Introduction
'Periodontium' is the general term that describes the tissues that surround and support the tooth structure. The periodontal tissues include the gums, the cementum, the periodontal ligament and the alveolar bone. Among several acute conditions that can occur in periodontal tissues, the abscess deserves special attention. Abscesses of the periodontium are localized acute bacterial infections which are confined to the tissues of the periodontium. Abscesses of the periodontium have been classified primarily, based on their anatomical locations in the periodontal tissue. According to Meng et al (1999)[1] abscesses of periodontium are classified as: Gingival, Periodontal & Pericoronal abscess.
Gingival abscess
A gingival abscess is a localized, painful, rapidly expanding lesion involving the marginal gingiva or interdental papilla sometimes in a previously disease-free area.
Periodontal abscess
A periodontal abscess is a localized accumulation of pus within the gingival wall of a periodontal pocket resulting in the destruction of the collagen fibre attachment and the loss of alveolar bone.
Pericoronal abscess
The pericoronal abscess is a localized accumulation of pus within the overlying gingival flap surrounding the crown of an incompletely erupted tooth, usually occurring in the mandibular third molar area.
Classification based on etiological criteria[2]:
1. Periodontitis related abscess: When acute infections originate from a biofilm (in the deepened periodontal pocket)
2. Non-Periodontitis related abscess: When the acute infections originate from another local source. E.g. Foreign body impaction, alteration in root integrity.
Among all the abscesses of the periodontium, the periodontalabscess is the most important one, which often represents the chronic and refractory form of the disease[1].
Predisposing factors:
1. Changes in the composition of the micro-flora, bacterial virulenceor in host defences could also make the pocket lumen inefficient to drain the increased suppuration
2. Tortuous periodontal pockets are especially associated with furcation defects. These can eventually become isolated & can favour the formation of an abscess.
3. Periodontal abscesses can also develop in the absence of periodontitis, due to the following causes:
Impaction of foreign bodies (such as a piece of dental floss, a popcorn kernel, a piece of a toothpick, fishbone, or an unknown object)
Infection of lateral cysts,
Local factors affecting the morphology of the root may predispose to periodontal abscess formation. (The presence of cervical cemental tears has been related to rapid progression of periodontitis and the development of abscesses).
Pathogenesis:
The entry of the bacteria into the soft tissue pocket wall could be the event that initiates the formation of a periodontal abscess. However, accumulation of leukocytes & formation of acute inflammatory infiltrate will be the main cause of the connective tissue destruction, encapsulation of bacterial mass & formation of pus. The inflammatory cells & their extracellular enzymes are the main cause of destruction of connective tissue. Both lowered tissue resistance & virulence & number of bacteria will determine the course of this acute infection.
Features that differentiate the gingival abscess from the periodontal abscess are:
I. History of recent trauma;
ii. Localisation to the gingiva;
iii. No periodontal pocketing
Periapical Abscess
Periapical abscess can be differentiated by the following features:
i. Located over the root apex
ii. Non-vital tooth, heavily restored or large filling
iii. Large caries with pulpal involvement.
iv. History of sensitivity to hot and cold food
v. No signs / symptoms of periodontal diseases.
vi. Periapical radiolucency on intraoral radiographs.
Microbiology:
The culture studies of periodontal abscesses have revealed a high prevalence of the following bacteria:
1. Porphyromonas gingivalis-55-100% (Lewis et al) [3]
2. Prevotellaintermedia- 25-100% (Newman and Sims) [4]
3. Fusobacteriumnucleatum -44-65% (Hafstrom et al) [5]
4. Actinobacillus actinomycetem comitans - 25% (Hafstrom et al) [5]
5. Campylobacter rectus- 80% (Hafstrom et al) [5]
6. Prevotella melaninogenica-22%
Description of Cases:
Case1 - Gingival abscess:
A 32 year old male patient reported to the Department of Periodontics, complaining of pain & swelling in the lower right back region of the jaw since 2-3 days. (Fig. 1) Patient’s history revealed that he had pricked the area with toothpick 3-4 days ago while attempting to remove impacted food. The pain was dull & intermittent in nature. On examination, there was a soft, fluctuant swelling in relation to 47. The swelling was ovoid in shape & was not associated with periodontal pocket.
 | Fig. 1. : Intra-oral preoperative photograph: Right lateral View showing gingival abscess in relation with 47
 |
Intraoral peri-apical radiograph with 47, 48 did not reveal any alteration in bone levels or periapical changes. (Fig. 2) Considering the history, symptoms and clinical & radiographic findings, the lesion was provisionally diagnosed to be a gingival abscess.
 | Fig. 2. : Preoperative Radiographic view: Intraoral peri-apical radiograph did not reveal any alteration in bone levels or periapical changes in relation with 47
 |
Antibiotics and anti-inflammatory drugs were prescribed.The patient was prescribed amoxicillin 250 mg thrice-daily with ibuprofen thrice-daily for three days.
