Introduction
The prevalence of dental caries has been reduced over the years due to increased access of fluorides, frequent dental services and increased oral health education on the great part of the population. However, a significant portion of the same population still remains undertreated and show dental cavities as after-effects of this oral disease. In spite of strongly influence of social, economic, cultural, religious and environmental factors on dental caries, its severity may be increased by structural changes of enamel/dentin such those observed in cases of molar incisor hypomineralization (MIH).Molar incisor hypomineralistion (MIH) wasintroduced as a definitive clinical entity byWeerheijm in 2001. She defined MIH ashypomineralisation of systemic origin affecting one, two, three or all first permanent molars (FPMs) and the permanent incisors.[1]
The MIH increases the dental caries risk as consequence of affected teeth because they are not only soft and porous enamel teeth but also very sensitive to stimuli making effective oral hygiene difficult.[2] Several aetiological factors are mentioned as the cause of MIH[3],[4],[5] and they are frequently associated with childhood diseases or nutritional conditions during the first three years of life. [4]
Clinically, MIH can create serious drawbacks for the dentist as well as for the child affected. Moreover, these teeth are very sensitive and often require extensive treatment since rapid breakdown of tooth structure may occur, giving rise to acute symptoms and complicated treatments. Defected enamel teeth require complex treatment solutions and different treatment options will depend on the extension of the defect, degree of tooth eruption, oral hygiene and dietary habits of the patient. According to the severity of the case, the treatment ranges from topical fluoride varnish, to the use of adhesive materials for restorative procedures, or even the extraction of the teeth associated with orthodontic therapy.[5] The child, on the other hand, will experience pain and sensitivity, even when the enamel is intact, suffering from toothache during teeth brushing. Often, there is more difficulty to anaesthetize the MIH molars when treatment is indicated.[6] Apart from the restorative difficulties faced by clinicians, children with MIH experience higher dental fear and anxiety that can be related to pain experienced by the patients during multiple treatment appointments, as many of them were either inadequately anesthetized or even had treatment without local analgesia.[7] It has been shown that children with MIH receive much more dental treatment that unaffected children.[7],[8],[9] Thus, treatment planning should also consider the long-term prognosis of teeth suffering from this condition.
Clinical Features
MIH is a hypomineralized defect of the first permanent molars, frequently associated with affected incisors. The number of affected first permanent molars per patient varies from one to four and expression of the defects may vary from molar to molar. When a severe defect is found within a subject, it is likely that the contralateral tooth is also affected.[10]
The risk of defects to the upper incisors appears to increase when more first permanent molars have been affected. The defects of incisors are usually without loss of enamel substance.[11]
Clinically, the hypomineralized enamel can be soft, porous and look like discoloured chalk or old Dutch cheese. The enamel defects can vary from white to yellow or brownish but they always show a sharp demarcation between the affected and sound enamel. The porous, brittle enamel can easily chip off under the masticatory forces. Sometimes, the loss of enamel (posteruptive enamel breakdown) can occur so rapidly after eruption that it seems as if the enamel was not formed initially. After occurrence of the post-eruptive enamel breakdown, the clinical pictures resembles hypoplasia. In hypoplasia, however, the borders to the normal enamel are smooth, whilst in posteruptive enamel breakdown the borders to the normal enamel are irregular.
MIH can sometimes be confused with fluorosis or amelogenesis imperfecta. It can be differentiated from fluorosis as its opacities are demarcated, unlike the diffuse opacities that are typical of fluorosis and by the structure of the enamel (fluorosis is caries resistant and MIH is caries prone). The cause of fluorosis can, mostly, directly be related to the period in which the fluoride intake was too high. Choosing between amelogenesis imperfecta (AI) and MIH as a diagnosis seems a matter of definition: it should be stressed that, only in very severe MIH cases, the molars are equally affected and mimic the appearance of AI. Mostly in MIH, the appearance of the defects will be more asymmetrical in the molars as well as in the incisors. In AI, the molars may also appear taurodont on radiograph and there is often a history of family onset.
Prevalence
Many prevalence studies for MIH were carried out in various countries and large variations found in the prevalence rates, ranging from 2.5-40.2%.[12],[13] This wide range could be because of difference in recording methods, indices used and different age or population investigated. In some countries, caries levels may mask the true prevalence of MIH.[14],[15],[16] No much difference in prevalence has been reported so far between the male and female genders.[1],[17],[18]
Aetiology
A variety of systematically acting medical factors have been proposed as contributing to or causing MIH, including prenatal, perinatal and postnatal illnesses, low birth weight, antibiotic consumption and toxins from breast-feeding.[19] Children with poor health during the first years of life, the critical period for crown formation of the FPM and incisors, are more likely to be at increased risk for MIH.[20] It also has been proposed that there could be an underlying genetic predisposition that contributes to the risk of developing MIH in at least some cases.[21] The varying degree of enamel defects in FPM and incisors, that develop at the same time, suggest that not all teeth are equally susceptible to enamel defects and developmental disturbances. Either genetic or spatial differences could play a part in the development and variability observed clinically in MIH. Collectively, the majority of previous studies imply that the aetiology of MIH is complex with undetermined systematic and genetic factors disrupting normal amelogenesis in the affected teeth.
