Introduction
Dental implants are a valuable aid to the restoration of form and function of the oral cavity. Replacement of missing teeth can be achieved preferably by implants as compared to standard fixed and removable dental prostheses. Success of dental implants depends on good osseointegration with the bone. Meticulous planning and careful surgical procedures are required for the placement of dental implants. The success of any implant treatment depends on careful preoperative planning.
In addition to a thorough an amnesis and clinical examination, radiographic assessment is essential to estimate the morphologic characteristics of the proposed implant site and the location of anatomical structures. A combination of a limited bone volume and poor bone quality may lead to less predictable bone apposition and early implant failures. In each instance, the imaging strategy most appropriate for a particular phase of implant therapy should always be based on the collective decision of the implantologists. Radiographic examination of a proposed implant site is an essential step in the presurgical evaluation of a patient requiring dental implant surgery. In the clinical practice of implantation, radiographic imaging assists in the therapy, preoperative treatment planning, surgical procedure, and in the postoperative assessment and ongoing implant function.Various imaging options are available for the evaluation of the recipient site .[1],[2],[3] Panoramic radiographs will provide information on the gross anatomy of the jaws and related anatomical structures. Due to inherent distortions, these images are less well suited for estimating the amount of alveolar bone, particularly in the horizontal planes.[4] Furthermore, another drawback associated with panoramic radiography is its inborn unsharpness, which impedes detailed diagnosis in the jawbone. The intraoral periapical image is valuable for an estimate of the mesio-distal dimension of the potential implant site, as well as a preliminary estimate of the vertical dimensions. A combination of panoramic and intraoral views is often recommended for a preliminary evaluation of the intended implant site.
However, an obvious limitation of these radiographic methods is that they do not provide information on the bucco-oral width or angulations and concavities in the alveolar process, and therefore, it may be preferable to supplement these examinations with some form of cross-sectional tomographic imaging. So far, there is no consensus regarding the guidelines for pre-implant radiographic planning. In a position paper by the American Academy of Oral and Maxillofacial Radiology, recommended that conventional cross-sectional tomography should be the method of choice for most implant patients. Nevertheless, the authors emphasize that currently there is no scientific evidence for that recommendation.[5]
Diagnostic imaging for implantology
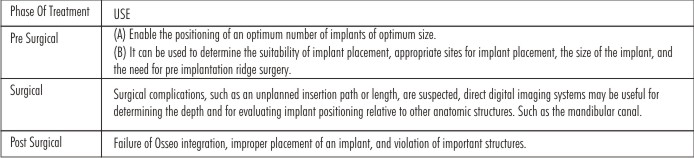
In the clinical practice of implantation, radiographic imaging assists in the therapy, preoperative treatment planning, surgical procedure, and in the postoperative assessment and ongoing implant function.
Successful Diagnostic Imaging Showed Fulfill following criteria
1. Cross-sectional views for the visualization of the spatial relationship of internal structures(such as the inferior alveolar canal, mental foramen, maxillary sinuses, and incisive canal)
2. Minimal image distortion.
3. Depiction of the density of the cancellous bone and thickness of the cortical plates of the bone.
4. Minimum radiation dose.
5. Orientation of the axis of alveolar height.
6. Pre-existing pathology.
Why radiographic technique so important?
The purpose of the pre-implant examination is first of all to decide whether implant treatment is appropriate for the patient, and whether it is possible to accomplish. Furthermore, this examination should estimate the prognosis as well as aid in preparing the treatment. Assessment of bone quantity, such as the height of the alveolar process, the bucco-lingual width, the angulation, and the detection of possible undercuts and concavities, is a prerequisite for the planning of implant placement in the jaws. A clinical examination including analysis of study casts may be helpful in estimating the morphology of the alveolar process. However, it cannot be taken for granted that the morphology of the alveolar process covered with mucosa agrees with that of the underlying bony layer. Therefore, it has been suggested to assess the size and shape of the alveolar bone by “bone sounding” (also termed “ridge mapping”) .[6], [7]
Following local anesthesia, the thickness of the mucosa is measured by penetrating the soft tissue with e.g. a periodontal probe at various sites in the region. To facilitate interpretation, the measurements of the mucosa thickness may be transferred to a sawed-through cast model. Radiography is an alternative, non-invasive technique for determining presurgically the alveolar bone quantity as well as the quality. In order to avoid morbidity caused by the surgical procedure, it is essential to know the location of vital anatomical structures such as the inferior alveolar nerve and the extension of e.g. the maxillary sinus. Another yield of the radiographic examination is to identify possible pathological conditions. As will appear from the above, radiographic examination may be regarded as an indispensable part of the implant treatment planning. The information acquired from radiography should be used to estimate the length and width of the implant to be inserted, the appropriate number of implants, the location and orientation, and the possible need for additional treatment before implant placement, for instance bone augmentation procedures.
