Introduction
The first feature of the face to be noticed is eyes. It is an organ of vision but also an important component of facial expressions. Loss of an eye has a psychological effect on the patient. So prosthesis should be provided as soon as possible for psychological well being of the patient [1].
An ocular prosthesis is a simulation of human anatomy using prosthetic materials to create the illusion of a perfectly normal healthy eye and surrounding tissues. Ocular prosthesis artificially replaces an eye missing as a result of trauma, surgery or congenital absence. The Prosthesis does not replace missing eyelids, adjacent skin, mucosa or muscle. There are basically 2 types of prosthesis (i) Readymade (stock eye) ocular prosthesis and (ii) Custom- made. The various surgical procedures for the removal of eye are Evisceration, Enucleation and Exenteration as classified by Peyman, Saunders and Goldberg (1987) [2],[3].
Evisceration is the removal of the content of the eyeball leaving the sclera and sometimes the cornea intact also preserving the extraocular muscle attachments. This procedure is indicated in case of blind and painful eye, corneal perforation and endophthalmitis. In this extraocular muscles are left intact therefore good mobility of the prosthesis is usually possible.
Use of an artificial eye dates back to the period of the Egyptians in 1613 BC. They used silver eyes for mummies. Ambroise pare (1510-1590) a French man was the first to describe the use of artificial eye made of gold and silver (“emblepharon”) to fit an eye socket[4]. He also used glass and porcelain for eyes, which was a great step forward and resulted in the use of the shell type of pattern rather than spheres [5]. But it was Ludwig Mueller- Uri (1830) a German glass bowler who was credited with the development of fine quality glass eyes. In those days, Germany was the main producer of glass eyes. During the World War II the supply of glass eyes from Germany to USA was halted. It was then that the Naval Dental School (USA) in 1943 tested the use of acrylic resin in fabricating ocular prosthesis [6].
This case report describes the rehabilitation of a patient with a sclera prosthesis following evisceration of the eye to rehabilitate an operated case of trauma to an eye.
Case Report
A 28 year old male patient reported to the department of prosthodontics with the chief complaint of unesthetic appearance of right eye following surgery. Patient gives history of trauma with wooden block during his childhood for which he was operated. He lost his vision in right eye, after surgery there was discolored and shrunken right eye. Patient was referred by an ophthalmologist for the fabrication of sclera prosthesis (Fig 1).
 | Fig - 1
 |
Technique
(a)The impression procedure
Stock tray technique- Perforated stock tray (conformer) is used to make an impression. Alginate is loaded in a 10 ml disposable syringe. Impression material was expressed into the defect when the patient gazes directly forward. Once material sets, tray was removed from shallower sulcus first and rotated out of deeper upper sulcus (Fig 2).
 | Fig - 2
 |
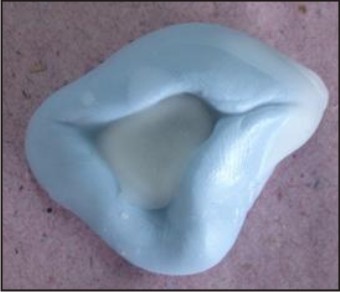
(b)Wax pattern fabrication and positioning of the iris
Putty material was adapted around the impression to form a mold. Molten tooth colored carving wax flowed into putty mold (Fig 3). Smoothed and polished wax pattern was tried into patient’s eye. Eye contours are checked. Lines are marked on the face and the position of middle of the pupil is marked while the patient gazes directly straight at the clinician (Fig 4). Natural eye is observed closely and the diameter of the iris is estimated using a mm measurement gauge. To determine the position of iris/cornea black color acrylic stalk, ocular disc or corneal buttons are used (Fig 5).
 | Fig - 3
 |
 | Fig - 4
 |
 | Fig - 5
 |
(c) Wax pattern try in
The wax pattern was tried in the patient’s ocular defect for comfort, stability, a proper orientation, mobility and for iris and sclera contours. The position, gaze and aesthetics of the prosthesis were shown to the patient and it got approved.
(d) Flasking and curing
When the wax pattern is determined to be appropriate, it is flasked and processed in crown flask with tooth colored methylmethacrylate resin (Fig 6). The color of resin should match the color of sclera of patient’s eye. The sclera prosthesis was then finished and polished using pumice and acrylic resin polishing cake.
 | Fig - 6
 |
(e) Positioning the iris, finishing and polishing of prosthesis
By using a flat end bur, a flat surface is prepared in the corneal area where black color corneal button was present. Digital photographs of patient’s natural iris were clicked using a digital camera. Slight adjustment of color, brightness, contrast and intensity were made using graphic software. (Adobe Photoshop). Final images were printed on white paper with differing brightness, contrast using a laser printer with a color ink cartridge. Multiple prints were compared with the patient’s natural iris for perfect color match and best print among them was selected and pasted over the flat surface which was created over corneal button. Remainder of the prosthesis was then painted to match sclera of the natural eye. Fine red embroidery threads were placed on the sclera to mimic the blood vessels of the natural eye (Fig 7). The entire sclera prosthesis was then coated with cold cure transparent monomer and polymer to keep blood vessel fibers in place and allowed to set. Final sclera prosthesis was trimmed, finished and polished. At the time of insertion aesthetics, fit and the movement of the prosthesis were assessed (Fig 8).
