Introduction
Extraction sockets generally heal with bone tissue after 1 to 2 months, and this healing process usually occurs with substantial reduction of the original height and width of the alveolar bone. Ridge defects often hamper the placement of ideally shaped artificial crowns and are basically treated with soft or hard tissue grafts. Resorption of the residual alveolar ridge is an inadvertant process after extraction. Chen[1] and Schropp[2] have reported an average 0.34 to 7.7 mm horizontal and 0.2 to 3.25 mm vertical bone loss 6 month after extraction. To reduce these difficulties ridge bone maintenance procedures using biomaterials were utilized to preserve the ridge anatomy and increase the possibility of rehabilitation after tooth extraction. Various materials have been used to prevent or minimize ridge collapse after tooth extraction in an attempt to improve implant placement.
Acellular dermal matrix (ADM) is a processed allogenic material obtained from human skin, and is processed in such a way that the epidermal layer and all cells in the dermis are removed.(ref)In this case report, an extraction socket was grafted with ADM as GBR (guided bone regeneration membrane) and corticocancellous bone graft. Bone healing was evaluated by harvesting a bone sample at the time of implant placement.
Case Description
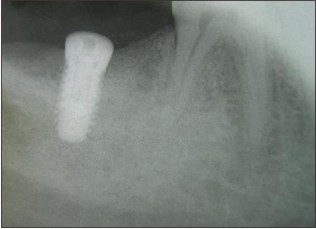
A 54 year old male presented with pain in lower right region of the mouth. Intraoral examination showed 47 sensitive to percussion with deep buccal pocket (7 mm) with furvcation involvement. Radiographic evaluation revealed a fractured 46 with poor prognosis (Fig 1-3) Treatment planned for the case included : extraction of the tooth, socket augmentation, a delayed placement of the implant retained prosthesis.
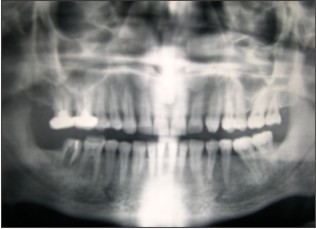 | Fig 1 : Perio-Endo Lesion In Relation To 47
 |
 | Fig 2 : Poor Prognosis 47
 |
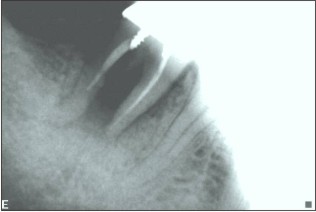
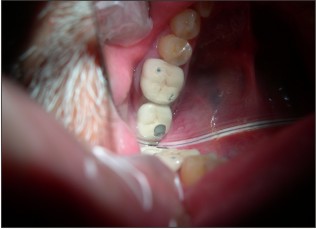
 | Fig 3 : Extraction Socket
 |
Treatment Planning
Radiographic interpretation of the case presented perio-endo lesion in relation to 47 with a poor prognosis. On removal of the crown there was a midline vertical fracture in the tooth. Treatment planned was : Guided bone socket augmentation to be followed with implant supported prosthesis.
Surgical Stage
After administering local anaesthesia, failing 47 was extracted. Thorough debridement of the socket was done to remove the diseased granulation tissue. (Fig 4) A wide buccal dehiscence was present (6 mm long and 4mm wide, as measeured with the William’s periodontal probe) Horizontal bone width was meassured with bone caliper after tooth extraction with reference to the centerpoint of the buccal defect as 5.7 mm. Socket walls were decorticated to infuse the fresh bleeding. Corticocancellous graft Mineross (Biohorizon , AL) was filled into the extraction socket to the crestal confines of the socket. (Fig 5) Alloderm GBR (Biohorizon, AL ) was tacked over the socket bucally and lingually. Soft tissue was coronally advanced and 5-0 nylon Ethicon (Johnson and Johnson ) sutures were placed in. (Fig 6) Augmentin (Glaxosmithline)was prescribed as 675 mg for 5 days. After 12 days the sutures were removed. Radiographic evaluation at 9 months presented as well condensed bone (Fig 7) and a thick keratinized soft tissue . (Fig 8) Ridge mapping revealed a midbuccal horizontal width and the soft tissue thickness as 6.1mm and 2.3mm respectively. Trephine bone core biopsy was done for histologic examination. Bio-horizon (4.2 x 10mm) implant was placed in. (Fig 10) Histological examination under (H&E x400) magnification revealed active bone formation in the areas adjacent to the graft material. (Fig 9).