Case Report 1
A 9 year old girl reported to the Department of Pedodontics and Preventive Dentistry at Genesis Institute of Dental Sciences and Research, Ferozepur with a chief complaint of decay in lower right and left back region of the jaw since 1 year. No other family member had similar complaints. Personal history includes previous hospitalization at the age of 3-4 years for the treatment of severe chest infection for which intravenous antibiotics were administred.
On intra oral hard tissue examination, it has been revealed that teeth are in mixed dentition stage. It was found that all the four permanent first molar were yellow brown with demarcated opacities (Fig 1).
 | Fig 1: Maxillary And Mandibular Arch Showing Mixed Dentition
 |
Investigation
Intra oral periapical radiograph of teeth 16, 36 and 46 (Fig 2) shows the coronal radiolucency involving complete enamel surface and deep dentinal layer almost approaching pulp indicating irreversible pulpitis and on the teeth 26 coronal radiolucency involving distal side of enamel and dentinal layers indicating dentinal caries without involving pulp.
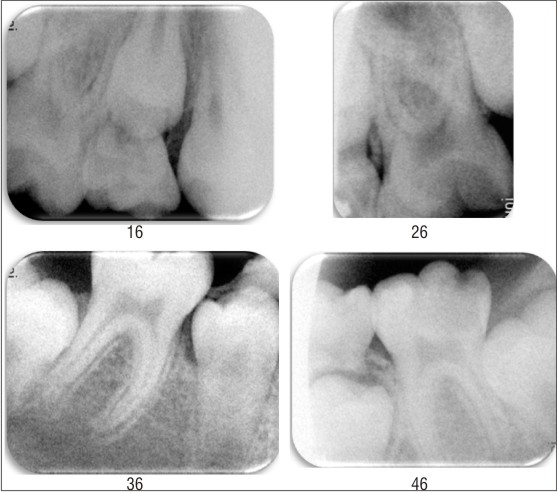 | Fig 1: Maxillary And Mandibular Arch Showing Mixed Dentition
 |
Diagnosis
A case of molar hypoplasia affecting four permanent first molars excluding incisors.
Treatment
Preparatory Phase
- Oral prophylaxis
- Fluoride application
Corrective Phase
- Composite restoration wrt 26
- GIC restoration wrt 65, 75
- Root canal treatment wrt 16, 36, 46 followed by stainless steel crowns (Fig 3, Fig 4)
- Extraction under local anesthesia wrt 55
 | Fig 3: Postoperative View Of Maxillary And Mandibular Arch
 |
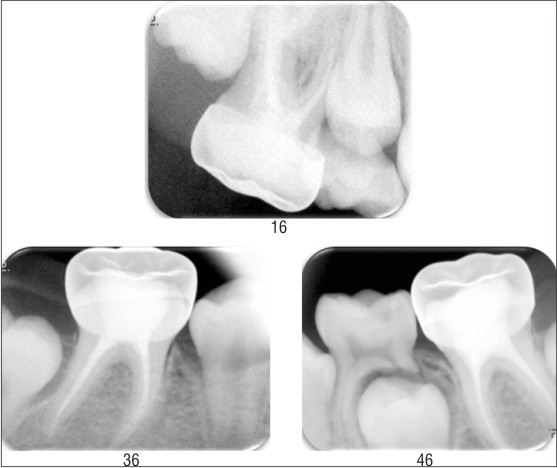 | Fig 4: Post-operative Radiographs Of 16, 36 And 46
 |
Clinical management of the case of molar incisor hypoplasia was challenging due to:
1. The sensitivity and rapid development of dental caries in affected permanent first molars
2. The limited cooperation of a young child
3. Difficulties in achieving anesthesia
4. Repeated marginal breakdown of restoration.
So the treatment of the patient in the initial visits was planned under conscious sedation (Fig 5) to make the patient cooperative and relive the anxiety and fear she has with the dental treatment.
 | Fig 5: Treatment Was Performed Under Nitrous Oxide Inhalation Conscious Sedation Using Pulse Oximeter
 |
Case Report 2
A 10 year old boy reported to the Department of Pedodontics and Preventive Dentistry at Genesis Institute of Dental Sciences and Research, Ferozepur with a chief complaint of pain in lower right and left back region of the jaw since 3-4 months. No other family member had similar complaints. On intra oral hard tissue examination, it has been revealed that teeth are in mixed dentition stage. It was found that the entire four permanent first molars were brownish in colour (Fig 6), extensive post-eruptive enamel breakdown with severe bite collapse (Fig 7).
 | Fig 6: Severe Post Eruptive Enamel Breakdown (Peb) Of All The Four First Permanent Molars
 |
 | Fig 7: Severe Bite Collapse On Both Right And Left Sides
 |
Investigation
Orthopantomogram shows the coronal radiolucency involving complete enamel surface and deep dentinal layer almost approaching pulp indicating irreversible pulpitis with respect to 16, 26 and 36 (Fig 8). Upper and lower impressions were made to diagnose the severity of bite collapse.
