 71 (61.2%) of 116 patients were operated by Von Langenbeck’s technique and 45 (38.8%) patients by Wardill Kilner technique. The 116 patients included in the study were operated by 5 cleft patients and were designated surgeon A,B,C,D,E. 15 (12.9%) patients were operated by surgeon A, 60 (51.7%) by surgeon B, 15 (12.9%) by surgeon C, 18 (15.5%) by surgeon D and 8 (7%) patients were operated by surgeon E.
From the series of 116 follow up patients 33 patients with oronasal fistula were selected for the study. Twenty-six fistulae occurred in anterior hard palate, 3 in posterior hard palate, 3 fistulae at the junction of hard and soft palate and one at soft palate. The frequency of fistulae in relation to size and site were summarized in Table 1. Most of the fistulas in the study were of medium size measuring between 6 – 10 mm in size. Only 4 (12.1%) fistulas were of large size measuring > 10 mm.
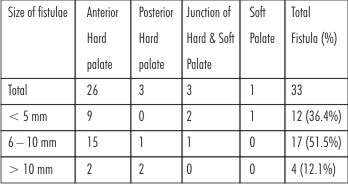 | Table 1: Frequency Of Fistulae In Relation To Size And Site
 |
Incidence offistulae in relation to age of patients at the time of surgery is summarized in Table 2. Fistulae occurrence is more in age group 5 – 15 yrs when compared with other age group. Age at the time palate closure was examined as a continuous variable, and the mean age at closure were compared using student’s ‘t’ test for groups with unequal variance and statistically no difference is seen in the mean age of the two groups.
Eighteen (26.1%) of 69 operated male patients had fistulae and fifteen (31.9%) of 47 operated female patients developed fistulae. Sixteen (24.2%) of operated left sided cleft lip palate patients developed fistulae, eight (30.7%) of operated right sided cleft lip palate patients and 9 (37.5%) of 24 operated bilateral cleft lip palate patients developed fistulae.
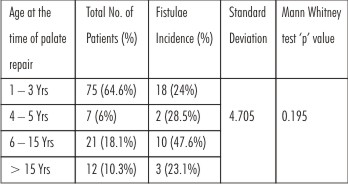 | Table 2: Incidence Of Fistulae – In Relation To Age At Surgery
 |
Incidence of fistulae in relation to type of surgery is summarized in Table 3. Patients operated with Von Langenbeck Variantshows a mild higher degree of fistula incidence though statistically no significant correlation is noted between the type of palate closure and incidence of Oro-Nasal Fistulae. Incidence of fistulae in relation to operating surgeon is summarized in Table 4. Even though incidence of Oro-Nasal Fistulae is more with Surgeon C, D and E when compared with Surgeon A and B, difference is statistically not significant.
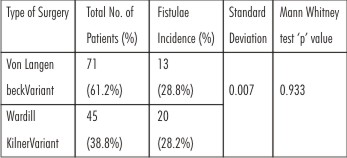 | Table 3: Incidence Of Fistulae – In Relation To Type Of Surgery
 |
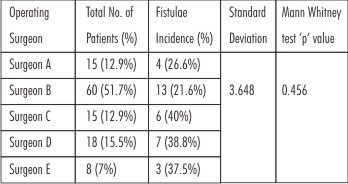 | Table 4: Incidence Of Fistulae – In Relation To Operating Surgeon
 |
None of the parameters considered in the study are statistically associated with the incidence of Oro-Nasal Fistulae. When we run Multiple Logistic Regression test, the same result was obtained. Table 5 summarizes the same.
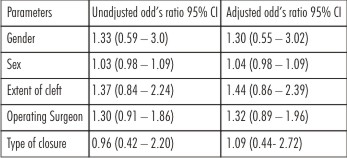 | Table 5: Multiple Logistic Regression Results
 |
Discussion
The paramount issues involved in the treatment of cleft palate are to achieve normal speech without incurring maxillofacial growth disturbances and to minimize hearing loss and middle ear complication[4], [15]. The occurrence of a fistula after palate repair clearly compromises these goals and represents a challenging management problem for the cleft treatment team[20].
In his discussion on Schultz’s paper, Randallemphasized the difficulty in achieving an intact palate after a fistulae had occurred[6]. He also felt that “an open discussion of the problems associated with cleft palate surgery was very helpful and therefore praised Dr.Schultz in this regard.