 | Fig 4 : Minerosss Grafted Into The Extraction Socket
 |
 | Fig 5 Alloderm Tacked And Suturing Done
 |
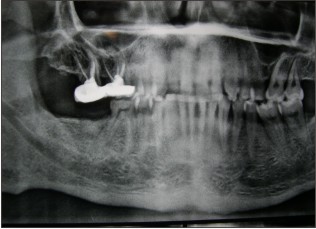 | Fig 6 : 9 Months Post Ridge Augmentation
 |
 | Fig 7 : Thick Keratinized Mucosa Overlying The Augmented Site
 |
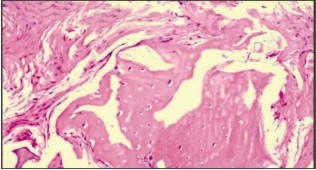 | Fig 8 : Active Bone Formation Adjacent To The Resorbing Graft Particles (H&e X400)
 |
 | Fig 9 : Biohorizon (4.2x10mm) Implant In Place
 |
 | Fig 10 : Healing Abutment In Place
 |
Prosthetic Stage
At 4 months cover screw was removed and a 2mm healing abutment was placed- in. (Fig 11) 2 weeks later, impression was recorded for PFM prosthesis (Fig 12). Owing to the reduced interocclual space, a screw retained prosthesis was seated in. (Fig 13-14) The abutment screw was ratched at 35 Ncm and the access hole was sealed. Patient was put on the maintainence follow up of 6 months interval and was followed upto 2 years with clinical and radiographic evaluation
 | Fig 11 : Preparation For Impression
 |
 | Fig 12 : Metal Frame Work For Screw Retained Prosthesis
 |
 | Fig 13 : Screw Retained Prosthesis In Place
 |
 | Fig 14 : 25 Month Post Restoration
 |
Results
25 months follow up post- restoration revealed a stable prosthesis in function. The soft tissue assessments presented a periimplant sulcus depth of 4mm with a thick keratized mucosa around.
Discussion
Post extraction resorption rate is higher buccally than lingually.[3] The loss of width of the alveolar ridge is always higher than the ridge height.[4],[5],[6],[7] Higher resorption has been reported in the maxilla than mandible.[3] Socket augmentation helps to reduce the localized ridge deformities and help in a successful rehabilitation with endosseous implants[8]. Research has shown that ridge bone maintainence procedures with the use of the biomaterials, helps in decreasing the expected bone loss and increases the success of rehabilitation after tooth extraction.[9],[10] Combination of bone grafts with other materials e.g PRP , GTR membranes, collagen plug etc were introduced to maximize the effect of the bone formation. In this case we evaluate clinically, histologically and radiographically the tissues formed around the implant in a socket presenting buccal bone defect utilizing the guided bone regeneration technique with corticocancellous graft and allograft GBR membrane. The GBR technique resulted in 0.4mm increase of horizontal width and a quantum bone fill around the implant. Appreciable keratinized mucosa resulted after healing. Histological section showed a viable bone formation in the vicinity of the bone graft with absence of any inflammatory cell findings.
Conclusion
The results from this case report reveaal thatt ridge preservation presents a predictable option to prepare the extraction site for future implant supported rehabilitation especially in cases where delayed implants is the opted option
References
1. Chen ST,Wilson TG. Immediate or ealr implant placements following tooth extraction . Review of biologic basis , clnical procedures and outcomes. Int J Oral Maxillofac Implants 2004;19:12-25.
2. Schropp L,Wenzel A,Kostopoulus L.bBone healing and soft tissue contour changes following songle tooth extraction: A radiographaic and clinical 12 month retrospective study.
3. Pietrokovski J,Massler M. Alveolar ridge resorption following tooth extraction.J Prosth Dent1967 ;17:21-27.
4. Lekovic V ,Kenney EB,Weinlander M.A bone regenerative approach to alveolar ridge maintainence following tooth extraction. Report of 10 cases. J Periodontol1997;68:563-570.
5. Lekovic B,Camargo PM,Klokkevold P. Preservation of alveolar boneinextarction socket using bioabsorbable membrane. J Periodontol 1998;69:1044-1049.
6. Johnson K.A study of the dimensional changes occurring in the maxilla following closed face immediate denture treatment. Aust Dent J 1969;14:371-376.
7. Johnson K.A study of dimensional changes occurring on the maxilla following tooth extraction. Aust Dent J 1969;14:241-244.
8. Barboza EP. Localized ridge maintainence using bone membrane Implant Dent 1999;8:167-172.
9. Bartee BK .Extraction site reconstruction for alveolar ridge preservation. Part 1:Rationale and materials selection.J Oral Impalntol2001;27:187-193.
10. Becker W,Hujoel P,Becker BE. Effect of barrier membrane and autologous bone graft on ridge width preservation around implants. Clin Implant Dentist Related Res 2002;4:143-149.
|