Introduction
Literature is replete with instances of the replacement of lost soft tissue structure owing to either traumatic extractions, trauma, alveolar ridge resorption or periodontal disease, employing various mucogingival surgical techniques[1]. Foreseeable outcomes have been accomplished by numerous authors[2],[3] for isolated gingival recession defects. Multiple gingival recessions with open interdental spaces however are the frequent consequences that have been of esthetic concern since decades for which a predictable regenerative solution is still not available. Additionally, altered labiodental / linguoalveolar consonant production[4] may also hamper normal speech thus being a social embarrassment for the patient. With the growing emphasis on esthetics and the patients vying for a perfect smile, the periodontists have steered their attention towards prosthetic replacement options. The challenge however lies in the patients with excess maxillary display to create a proportional prosthetic replacement that phonetically seals these patient’s interdental areas yet maintaining the patient’s oral hygiene.
Prosthetically these appliances might be of either removable or fixed variety capable of replacing large volumes of tissue. Fabrication materials may vary from pink autocure and heat-cured acrylics, porcelains, composite resins and thermoplastic acrylics, silicone-based soft materials to flexible nylon based thermoplastic material[5],[6]. Engineering of the appliance is initiated two to three months subsequent to the initial periodontal therapy to provide the window period for the restitution of the tissue contours.
Traditionally these have been employed to mask the exposed root surfaces, prevent impaction, improves speech and phonetics and esthetics of the patient[7]. Antony and Khan[8] have also discussed them as an interim measure to improve the esthetics of anterior crowns after initial periodontal therapy to allow time for healing and the establishment of periodontal stability and prognosis. Severe alveolar deficiencies may also be corrected utilizing implant supported prosthesis[9].
The following case report describes the fabrication of an esthetic soft flexible nylon based thermoplastic gingival veneer in a chronic periodontitis patient following surgical periodontal therapy thereby providing an economical and esthetically acceptable solution.
Case Report
A 39 year old male patient who had undergone previous orthodontic treatment 3 years ago and had splinted maxillary and mandibular anterior teeth reported to our periodontal office with a major concern of weak periodontal tissues and esthetic embarrassment due to gingival recession. On periodontal examination, the patient was found to have moderately deep periodontal pockets with generalized Miller’s Class III gingival recession. On smiling the patient exhibited a high lip line rendering the open interdental spaces and the exposed root surfaces visible thereby making it a cause of social embarrassment for him. The patient desired a remedy for the same.
 | Fig. 1 : Preoperative View Showing High Smile Line With Open Interdental Spaces And Exposed Root Surfaces
 |
 | Fig. 2 : Miller’s Class III Gingival Recession
 |
As the patient suffered from Miller’s Class III gingival recession situation, he was explained the inability of regenerative periodontal therapy to completely fill up the gross tissue deficits in open interdental spaces and rectify the situation to previously normal levels. The treatment plan encompassed initial scaling and root planing followed by periodontal flap surgical procedure along with bone grafting and GTR membrane in the indicated areas. Upon achievement of satisfactory gingival health and oral hygiene maintenance by the patient, on reevaluation after a healing period of three months, the fabrication of a prosthetic “artificial gingival mask” was initiated.
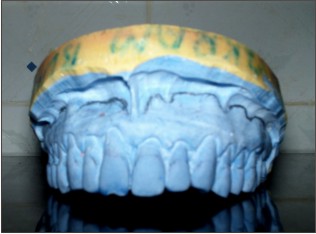 | Fig. 3 : Maxillary Cast With Blocked Out Lingual Embrasures And Outline For The Gingival Mask Fabrication
 |
 | Fig. 4 : Gingival Mask On The Cast
 |
The lingual embrasures were blocked with utility wax to prevent the distortion of the impression on removal. The buccal embrasures were left open to facilitate mechanical retention of the appliance. An elastomeric impression material was used to make the final impression to allow recording of the depth of the vestibule. Subsequent to elastic recovery, the cast was poured in dental stone. The extension of the prosthesis was outlined on the cast from the depth of the vestibule to the cementoenamel junction and a wax up was done incorporating the surface characterization mimicking healthy gingiva. The wax up was then sent to the laboratory for fabrication of a soft, flexible nylon based thermoplastic gingival veneer.
Following insertion the patient was instructed regarding the usage and maintenance of the appliance. The patient was recalled on a weekly basis for the first month to evaluate the gingival health and oral hygiene maintenance.
 | Fig. 5 : Gingival Mask Placed Intraorally
 |
 | Fig. 6 : Improved Smile With Gingival Mask In Position
 |
Discussion
Excessive gingival deficiencies consequent to periodontal disease creates unsightly open interdental spaces with increased incidences of food impaction, hampered phonetics as well as unacceptable esthetics for the patient. Advanced bone and soft tissue loss in such cases are not amenable to the most aggressive measures towards periodontal regeneration. Periodontists often face these challenging demands of providing the patients with an esthetic smile while ensuring impeccable oral hygiene maintenance. Prosthetic replacements offer the advantage of an aesthetically pleasing, functional restoration that mimics the anatomic tissue contours. Moreover, the patient can visualize a completely waxed up prosthesis prior to the final fabrication thus augmenting the predictability of the procedure further.
Apart from the above mentioned, a multitude of other clinical situations warrant the formulation of gingival veneers; also referred to as the Gingival mask, Flange prosthesis, Gingival veneer prosthesis and Artificial gingiva; viz.[10],
To cover- exposed crown margins, exposed implant components and root surfaces and reduce the length of the clinical crown.