 | Fig - 7
 |
 | Fig - 8
 |
(f) Delivery of prosthesis
Prosthetic eye was washed with soap and water. A drop of an ophthalmic lubricant on the surface of the prosthesis facilitates insertion. The patient was educated on a thorough maintenance protocol. Review of the patient was done at 1 wk, 3 weeks and 1 month intervals to assess tissue response to new prosthesis. Only mild soap or detergent should be used with warm water for cleaning. During recall visits the fit, mobility and direction of gaze of the prosthesis should be first checked. Then it should be removed and checked for scratches, chips and bacterial growths etc. If prosthesis neither too old, nor chipped, then careful repolishing can be done to remove scratches due to dirt and dust.
Discussion
A correctly placed prosthesis should restore the normal opening of the eye, support the eyelids, restore a degree of movement, and be adequately retained and esthetically pleasing. Several techniques have been used for fabricating artificial eyes like (1) Use of a stock ocular prosthesis of an appropriate size and color, which is adapted by selective grinding or addition of acrylic resin. This has been advocated by Laney and Gardner [7]. Another technique involves the use of a viscoelastic tissue conditioner material as an impression material to modify a stock ocular prosthesis in relation to an anophthalmic socket [8]. But the tissue conditioner may cause irritation to the conjunctivae if the ethyl alcohol in the liquid is not thoroughly incorporated into the Polyethyl Methacrylate powder. And if mixed in thick consistency and added excessively to the prosthesis, it may produce a protruded or exophthalmic ocular prosthesis [8]. However because of extreme individual variation and diverse nature of ocular injuries, certain patient’s would benefit more from custom–made ocular prosthesis. In custom-made prosthesis, intimate contact is achieved between the prosthesis and tissue bed. Also pressure is distributed more equally thereby helps in reducing the incidence of the conjunctival abrasion and ulceration. It enhances tissue health by reducing potential fluid stagnation spaces at the prosthetic-tissue interface [8]. It provides better aesthetic results because the iris and the sclera are custom fabricated and painted.
Till date various materials like gold, silver, glass, acrylic and even porcelain have been used for making artificial eyes, but the preferred material is acrylic [9]. Acrylic is light weight, easy to fit and adjust, translucent, easily fabricated, has intrinsic and extrinsic coloring capabilities, and is inert to the socket secretions [10].
Several techniques for fabricating the iris of custom acrylic resin prosthesis exist. 1 technique is the conventional oil paint and Iris –painting technique. But this technique requires tremendous artistic skills and is time consuming. In another technique digital photography of the patient’s iris is used in the fabrication of the iris for an ocular prosthesis [11].
The digital image provides the acceptable esthetic results because it closely replicates the patient’s iris with minimal color adjustments and modifications. But it requires special digital photography equipment, settings and the computer software that allows for Image adjustments. However we have fabricated custom ocular prosthesis utilizing digital photography. This technique is simple, decreases treatment time and requires minimal artistic skills. The prosthesis produced by this method is esthetically good, comfortable, promote physical and psychological healing of the patient and thus improves social acceptance.
Conclusion
Most vital concern of a patient needing an ocular prosthesis is long lasting esthetics and comfort. The esthetic outcome of the custom made prosthesis was far better than the stock ocular prosthesis. The procedure used here is simple and cost effective. The patient cannot see by this prosthesis, but this prosthesis will help in increasing the self confidence of the patient to face the world.
References
1. T Taylor. Clinical maxillofacial prosthetics, Quintessence Chicago III USA 2000.
2. Marunick MT, Harrison R, Beumer J. Prosthodontic rehabilitation of midfacial defects. J Prosthet Dent.1985; 54: 553-560.
3. Su GW, Yen MT. Current trends in managing the anophthalmic socket after primary enucleation and evisceration. Ophthalmic plastic and reconstructive surgery. 2004; 20: 274.
4. Roberts AC. Ocular prosthesis. In facial prosthesis. Ist ed. London Henry Kimpton, 1971: p 4.
5. Murphy PI, Schlossberg L. Eye replacement by acrylic maxillofacial prosthesis. Naval Med Bull 1944; 43: 1085.
6. Skyes LM. Custom made ocular prosthesis: a clinical report. J Prosthet Dent 1996; 75: 1-4.
7. Laney WR, Gardner AF. In Maxillofacial Prosthesis 2nd ed. Littleton PSG Publishing 1979;p 255-258.
8. Ow RK, Amrith S. Ocular prosthesis: use of a tissue conditioner material to modify a stock ocular prosthesis. J Prosthet Dent. 1997; 78: 218-222.
9. Ishigami T, Tanaka Y, Kishimoto Y, Okada M. A facial prosthesis made of porcelain fused to metal: a clinical report. J Prosthet Dent. 1997; 77: 564-567.
10. Dyer NA. The artificial eye. Aust J Ophthalmol. 1980; 8: 325-327.
11. Artopoulou II, Montgomery PC, Wesley PJ, Lemon JC. Digital imaging in the fabrication of ocular prosthesis. J Prosthet Dent.2006; 95: 327-330.
|