Introduction
A variety of names have been given to a form of periodontal disease characterized by deep pockets and advanced alveolar bone loss in young, adolescents and young adults without any systemic disease. Many forms of classification have been devised in attempting to provide the clinician with some rationale for making a differential diagnosis, and arriving at a reasonable prediction of how the tissues respond to treatment.
The first of these was by the 1st World Workshop in Clinical Periodontics in 1989 (The American Academy of Periodontology, 1989). They separated periodontitis into three categories of chronic periodontitis, rapidly progressive periodontitis and refractory periodontitis on the basis of rate of progression and response to therapy. It also included separate entities of early onset disease separating them into localized and generalized juvenile periodontitis and prepubertal periodontitis[1].
Generalized early-onset periodontitis has previously been designated rapidly progressive periodontitis, generalized juvenile periodontitis, and post-juvenile periodontitis. A review of the microbiology literature is complicated because of the many different criteria that have been used to define this disease entity in the past, and very often patients with this form of periodontitis have been included as part of an adult periodontitis group[2].
Postjuvenile periodontitis is seen in patients of 20 or more years of age having overlapping clinical presentations of both localized aggressive and chronic periodontitis. It remains conspicuous in terms of clinical presentation and response to therapy.[3]
Case Report
A 22-year male patient, reported to the Department of Periodontics, Shree Bankey Bihari Dental College & Research Centre, Ghaziabad with the complaint of generalized mobility of teeth since 8 months. The history of present illness revealed that the mobility was progressively noted over a period of 6 months by the patient. There was exfoliation of 26 and 35 earlier due to compromised periodontal support.
Extra-oral examination proved uneventful. The intra-oral examination revealed grade II mobility of 11, 16, 31,34 and grade III mobility in 36. Large amounts of calculus and plaque deposits were present. The gingiva was bluish red, soft and edematous with evidence of bleeding and exudation. There were generalized pockets measuring more than 7 mm and attachment loss was also present. (Fig 1) Radiographic features revealed vertical bone loss (Fig 2). Hematological investigations were done which were within the normal limits. Based on the clinical findings and radiographical investigations, a diagnosis of post-juvenile periodontitis was made.
 | Fig 1 : Pre-operative Photographs With Pocket Depth.
 |
 | Fig 2 : Pre-operative Radiograph.
 |
Treatment
After diagnosis, treatment was started with the extraction of 36 followed by initial phase of mechanical therapy. The mechanical therapy included systematic scaling and root planning and the introduction of meticulous oral hygiene (brushing twice a day, chlorhexidine gluconate mouth rinse 0.2%{10ml} twice a day). Systemic antibiotics in the form of doxycycline 100 mg bid the first day, then 100 mg qid for 14 days was prescribed. The mobile teeth were splinted using restorative composite resin reinforced with splinting-ribbon (Ribbond) (Fig 3). Selective grinding of the occlusion and incisal edge was done to avoid premature contacts. Clinical reassessment after a period of 4 weeks revealed marked reduction in pocket depth (Fig 4). Radiographic assessment after a period of 6 months revealed significant regeneration of bone (Fig 5).
 | Fig 3 : Splinting With Ribbond.
 |
 | Fig 4 : Post-operative Pocket Depth.
 |
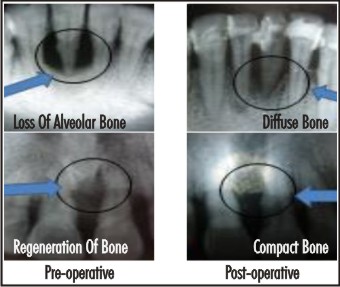 | Fig 5 : Comparison Of Pre-And Post Operative Results After 6-months.
 |
Discussion
In the course of periodontal pathology, many factors enter the equation to produce a variety of tissue changes and therefore, different clinical features. Based on the etio-pathogenesis, many forms of classification systems have been revised, though the line of treatment remains almost the same.
Although the new classification of periodontal diseases has tried to remove the confusion with regard to some terms, a clinical dilemma still appears in the diagnosis of a case where clinical features of two diseases overlap. In the present case, treatment was not a problem but dilemma existed in placing the clinical entity in the present classification system.
Chronic periodontitis has been defined as “an infectious disease resulting in inflammation within the supporting tissues of the teeth, progressive attachment loss, and bone loss”.[4] The characteristics of chronic periodontitis are that it is prevalent in adults but can occur in children. The amount of destruction is consistent with local factors. There is slow to moderate rate of progression with possible periods of rapid progression.
Aggressive periodontitis is a distinct bacterial disease from adult chronic periodontitis which occurs in otherwise clinically healthy patient. There is rapid attachment loss and bone destruction. The amount of microbial deposits is inconsistent with disease severity. There is familial aggregation of diseased individuals. The localized form have circumpubertal onset of disease and affects first molar or incisor teeth with proximal attachment loss on at least two permanent teeth, one of which is a first molar. The generalized form affects persons under 30 years of age (however, may be older) and there is generalized proximal attachment loss affecting at least three teeth other than first molars and incisors.
The hallmark of the early onset periodontitis is the clinical presentation of the disease early in the life coupled with the high virulence of the organism and elevated host susceptibility.
The criteria for the diagnosis of generalized early-onset periodontitis or post-juvenile periodontitis given by (Bare 1971)[5] are:
1. Attachment loss of 4mm or more affecting at least eight teeth.
2. Distribution- At least 3 affected teeth other than molars and incisors.
3. Age of onset- Before 35 years of age.
4. Advanced attachment loss frequently leading to premature tooth exfoliation.
5. Affecting most of the dentition (both primary and permanent).
6. Inflammation of both marginal and attached gingiva.
Conclusion
The problem of classification of periodontal diseases is extremely difficult and complex. The new classification of periodontal diseases has on the whole removed the dilemma with regard to some terms and has thus facilitated application in practice. As previously remarked neither of these classification are ideal[6].
Postjuvenile periodontitis, the heterogenous group includes the most severe form of periodontitis, remains conspicuous in terms of clinical presentation and response to therapy. Successful treatment of the postjuvenile periodontitis is considered to depend upon early early diagnosis, directing therapy towards maximal suppression of the infecting microorganisms and providing an environment conducive to long term maintenance[7].
References
1. Denis F. Kinane; Periodontology 2000, Vol. 26, 2001, 7–15J.A.
2. Ivan Darby & Michael Curtis: Periodontology 2000, Vol. 26, 2001, 33–53.
3. B.M. Eley and J.D. Manson; Periodontics; 5th edition.Wright, Elsevier limited.
4. Newman, Takei, Klokkevold, Carranza; Carranza’s Clinical Periodontology,10th edition.Saunders, Elsevier.
5. Bare p. The case of periodontitis as a clinical entity, Periodontal 1971,42:516-520.
6. Darije PlanEak, Ksenija Jorgie-Srdjak, Zvonimir Curilovie, New Classification of Periodontal Diseases; Acta Stomat Croat 2001; 89-93.
7. Rajesh R, Prabhu V. R. Generalized early onset periodontitis: A case report; J Ind Soc. Of Pedo Pre Dent ; June 2000.
|