Imaging Techniques
When implant treatment is considered, a large variety of radiographic imaging techniques exist for the preoperative planning. The choice of technique, projections, and number of exposures depend on the region of the suggested implant treatment in particular, but also other factors should be considered. If severe bone resorption of the jawbone or anomalous anatomical conditions can be expected from the clinical examination, or bone augmentation procedures have been performed before implant surgery, this will influence the choice of examination. Furthermore, the accessibility of radiographic equipment, the financial costs, and radiation risk estimates play an important role. Ideally, the goal of the radiographic examination is to achieve as much information on the jawbone as possible and at the same time minimize the radiation burden to the patient as well as the costs. All types of imaging techniques possess both advantages and disadvantages, and a combination of different methods may be used in order to optimize the diagnostic outcome. In the following, different radiographic methods will be discussed with regard to their strengths and weaknesses that may be of importance in relation to implant planning.
 | Role of Radiograph in Implant
 |
1. Intraoral Periapical radiography
By the use of reference images from mandibular sections presenting three defined classifications for bone trabecular patterns, it is possible to assess the trabecular pattern in intraoral radiographs with high diagnostic accuracy.[8] Periapical radiographs can be useful in identifying the approximate location of anatomical structures as well as the relative parallelism of roots adjacent to an edentulous site. Occlusal radiographs are capable of demonstrating the bucco-lingual width of the alveolar ridge in the mandible. A limitation of this method is that the images only display the maximum width of the alveolar process. The dimensional accuracy is poor in intraoral radiography due to inherent magnification and distortion.[9],[10] The technique is, however, readily available and rather inexpensive.
2. Panoramic radiography
A panoramic image yields an overview of the jaws and the general status of possible remaining teeth. It is most useful in the preliminary evaluation of the implant site. An obvious drawback is that the panoramic radiograph does not provide information on the bucco-lingual width of the alveolar process. Similar to intraoral radiography, some degree of magnification and distortion is inevitable in panoramic views. The magnification varies more in the horizontal plane than in the vertical plane, and it depends on the equipment, the position of the patient, and the location in the arch.[11] Studies have thus shown that distance measurements in panoramic images are unreliable.[12],[13] Babbush (1991) has described a method to overcome the magnification problem.[14] A reference, e.g. a metal ball, with known dimensions may be placed in the region of interest making it possible to determine the actual magnification in both planes. Some advantages of panoramic radiography are low costs and a rather high availability.
3. Lateral Cephalography
Profile radiographs have been proposed as part of presurgical implant planning.[15],[16] These images provide information on the relationship between the upper and lower jaw in the sagittal plane, the inclination, the bucco-lingual width, and the vertical height of the jawbone in the anterior region. Furthermore, knowledge of the anatomical structures in this region can be obtained. Since information from cephalograms is limited to the midline of the maxilla and mandible, this radiographic method has become less suitable concurrently with the advance of cross-sectional imaging techniques.
4. Conventional cross-sectional tomography
Because information on the jawbone in all three dimensions is needed for implant treatment planning, it may be preferable to supplement the aforementioned radiographic techniques with cross-sectional imaging. Tomography may produce cross-sectional views in any jaw location making it possible to accurately assess the alveolar bone height, bucco-lingual width and inclination, and furthermore, the spatial relationship of the anatomical structures at the recipient site. The principle of this method is blurring of the structures lying outside the image layer of interest, which can be achieved by a coordinated movement of the x-ray source and the film. The effectiveness of this blurring depends on the tomographic motion that can be linear or multidirectional (hypocycloidal, spiral). The more complex motions, the more effective and uniform blurring can be produced. The tomographic equipment is able to produce image layers of different thickness. The interpretation of the resulting tomograms is often rather difficult and calls for some experience. To aid the orientation of the images, it is preferred to place metallic markers at strategic sites in the mouth before the radiographic examination, which afterwards can serve as references for the exact location of the slices. The advantages of conventional tomography include uniform magnification and moderate expenses (compared with computed tomography). The availability of this method has increased recently, since dental schools, hospitals, and private practices are more prone to purchase tomographic equipments concurrently with their reduction in price.