As rightly stated “Oro-Nasal Fistulae occurrence is not a complication but is a failure to achieve the purpose”. Evaluating the incidence of Oro-Nasal Fistulae and hence the success rate of each cleft and craniofacial centre, becomes vital in providing best treatment.
Stimulated by the need for ongoing review of problem areas in cleft palate surgery, we undertook a review of the factors influencing the occurrence of cleft palate fistulae in our patient population. In this study 116 patients out of thousands treated for unilateral and bilateral complete cleft lip-palate, at the Cleft and Craniofacial Centre in K.L.E.S Hospital and Medical Research Centre, Belgaum, were assessed.
While reviewing the literature, it became clear that there were, several shortcomings in the literature on cleft palate fistulae, and therefore, definite conclusions were difficult to establish. For one, cleft palate fistulae was a potpourri of fistulous “openings” and included both persistent and unrepaired fistulas and new communications between nasal and oral cavity[6]. Until a uniform definition of palatal fistulae is utilized, it will be difficult to compare the results of different studies. Accordingly, we excluded all nasal alveolar fistulas and/or anterior palatal fistulas that were intentionally not repaired at the time of cleft palate closure.
To get a more uniform study population we included in our study only patients with unilateral and bilateral complete cleft lip and palate. Incomplete cleft palate and isolated cleft palate patients were excluded from the study.
In accordance to Fogh-Andersen that, complete cleft lip and palate is more common in males our study also revealed that there was 69 (59.5%) male patients with complete cleft lip and palate than females who accounted to 47 (40.5%) in number (Table1).
In our study maximum number of patients were with left sided cleft lip and palate (56.9%) followed by right sided cleft lip and palate (22.4%) and least number of complete bilateral cleft lip and palate (20.7%) (Table 3), which was similar to Wilson41 report stating that unilateral left sided clefting, unilateral right sided clefting and bilateral clefting occurs in a 6:3:1 relationship.
When reviewing the previous record of all these patients, most of them (64.6%) were operated in the age group ranging from 1 – 3 yrs (Table 2) in accordance to our protocol for treating cleft patients. But however, there were patients whose primary palate repair was carried out in later years because of delayed presentation of the patients forthe primary surgery.
Von Langenbeck Variant was used for primary palate closure of 71 patients (61.2%) included in the study population andWardill Kilner Varient type of palate closure for 45 (38.8%) patients (Table 4). Amaratunga[7] in his report stated that more fistulae were found in the alveolar region in patients whose palates were repaired by the Langenbeck method than with Wardill’s method. He adds that this may be because Langenbeck’s method does not effect a closure in the alveolar region. Unless this region had been repaired at the time of lip repair Langenbeck’s method is bound to leave a defect. Also in his study the rate of junctionalfistulae also proved to be higher with Langenbeck’s method than with Wardill’s. This may be because Wardill’s method gives better access to the posterior border for a more complete detachment of the aponeurosis and muscle attachment.
Site of Fistulae Occurrence:
In our study 87.9% of fistulae occurred in hard palate (29 out of 33 patients) with 3 patients at the junction of hard and soft palate (9.1%) and 1 patient at soft palate (9.1%). Anterior hard palate had the maximum incidence of fistulae accounting up to 26 out of 33 patients (78.8%). This result is in accordance to Muzaffar et al.[4] who reported that more significant fistulae in his study were located in the anterior hard palate. Also Cohen et al.[6] and Rohrich et al.[15] in their study reported increased incidence of fistulae in hard palate. In contrast Amartunga[7] in his study revealed a increased incidence of fistulae at the junction of hard and soft palate in patients whose palates were repaired by the Langenbeck’s method than with Wardill’s. This may be because Wardill’s method gives better access to the posterior border for a more complete detachment of theaponeurosis and muscle attachment.
Size Of Fistulae:
Most of the fistulas in our study 17 (51.5%) out of 33 fistulae were of medium sized measuring 6 – 10 mm in size and 12 (36.4%) fistulae out of 33 were of small size measuring < 5 mm in size and only 4 (12.1%) out of 33 were of large size measuring > 10 mm in size. In contrast Cohen et al.[6] reported that most of the fistulas in his study measured 1 - 2 mm in size (47%) and only 16% were greater than 5 mm in size.