Supragingival scaling was done and scaling and root planing was done in relation to 47, 48 under local anesthesia. The patientwas put on maintenance therapy after review wasdone. (Fig. 3)
 | Fig. 3. : Intra-oral postoperative photograph: Right lateral View showing resolution of gingival abscess in relation with 47
 |
Case2 - Periodontal abscess:
A 35 year old female patient reported to theDepartment of Periodontics, complaining of pain & swelling in the lower left front tooth region for the past 1 week. (Fig. 4) The pain was dull & intermittent & aggravates after taking cold food stuff. On examination, there was a soft, fluctuant swelling in relation to 31, 32. The swelling was ovoid in shape & was associated with 10mm deep periodontal pocket in relation to 32 which was grade 2 mobile. (Fig. 5)
 | Fig. 4. : Intra-oral preoperative photograph: Frontal view showing periodontal abscess in relation with 32
 |
 | Fig. 5. : Intra-oral preoperative photograph: Frontal view showing 10mm deep periodontal pocket in relation to 32
 |
Intraoral peri-apical radiograph with 31, 32 revealed bone loss in relation to 32. (Fig. 6) Considering the history, symptoms and clinical & radiographic findings, the lesion was provisionally diagnosed to be a periodontal abscess.
Antibiotics and anti-inflammatory drugs were prescribed. The patient was prescribed amoxicillin 250 mg thrice-daily and metronidazole 200 mg thrice-daily with ibuprofen thrice-daily for three days.
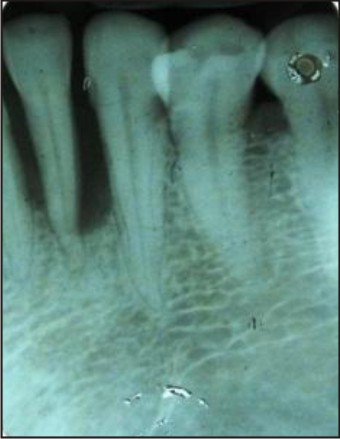 | Fig. 6. : Preoperative Radiographic view: Intraoral peri-apical radiograph revealed bone loss in relation with 32
 |
Supragingival scaling was done and root planing was done in relation to 31, 32 under localanaesthesia. (Fig. 7) Pulp testing,Coronoplasty, Splinting (Fig. 8) was performed there after that. The patient was then put on maintenance therapy.
 | Fig. 7. : Intra-oral postoperative photograph: Frontal view showing resolution of periodontal abscess in relation with 32
 |
 | Fig. 8. : Intra-oral postoperative photograph: Frontal view showing provisional splinting in relation with lower anteriors
 |
Case 3 - Periodontal abscess associated with diabetes:
A 32 years male patient reported to the Department of Periodontics with the chief complaint of swollen bleeding gums on the left side of the upper jaw with pus discharge and loose teeth since 2 months. (Fig. 9) There was bleeding from gums on digital pressure & while brushing. He also experienced difficulty in chewing and biting food and bad breath. Patient is a known diabetic since 8 years & currently under medications. He was on insulin injections (10 units) daily earlier. At present he is taking Gluformin G2 forte - 1 tab in morning and ½ tab at night. Radiograph revealed generalized vertical defect in maxillary posterior teeth, crestal bone loss seen in maxillary anteriors and mandibular arch. (Fig. 10)
 | Fig. 9. : Intra-oral preoperative photograph: Left lateral view showing periodontal abscess in relation with 24
 |
 | Fig. 10. : Preoperative Radiographic view: OPG showing generalized bone loss
 |
A treatment plan was devised for the patient, which included abscess drainage under antibiotic coverage. Antibiotics, Amoxicillin 250 mg thrice daily, Metronidazole 200 mg thrice daily were prescribed for 21 days, Analgesic for first three days thrice daily was also prescribed. Thorough scaling, root planing & curettage of all the areas were performed. Patient was advised to use Chlorhexidine Mouthwash 10 ml of 0.2% twice a day for 15 days and use of interdental floss. Occlusal therapy was done to relieve trauma from occlusion. After the treatment, at subsequent appointments there was reduction in inflammation. Abscess in the maxillary arch was subsided. (Fig. 11) There was generalized reduction in probing pocket depth and mobility of teeth. Improvement was seen in Fasting blood sugar & Random blood sugar levels. Improvement was seen in the oral hygiene as well.