Digital radiography has advantages over film radiography, one of which is the ability of image manipulation that may result in enhanced diagnostic information.[17] In addition, software programs have been developed that may aid in simulating placement of an implant in the patient before surgery by using a template on the radiograph (SIM-Plant, Columbia Scientific Inc., Columbia, Md.; Implant Planner, Gotfredsen, Aarhus).
5. Computed tomography
An advanced digital radiographic technique proposed for implant treatment planning is computed tomography, also called CT scanning or just CT. Like conventional tomography, this method is able to produce cross-sectional cuts of the jawbone. The technique was introduced by Hounsfield (1973) in the 1970s, and was based on cross-sectional imaging in the axial plane.[18] Attempts were made to produce direct coronal and sagittal images similar to film tomograms, but this direct procedure has limitations when applied to the clinic.[19] Instead, computer software was developed, capable of transforming the data of these axial slices into panoramic images and multiplanar cross-sectional images. This transformation is also known as reformatting or reconstruction. In the late 1980s, commercial programs were developed for application of CT to presurgical implant planning. The advantages of CT include: multiplanar views, high contrast, image layer free of blurring, uniform magnification (”real-size” imaging is possible), availability of image analysis by computer, and 3-dimensional reconstruction. In addition, many implant recipient sites can be evaluated in one exposure. However, computed tomography is also associated with limited accessibility, high expenses, and high radiation doses. Another problem is that presence of metallic restorative materials can cause streak artifacts. For that reason, CT may be more appropriate in the treatment planning of fully edentulous patients.
6. Magnetic resonance imaging
Magnetic resonance imaging was first introduced by Lauterbur.[20] Magnetic fields and radiofrequencies, which are used by electromagnetic detectors to provide electronic images of body protons, are processed by a computer that generates them as digital images. There is no exposure toradiation and soft tissues can be visualized when MRI is used. It can be used as a secondary imaging technique when primary imaging techniques such as complex tomography and CT scanning are not satisfactory.[21] The magnetic field strength used in MRI (up to 3.0 Tesla) is unlikely to cause tissue damage. It is believed that a much greater magnetic field strength could lead to marked heating of tissues but this potential heating problem has been overcome by the use of an advanced imaging excitation sequence. Devge et al.[22] found that MRI images are not affected by implants of the Branemark system. On the other hand, MRI is contraindicated for patients with ferromagnetic metallic implants in their bodies because of the potential risks associated with movement or dislodgment of such objects.[23] It has recently been proposed that MRI be used as an alternative technology for implant planning to avoid the radiation hazards associated with the use of CT.[24],[25],[26]
New generation radiographic technique
(A) HELICAL CT
The new generation scanners are faster and have significantly lower radiation dose. The scan should be limited to the area of interest and avoid radiosensitive tissues such as the eyes. In place of conventional film, radiation is detected by highly sensitive a crystal or gas detector which is then converted to digital data. This data stored and manipulated by computer software to produce a grey-scale image. The software then allows multiplane sections to be reconstituted, the qualities of which are dependent on the original scan selection thickness and the integers between successive sections. Images produced as:
Standard radiographic negative images on large sheets.
Positive images on photographic paper.
Images for viewing on a computer monitor.
The patients head is aligned in the scanner with light markers, and a scout view is obtained which gives an image similar to a lateral skull film. Radiations dose of thin scout view is low; can be repeated if alignment incorrect.
Generally, mandible scanned with slices parallel to the occlusal plane; maxilla using the same plane or parallel to the floor of the nose. If there is a deviation from this alignment, the cross sectional slices will not be in the same direction as the proposed implant placement. Heavy metals will produce a scatter-like interference pattern if present in the slice, and the interference will appear in all the generated sectional images. Extensive interferences renders a CT scan unreadable. Interferences can be produced by large posts in root canals or heavily restored teeth. The various scan images can be measured for selection of implant length and diameter. The nominal magnification of the images is 1:1; but some machines and cameras produce images where the magnification may vary. In such cases, a scale is usually incorporated alongside the various groups of images and the real magnification determined. A correction factor can then be applied to measurements taken directly from the films.
(B) Simplant
Simplant is a computer based image software programme where it is possible to produce images of implants and their restorative components which can then be placed within the ‘CT scan’. Hence the relationship between the proposed implant and ridge morphology, anatomic features and the adjacent teeth can be evaluated. In July 1993, the first version of Sim/Plant was released. With this software, the dental clinician could visualize a patient’s axial, cross-sectional, and panoramic views on one screen and place virtual implants. In 1999, with the introduction of Simplant 6.0, the ability to create 3-dimensional (3D) reformatted images was added to the software.[27]
(C) SCAN ORA
Scan ora is a new generation sophisticated tomographic device similar to conventional DPT machines, but with facilities to generate high quality sectional images. In CT scanning, the sectional images are software generated; but the scan ora produces a tomographic image directly onto film. Scan ora uses complex broad beam spiral tomography and is able to scan in multiple planes. The scans are computer controlled with automatic execution; but they still rely heavily on good patient positioning and experience in using the machine. The patients head is carefully aligned within the device and this position recorded with skin markers and light beams. A DPT image is produced from which the sites which require sectional tomographic data determined.