To fill in the space between the crown and the soft tissue.
To prevent airflow through or beneath maxillary fixed restorations or through the spaces between the teeth and thus improving phonetics.
To provide increased lip and cheek support for those patients who require it.
It is also beneficial for patients with high lip lines and a gummy smile who have been treated with osseo integrated dental implants.
To hide the dark lines around old crowns that are often seen with patients who have experienced gingival recession.
It also aids the prosthodontist to design implant supported prosthesis with optimal configurations permitting easy access for oral hygiene maintenance.
Used in the management of acute gingival conditions like desqua mative gingivitis[11].
Patients exhibiting poor plaque control, unstable periodontal health and high caries activity however are absolutely contraindicated to receive such therapy. Furthermore, acrylic veneers are often associated with discomfort owing to their rigidity and pain while insertion and removal[12],[13]. Discoloration due to frequent consumption of tea or coffee is yet another corollary which the patient has to deal with thus necessitating either the reduction of intake or recurrent replacement of the appliance[14],[15].
Keeping in view the patient’s expectations and the clinical picture available, either a fixed or a removable variety of the prosthesis should be selected. While on one hand the fixed options offer the advantage of being stable thus contributing to the psychological stability of the patient, stains less and gets cleaned easily due to the highly polished porcelain surface, yet they are most unsuitable when gross alveolar ridge deficiencies exist. Besides, inaccessible interproximal surfaces and embrasure areas might complicate oral hygiene maintenance. Removable prosthesis on the other hand due to their mobility during function might confer an unnatural feel and discomfort to the patient, are amenable to ingestion or loss and readily stain from food pigments[16]. Nevertheless, they are the replacements of choice when large volumes of the tissue need to be created for aesthetic appearance and the prosthesis can be adjusted as the tissue changes. Advent of nylon based thermoplastic veneers has revolutionarized this field by offering the chief advantage of superior aesthetics and complete tissue comfort with a feeling of "own tissue" [17]. In this case report too, we have employed these soft nylon veneers to bridge the soft tissue deficits resulting in a satisfied patient with an aesthetically pleasing and confident smile.
Conclusion
In cases of gross periodontal tissue loss, patients often face esthetic, functional and consequent psychological problems. Removable gingival prosthesis provides a satisfactory option addressing all the tribulations efficiently and warranting a multidisciplinary approach in routine clinical practice to provide the patients with a holistic treatment approach.
Conflict Of Interest
There was no financial support in the form of grants, equipments, drugs or any other significant sources of support for the present study. Also there was no financial relationship between the authors and any commercial firm.
References
1. Bertoldi C, Zaffe D, Consolo U. Polylactide/polyglycolide in the bone defect healing in humans. Biomaterials. 2008 Apr;29(12):1817-23.
2. Meyer MJ, Wikesjo UME. Gingival recession defects and guided tissue regeneration: A review. J Periodont Res 2001; 36: 341-54.
3. Kimble KM, Eber RM, Soehren S, Shyr Yu, Wang HL. Treatment of gingival recession using a collagen membrane with or without the use of demineralized freeze-dried bone allograft for space maintenance. J Periodontol 2004; 75: 210-20.
4. Mekayarajjnanoth T, Kiat-amnuay S, Sooksuntisakoonchai, N, Salinas TJ. The functional and esthetic deficit replaced with an acrylic resin gingival veneer. Quintessence Int 2002;33:91-4.
5. Barziley I, Tamblin I. Gingival Prosthesis- A Review. Can Dent Assoc 2003; 69(2):74–8.
6. Hannon SM, Colvin CJ, Zurek DJ. Selective use of gingival-toned ceramics:Case reports. Quintessence Int 1994;25:233-8.
7. Mericskestern R, Zarb GA. Overdentures: an alternative implant methodology for edentulous patients Int J prosthodont 1993; 6: 203-208.
8. Antony VV, Khan R. Gingival Mask- Restoring the lost smile. JDMS 2013;5(3):20-2.
9. Parel SM, Balshi TJ, Sullivan DY, Cardenas ER, Gingival augmentation for osseointegrated implant prostheses, J Prosthet Dent 1986;56;208-211.
10. Green PR. The flexible gingival mask; an aesthetic solution in periodontal practice. Br Dent J 1998. 184; 11: 536-540.
11. Materdomini D. and Friedman MJ.: The contact lens effect: Enhancing porcelain veneer esthetics. Journal of Esthetic Dent. 1995; 7(3): 99-103.
12. Brygider RM. Precision attachment-retained gingival veneers for fixed implant prosthesis J Prosthet Dent 1991; 65: 118-22.
13. Gunay H, Blunck U. Flexible gingival augmentation for implant supported denture. Quintessenz 1990; 4: 227-34 German.
14. Iselin W, Merer C, Lufi A, Lutz F. The flexible gingival epithesis: the practical procedure, laboratory technics and clinical experience Schweiz Monatsschr Zahnmed 1990; 100: 966-79.
15. Kapari D, Tsalikes Lehmann KM, Flores de Jacoby L. Changes in the physical properties of gingivamoll flexible epithesis. Dtsch Nahnarz HZ 1991; 46: 503-5.
16. Ellis SGS., Sharma P. and Harris IR.: Case report: Aesthetic management of localized periodontal defect with a gingival veneer prosthesis. Eur J Prosthodont Rest Dent. 2000; 8(1): 23-26.
17. Hummert TW, Kaiser DA. Block out technique for impression of teeth with increased open gingival embrasures. J Prosthet Dent 1999;82:100-2. 5.
|