Other factors Studied
Sex of the Patient :
In our population, there was no significant association (p = 0.495) between the fistulae occurrence and sex of the patients as in many other studies who reported the same[4], [6]. In his report Amaratunga[7] stated that a large proportion of males were in the group with fistulae than in the original sample of cleft palate patients and he also expressed that this seem to occur more commonly in males for some unknown reasons. However in our study no such association has occurred.
Age at the time of Primary Palate Closure :
The optimal age at which to perform palatal closure has been a matter of controversy. With respect to fistula formation, a slightly higher incidence was found in patients operated at the age group between 5 – 15 yrs when compared with other age groups (Table 2), this was of borderline significant, and its relevance, if any, is unclear. Also age at the time of palate closure was examined as a continuous variable, and the mean age at closure were compared using student’s ‘t’ test for groups with unequal variance and statistically no difference (p = 0.239) is seen in the mean age of the two groups. This results of our’s are in accordance with other studies[4], [6] who also reported absence of correlation with fistulae incidence and age at the time of primary palate repair. Roger et al.[10] reported a slightly higher incidence of fistulae in patient operated at the age group of 12 – 25 months than patients operated at age group < 12 months but was of borderline significance.
Side of Clefting :
Cohen et al.[6] used the Veau classification to estimate the magnitude of the preoperative defect, because it was impossible to determine retrospectively the size of defect on the basis of patients records which was true in our study also. But as we excluded all the incomplete and isolated cleft palate cases from our study to get a more uniform inclusive criteria we tried to compare unilateral and bilateral complete cleft lip and palates in our study. As expected, the more extensive the original cleft (as reflected by the Veauclassification), the more likely it was that a fistula would occur after palate closure. Even though fistula occurrence is more in bilateral complete cleft lip and palate (Veau IV) than unilateral complete cleft lip and palate (Veau III), there was no much statistical significance to prove it (p = 0.447). These findings agree with those of Emory et al.[10], who, did not find any correlation between fistula occurrence and extent of clefting. In contrast Arshad et al.,[4] and Karling et al.[9] , quoted a significant association between fistulae occurrence and Veau classification of the original cleft palate with more incidence with Veau III and Veau IV type of cleft. Cohen et al.,[10] in parallel with other reports stated that, the extent or severity of the cleft was a significant predictor of patients in whom cleft palate fistulae would develop.
Operating Surgeon:
In a six-centre international study on patients with clefts of the lip and palate, it was determined that the participation of high-volume operators was associated with good outcomes and low-volume operators with poor outcomes[10]. Stating this, Emory et al.[10] registered that the strongest predictor of the occurrence of a cleft palate fistulae was the surgeon performing the procedure. In contrast, our study revealed that incidence of fistulae is more with Surgeon C,D, and E when compared with Surgeon A and B who were the senior surgeons, but the difference is statistically not significant (p = 0.456). Our results go hand in hand with reports by Cohen et al.[6] and Muzaffer et al.[4] who also stated the same.
Technique of Palate Closure:
Not a single technique holds well in all hands. Although Cohen et al.[6] and Karling et al[9] found a higher fistulae rate among patients undergoing Wardill-type palatoplasty and Cohen et al.[6] also recommend avoidance of Wardill-type closures wheneverfaesible, Amartunga[7] noted a higher fistulae rate in patients repaired with the Von Langenbeck palatoplasty. However, Schultz[20] found no correlation between the type of palatoplasty and the rate of fistulae occurrence. There is no clear consensus in the literature as to which particular type of palatoplasty may be more prone to fistula formation. In our study patients operated by VonLangenbeck variant had a mild higher incidence of fistulae than the other type but the result was not statistically significant as stated in Table 3 (p = 0.933).
Though the operating Surgeon have some influence on fistula occurrence none of the other parameters considered in our study including sex of the patient, age at the time of primary palate surgery, the side of cleft and type of closure done are statistically associated with the incidence of Oro-Nasal Fistulae. When we run Multiple Logistic Regression test, the same is confirmed (Table 5).
It should be noted that because of the small number of cases with fistulas, the power of the statistical tests is low; this factor may account for the absence of other statistically significant association in this study.
Over 160 years have elapsed since the first successful cleft palate repairs. Despite advances in the assessment of success of a palate repair, a universal philosophy for repair of the cleft palate has not evolved. A major challenge in the management of the cleft palate patient is to settle the controversy surrounding various parameters of palate repair. Strict adherence to scientific method as well as cooperation among various specialties will help resolve this question. It is hoped that this study will stimulate others to evaluate their treatment outcome in an objective scientific manner.