The patient is repositioned in exactly the same alignment and the appropriate tomographic programme selected for the chosen region of the jaw. Scan ora magnification- 1.3 X or 1.7 X for routine DPT; but 1.7 for all sectional images.Tomographic sections = normally 2mm or 4mm thickness; scan sections are thicker and fewer; hence overall patient dose much less than a CT scan. Transparent overlays depicting implants of various lengths and diameters at the corresponding magnifications can be superimposed directly on the radiographs which provide a simple method of assessing implant sites and implant placement at different angulations. Scanora units give considerably lower radiation doses than does CT and their cost is approximately one-fifth of that of a CT machine. [28],[29]
(D) Computerized digital radiovisiography (CDR )
It provides an alternative medium to produce an image. Here, the detectors are solid state; hence the doses can be greatly reduced. Also, manipulation of the digitally derived image can provide further information about relative bone densities, particularly when assessing peri implant bone density changes by subtraction radiography. Their application in implant dentistry will become more widespread.
(E ) Cone beam
Mozzo et al in 1998 reported on the use of the first cone-beam volumetric tomographic (CBVT) machine specifically for dentistry, the New Tom 9000 (Quantitative Radiology, Verona, Italy). The technology allowed for less expensive, smaller, office-based machines that exposed the patient to lower radiation doses,[30],[31] but because of the lower radiation, somewhat less definition of bony images clinically. Since that time, multiple manufacturers have developed and marketed CBVT machines for the dental market. Volumetric imaging (VI) or cone beam CT (CBCT)) creates the opportunity to extend the information yield beyond the conventional imaging methods and is an ideal modality for implant planning. CBCT produces accurate 3 dimensional image data. The field of view is scalable and one scan can include the entire maxillofacial region including the maxilla, mandible, base of skull and TMJs.
Conclusion
Radiographs play an important part in the successful planning and execution of implant treatment. It is important to have an understanding of the different techniques available and their appropriate application. They are an important part of the patients records and as such constitute a significant proportion of the medico-legal documentation of the patient. It is the responsibility of the clinician to ensure that radiographs are appropriate, readable and are retained and repeated at accepted intervals throughout treatment and follow-up. Dental implant therapy requires an accurate preoperative assessment of the patient’s hard and soft tissues. Clinicians should understand the indications, applications, and limitations of different imaging techniques in order to obtain maximum information while keeping radiographic risks to a minimum.
References
1. Gröndahl HG. Radiographic examination. In: Lindhe J, Karring T, Lang NP, editors. Clinical periodontology and implant dentistry. Copenhagen: Munksgaard, 1997:873-889.
2. Jacobs R, van Steenberghe D. Imaging procedures for pre-operative assessment. In:Jacobs R, van Steenberghe D, editors. Radiographic Planning and Assessment of Endosseous Oral Implants. Berlin: Springer-Verlag, 1998b:7-30.
3. Kircos LT, Misch CE. Diagnostic imaging and techniques. In: Misch CE, editor. Contemporary implant dentistry. St. Louis: Mosby, 1999:73-87.
4. Tronje G, Welander U, McDavid WD, Morris CR. Image distortion in rotational panoramic radiography. VI. Distortion effects in sliding systems. Acta Radiol Diagn(Stockh) 1982;23:153-60.
5. Tyndall AA, Brooks SL. Selection criteria for dental implant site imaging: a position paper of the American Academy of Oral and Maxillofacial radiology. Oral Surg Oral Med Oral Pathol Oral Radiol Endod 2000;89:630-7.
6. Lekholm U. The surgical site. In: Lindhe J, Karring T, Lang NP, editors. Clinical periodontology and implant dentistry. Copenhagen: Munksgaard, 1997:890-905.
7. Palmer RM, Smith BJ, Howe LC, Palmer PJ. Treatment planning: general considerations. In: Palmer RM, Smith BJ, Howe LC, Palmer PJ, editors. Implants in clinical dentistry.London: Martin Dunitz Ltd, 2002:27-34.