 | Fig. 11. : Intra-oral postoperative photograph: Left lateral view showing resolution of periodontal abscess in relation with 24
 |
Case 4 - Pericoronal Abscess:
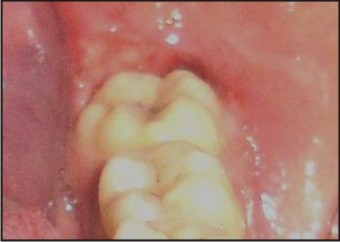
A 38 year old male patient reported to the Department of Periodontics with the chief complaint ofpain in lower right back region of jaw since 4-5 days.Pain was sharp shooting type and continuous throughout the day.Intensity of pain subsided on medication. Complained of bad breath in the mornings and while speaking since 6 months. On examination there was presence of swelling around 38 (operculum). (Fig. 12)
 | Fig. 12. : Intra-oral preoperative photograph: Pericoronal abscess in relation with 38
 |
A treatment plan was devised for the patient, which included scaling, curettage & irrigation of the area around 38 under antibiotic coverage. Operculectomy was performed for removal of operculum over 38. The healing in relation to 38 was uneventful. (Fig. 13)
 | Fig. 13. : Intra-oral postoperative photograph: 7 days post-operculectomy in relation with 38
 |
Discussion:
Periodontal abscess is the third most frequent dental emergency, representing 7–14% of all the dental emergencies. The diagnosis is done by the analysis of the signs and symptoms and by the usage of supplemental diagnostic aids. The treatment of the periodontal abscess has been a challenge for many years. In the past, the periodontal abscess in periodontallydiseased teeth was the main reason for tooth extraction. Today, three therapeutic approaches are being discussed in dentistry, that include, drainage and debridement, systemic antibiotics and periodontal surgical procedures which are applied in the chronic phase of the disease. The localization of the acute periodontal abscess and the possibility of obtaining drainage are essential considerations for successful treatment. Several antibiotics have been advocated to be prescribed in case of general symptoms or if the complications are suspected. Antibiotics like Penicillin, Metronidazole, Tetracyclines and Clindamycin are the drugs of choice.
Treatment of periodontal abscess is divides into 2 parts as: Initial therapy & Definitive treatment.
Initial therapy:
The initial therapy is usually prescribed for the management of acute abscesses without systemic toxicity or for the residual lesion after the treatment of the systemic toxicity and the chronic periodontal abscess.[6], [7]
Basically, the initial therapy comprises of:
a. The irrigation of the abscessed pocket with saline or antiseptics
b. When present the removal of foreign bodies
c. Drainage through the sulcus with a probe or light scaling of the tooth surface
d. Compression and debridement of the soft tissue wall
e. Oral hygiene instructions
f. Review after 24-48 hours; a week later, the definitive treatment should be carried out.
The treatment options for periodontal abscess under initial therapy:
1. Drainage through pocket retraction or incision
2. Scaling and root planning
3. Periodontal surgery
4. Systemic antibiotics
5. Tooth removal
Definitive Treatment:
The treatment following reassessment after the initial therapy is to restore the function and aesthetics and to enable the patient to maintain the health of the periodontium. Definitive periodontal treatment is done according to the treatment needs of the patient.
Conclusion:
The occurrence of periodontal abscesses in patients who are under supportive periodontal treatment has been frequently described. Early diagnosis and appropriate intervention are extremely important for the management of the periodontal abscess, since thiscondition can lead to the loss of the involved tooth. A single case of a tooth diagnosed with periodontal abscess that responds favourably to adequate treatment does not seem to affect its longevity. In addition, the decision to extract a tooth with this condition should be taken, while taking into consideration, other factors such as the degree of clinical attachment loss, the presence of tooth mobility, the degree of furcation involvement, and the patient’s susceptibility to periodontitis due to the associated systemic conditions.
References:
1. HuanXin Meng. Periodontal Abscess. Ann Periodontol 1999; 4:79-82.
2. Herrera D, Roldan S, Sanz M. The periodontal abscess:a review. J Clin Periodontol 2000; 27:377–386.
3. Lewis MAO, Parkhurst CL, Douglas CW, martin MV, Absi EG, Bishpo PA, Jons SA. Prevalence of penicillin resistant bacteria in acute suppurative oral infection. J AntimicrobChemother 1995;35: 785-791.
4. Newman MG, Sims TN. The predominant cultivable microbiota of the periodontal abscess. J Periodontol 1979;50: 350-354.
5. Hafstrom CA, Wikstrom MB, Renvert SN, Dahlen GG. Effect of treatment on some periodontopathogens and their antibody levels in periodontal abscesses. J Periodontol 1994;65:1022-1028.
6. Dello Russo NM. The post-prophylaxis periodontal abscess: Aetiology and treatment. Int J Periodontal Restorative Dent 1985;5:29-37.
7. Smith RG, Davies RM. Acute lateral periodontal abscesses. Br Dent J 1986; 161:176-178.
|