Conclusion
This study was attempted to determine the incidence of cleft palatal fistulae in a series of nonsyndromic complete cleft lip and palate children treated at our institution and also to assess the possible contributing factors towards the occurrence of Oro-Nasal Fistulae which includes the type of cleft, age at primary palate closure, type of closure and operating Surgeon.
Our study results supported certain statement reported in the literature regarding the occurrence of cleft palate which included that complete cleft lip and palate were common in males than females and unilateral left sided cleft lip palate are common.
The present study indicates a high incidence of fistulae in the hard palate region and most were of size ranging from 6 – 10 mm i.e., medium sized fistulae.
And the various factors considered which includes sex of the patient, age at the time of primary palate closure, side of the cleft and technique of closure did not have any contribution towards the occurrence of the oro nasal fistulae. Operating surgeon showed a mild influence towards occurrence of fistula though statistically not much significant.
In conclusion we state that such institutional studies act as surgical audits and give a rough indication of the factors that affect the occurrence of the cleft palate fistulae and thus help in improving the treatment quality and surgeons efficiency in treating the cleft patients.
Reference :
1. Radhakrishna U, Ratnamala U, Gaines M et al. Genomewide scan of nonsyndromic cleft lip and palate in multigenerational Indian families. The American Journal of Human Genetics 2006;79(3):580-5.
2. D.S. Inman, P. Thomas, P.D. Hodgkinson, C.A. Reid. Oro-nasal fistula development and VPI following primary cleft palate surgery—an audit of 148 children born between 1985 and 1997. British Journal of Plastic Surgery 2005;58(8):1051-4.
3. Bardach, J., Morris, H., Olin, W et al. Late results of multidisciplinary management of unilateral cleft lip and palate. Ann. Plast. Surg.1984;12: 235-2.
4. Muzaffar, A. R., Byrd, H. S., Rohrich, R. J et al. Incidence of cleft palate fistula: An institutional experience with two stage palatal repair. Plast. Reconstr. Surg. 2001;10:1515-8.
5. Schendel SA, Lorenz HP, Dagenais DMS, et al. A single surgeon’s experience with the Delaire palatoplasty. Plast Reconstr Surg. 1999;104:1993–7.
6. Cohen, S. R., Kalinowski, J., LaRossa, D., et al. Cleft palate fistulas: A multivariate statistical analysis of prevalence, etiology and surgical management. Plast. Reconstr. Surg. 1991;87:1041-7.
7. Amaratunga, N. A. Occurrence of oronasal fistulas in operated cleft palate patients. J. Oral Maxillofac. Surg. 1988;46:834-7.
8. Kirschner R, Cabiling DS, Slemp AE., et al. Repair of oronasal fistulae with acellular dermal matrices. Plastic and Reconstructive Surgery. 2006;118(6):1431-1440.
9. Karling J, Larson O, Henningsson G. Oronasal fistulas in cleft palate patients and their influence on speech. Scand J PlastReconstr Hand Surg 1993a;27:193-1.
10. Emory, R. E., Jr., Clay, R. P., Bite, U., and Jackson, I. T. Fistula formation and repair after palatal closure: An institutional perspective. Plast. Reconstr. Surg. 1997;99:1535-8.
11. Sze Yuen Anthony Mak, Wai Hong Wong, Chi Kong Or, and Angela Ming-See Poon. Incidence and Cluster Occurrence of Palatal Fistula After Furlow Palatoplasty by a Single Surgeon. Ann Plast Surg 2006;57: 55–59
12. Marcks, K.M., Travaskis, A.E., and Tuerk,M., 100 Palatoplasties. Plast. Reconstr. Surg. 1955;16(5):352-1.
13. Dalston RM, Marsh JL, Vig KW, Witzel MA, Bumsted RM. Minimal standards for reporting the results of surgery on patients with cleft lip, cleft palate, or both: a proposal. Cleft Palate J 1988;25(1):3–7.
14. Moore MD, Lawrence WT, Ptak JJ, et al. Complications of primary palatoplasty: A twenty-one-year review. Cleft Palate J 1988;25:156-2.
15. Rohrich, R. J., Rowsell, A. R., Johns, D. F., et al. Timing of hard palatal closure: A critical long-term analysis. Plast. Reconstr. Surg. 1996;98:236-46.
16. Jolleys, A., and Savage, J.P. Healing defects in cleft palate surgery: The role of infection. Br. J. Plast. Surg. 1963;16:134-9.