8. Lindh C, Petersson A, Rohlin M. Assessment of the trabecular pattern before endosseous implant treatment: diagnostic outcome of periapical radiography in the mandible. Oral Surg Oral Med Oral Pathol Oral Radiol Endod 1996;82:335-43.
9. Klinge B, Petersson A, Maly P. Location of the mandibular canal: comparison of macroscopic findings, conventional radiography, and computed tomography. Int J Oral Maxillofac Implants 1989;4:327-32.
10. Sonick M, Abrahams J, Faiella RA. A comparison of the accuracy of periapical, panoramic, and computerized tomographic radiographs in locating the mandibular canal. Int J Oral Maxillofac Implants 1994;9:455-60.
11. Babbush CA. Evaluation and selection of the endosteal implant patient. In: McKinney RV, editor. Endosteal dental implants. St Louis: Mosby Year Book, 1991:63-74.
12. Strid K-G. Radiographic procedures. In: Brånemark P-I, Zarb GA, Albrektsson T, editors. Tissue-integrated prostheses. Osseointegration in clinical dentistry. Chicago: Quintessence, 1985:317-327.
13. Wenzel A, Sewerin I. Sources of noise in digital subtraction radiography. Oral Surg Oral Med Oral Pathol 1991;71:503-8.
14. Wenzel A. Matters to consider when implementing direct digital radiography in the dental office. Int J Comput Dent 1999; 2:269-90.
15. Hounsfield GN. Computerized transverse axial scanning (tomography). 1. Description of system. Br J Radiol 1973;46:1016-22.
16. Quirynen M, Lamoral Y, Dekeyser C, Peene P, van Steenberghe D, Bonte J et al. CT scan standard reconstruction technique for reliable jaw bone volume determination. Int J Oral Maxillofac Implants 1990;5:384-9.
17. Rothman SL, Chaftez N, Rhodes ML, Schwarz MS. CT in the preoperative assessment of the mandible and maxilla for endosseous implant surgery. Work in progress. Radiology 1988;168:171-5.
18. Schwarz MS, Rothman SL, Chafetz N, Rhodes M. Computed tomography in dental implantation surgery. Dent Clin North Am 1989;33:555-97.
19. Lauterbur PC. Image formation by induced local interactions: examples employing nuclear magnetic resonance. Nature 1973;242:190-1.
20. Zabalegui J, Gil JA, Zabalegui B. Magnetic resonance imaging as an adjunctive diagnostic aid in patient selection for endosseous implants: preliminary study. Int J Oral Maxillofac Implants 1990;5:283-7.
21. Devge C, Tjellström A, Nellström H. Magnetic resonance imaging in patients with dental implants: a clinical report. Int J Oral Maxillofac Implants 1997;12:354-9.
22. Shellock FG. MR imaging of metallic implants and materials: a compilation of the literature. AJR Am J Roentgenol 1988;151:811-4.
23. Gray CF, Redpath TW, Smith FW. Pre-surgical dental implant assessment by magnetic resonance imaging. J Oral Implantol 1996;22:147-53.
24. Gray CF, Redpath TW, Smith FW. Magnetic resonance imaging: a useful tool for evaluation of bone prior to implant surgery. Br Dent J 1998;184:603-7.
25. Nasel CJ, Pretterklieber M, Gahleitner A, Czerny C, Breitenseher M, Imhof H. Osteometry of the mandible performed using dental MR imaging. AJNR Am J Neuroradiol 1999;20:1221-7.
26. Web history—About CSI. Available at: http://sites.google.com/ site/simplantisrael/simplantsources. Accessed May 4, 2010
27. Tammisalo E, Hallikainen D, Kanerva H, Tammisalo T. Comprehensive oral X-ray diagnosis: Scanora multimodal radiography. A preliminary description. Dentomaxillofac Radiol 1992;21:9-15.
28. Ekestubbe A, Thilander A, Gröndahl K, Gröndahl HG. Absorbed doses from computed tomography for dental implant surgery: comparison with conventional tomography. Dentomaxillofac Radiol 1993;22:13-7.
29. Mah J, Hatcher D: Three dimensional craniofacial imaging. Am J Orthod Dentofac Orthop 126:308, 2004
30. Hashimoto K, Yoshinori A, Kazui I, et al: A comparison of a new, limited cone beam computed tomography machine for dental use with a multi-detector row helical CT machine. Oral Surg Oral Med Oral Path Oral Radiol Endod 95:371, 2005
31. Sukovic P: Cone beam computed tomography in craniofacial imaging. Orthod Craniofac Res 6:31, 2003 (suppl 1)
|