17. Masatsugu Shimizu, Yanagisawa Shigetaka, Harumi Mizuki., et al. Oronasal fistulae in repaired cleft palates. Journal of Cranio-Maxillofacial Surgery. 1989;17(1):37-8.
18. Wilhelmi BJ, Appelt EA, Hill L, et al. Palatal fistulas: rare with the two-flap palatoplasty repair. Plast Reconstr Surg. 2001;107:315–8.
19. Bresnick S, Walker J, Clarke-Sheehan N, et al. Increased fistula risk following palatoplasty in Treacher Collins syndrome. Cleft Palate Craniofac J. 2003;40:280 –3.
20. Schultz RC. Management and timing of cleft palate fistula repair. Plast. Reconstr. Surg. 1986;78(6):739-7.
21. Bardach J, Morris HL, and Olin WH. Late results of primary veloplasty: The Marburg Project. Plast. Reconstr. Surg. 1984;73(2):207-4.
22. Pigott RW, Albery EH, Hathorn IS., et al. Comparison of Three Methods of Repairing the Hard Palate. Cleft Palate–Craniofacial Journal, July 2002;39(4):329-8.
23. Mommaerts MY, Combes FAAM, Drake D. The Furlow Z-plasty in teo-staged palate repair modifications and complications. Br J of Oral and Maxillofacial Surgery. 2006;44:94-9.
24. Eric R. Helling, M.D. Vipul R. Dev, M.D. Jaime Garza., et al. Low Fistula Rate in Palatal Clefts Closed with the Furlow Technique Using Decellularized Dermis. Plast. Reconstr. Surg. 2006;117:2361-5.
25. Clark DE, D'Antonio LL, Liu JR, Welch TB Radiographic demonstration of oronasal fistulas in patients with cleft palate with the use of barium sulfate contrast. Oral Surg Oral Med Oral Pathol. 1992;74(5):661-70.
26. Tania C.Murphy, Derrick R.Willmot., Image analysis of Oronasal Fistula in Cleft Palate Patients acquired with an Intraoral camera. Plast. Reconstr. Surg. 2005;115:31-7.
27. Brennan PA, Marus AF, Flood TR., et al. Do oral flora colonize the nasal floor of patients with oronasal fistulae?. Cleft palate-Craniofacial Journal, July 2001;38(4):399-0.
28. Brennan PA, Willy P, Rajiv Anand.m et al. Colonization of the cleft nasal floor by anaerobic oal flora in patients with oronasalfistulae. Cleft palate-Craniofacial Journal, July 2003, 40(4):431-2.
29. Shelton RL, Blank JL. Oronasal fistulas, intraoral air pressure and nasal airflow during speech. Cleft Palate J 1984;21:91-9.
30. Abyholm, F. E., Borchgrevink, H. H., and Eskeland, G. Palatal fistulae following cleft palate surgery. Scand. J. Plast. Reconstr. Surg. 1979;13:295-0.
31. Jackson MS, Jackson IT, Christie FB. Improvement in speech following closure anterior palatal fistulas with bone grafts. British Journal of Plastic Surgery. 1976;29:295-6.
32. Berkman MD. Early non-surgical closure of postoperative palatal fistulae. Plastic and Reconstructive Surgery 1978;62(4):537-1.
33. Posnick JC, Stanley BG. Surgical closure of end-stage palatal fistulas using anteriorly-based dorsal tongue flap. J Oral andMaxillofac Surgery 1987;45: 907-2.
34. De Mey A, Malevez C, Lejour M. Treatment of palatal fistula by expansion. British Journal of Plastic Surgery 1990;43:362-4.
35. Lehman JA, Curtin P, Haas DG. Closure of anterior palate fistulae. Cleft Palate Journal 1978;15(1):33-8.
36. Bless DM, Ewanowski SJ, Dibbell DG. A technique for temporary obturation of fistulae. Cleft Palate Journal, 1980;17(4):297-0.
37. Isberg A, Henningsson G. Influence of palatal fistulas on velopharyngeal movements: A Cineradiographic study. Plastic and Reconstructive Surgery, 1987;79(4):525-0.
38. Honnebier MB, Johnson DS, Parsa AA., et al., Closure of palatal fistula with a local mucoperiosteal flap lined with buccalmucosal graft. Cleft Palate-Craniofacial Journal, 2000;37(2):127-9.
|