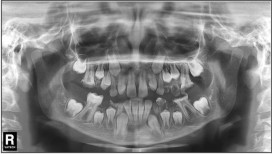 | Fig 8: Pre-operative Orthopantomogram
 |
Diagnosis
A case of molar hypoplasia affecting three permanent first molars excluding incisors.
Treatment
Preparatory Phase
- Oral prophylaxis
- Fluoride application
Corrective Phase
- Composite restoration wrt 46
- Root canal treatment wrt 16, 26, 36 followed by post and core
- Stainless steel crowns wrt 16, 26 and 36 (Fig 9)
- Extraction wrt 54 and 64
 | Fig 9: Post-operative Orthopantomogram
 |
Clinical management of the case of molar incisor hypoplasia was challenging due to:
1. The sensitivity and rapid development of dental caries in affected permanent first molars
2. Extensive post-eruptive enamel breakdown
3. Bite collapse
4. Repeated marginal breakdown of restoration.
With the help of stainless steel crown, bite was raised upto 2-3mm. Patient developed transient tongue thrust habit. This got corrected by itself within 12 months (Fig 10). At the follow up visit, patient’s occlusion was normal but with blocked upper and lower 2nd premolars for which the patient was referred to the department of orthodontics.
 | Fig 10: Immediate Post-operative And Follow Up Occlusion After 12 Months
 |
Discussion
MIH may lead to extensive treatment need. Although children with and without MIH showed similar dental histories concerning their primary dentition, it was found that, after eruption of the first permanent molars by the age of nine, children with MIH were treated ten times as often as children without such molars.[9] The MIH children in this study displayed more dental fear and anxiety compared to the healthy control group. Adequate use of local anaesthesia is regarded as an important factor to prevent dental fear and the reduction of discomfort of the child during treatment. The difference in treatment need was mainly related to the affected teeth.[22], [23]
MIH molars are fragile, caries may develop easily in these molars. This problem is aggravated because the children tend to avoid the sensitive molars when brushing their teeth. If an erupting first permanent molar shows signs of opacities and/or post-eruptive breakdown, the child should be monitored frequently until the moment that all four molars have completely erupted. In order to minimize the loss of enamel and any damage due to caries, both preventive and interceptive treatment is required. Besides normal brushing and education to child and parents, prevention also includes fluoride varnish application and application of glass ionomer sealants. Sometimes the sensitivity of the teeth is decreased by these applications.
The first aim should be relief of pain followed by consideration of the long-term viability of the molars. If restorative treatment is indicated, proper local anaesthesia is mandatory. Adhesive materials should be chosen for these restorations.
In hypersensitive cases, or very severely affected teeth, semi-permanent restorations with stainless steel crowns or adhesive-retained metal castings can be an alternative restoration. Extraction of such molars, combined with orthodontic treatment, should be considered as an alternative treatment, especially if the molars have a poor long term prospect. The optimal time for extraction is indicated by the beginning of calcification of the bifurcation of the roots of the lower second permanent molar (usually around the age of 81/2–91/2 years).
Conclusion
The prevalence of MIH appears to be increasing, and managing affected children is now a common problem for Pediatric dentists. Although the aetiology is unclear and may, in fact, be multifactorial, children born preterm and those with poor general health or systemic conditions in their first 3 years may develop MIH. The early identification of such children will allow monitoring of their PFMs so that remineralization and preventive measures can be instituted as soon as affected surfaces are accessible. The complex care involved must address the child’s behaviour and anxiety, aiming to provide durable restorations under pain-free conditions.
References
1. DaCosta-Silva. et. al. (2010). Molar incisor hypomineralization: prevalence, severity and clinical consequences in Brazilian children. Int J Paediatr Dent. 2010; 20(6):426-434
2. Kilpatrick N. New developments in understanding development defects of enamel: optimizing clinical outcomes. J Orthod. 2009; 36(4):277-282.
3. Alaluusua S. Aetiology of Molar-Incisor Hypomineralisation: A systematic review. Eur Arch Paediatr Dent. 2010; 11(2):53-58
4. Fagrell TG. et al. Aetiology of severe demarcated enamel opacities-an evaluation based on prospective medical and social data from 17,000 children. Swed Dent J. 2011; 35(2):57-67
5. Lygidakis NA. et al. Best Clinical Practice Guidance for clinicians dealing with children presenting with Molar-Incisor-Hypomineralisation (MIH): An EAPD Policy Document. Eur Arch Paediatr Dent.2010; 11(2):75-81.
6. William V. et al. Microshear bond strength of resin composite to teeth affected by molar hypomineralization using 2 adhesive systems. Pediatr Dent.2006b; 28(3):233-241
7. Jalevik B. & Klingberg GA. Dental treatment, dental fear and behaviour management problems in children with severe enamel hypomineralization of their permanent first molars. Int J Paediatr Dent. 2002; 12(1):24-32.
8. Jalevik B. et al. Scanning electron micrograph analysis of hypomineralized enamel in permanent first molars. Int J Paediatr Dent.2005; 15(4): 233-240.
9. Lygidakis NA. Treatment modalities in children with teeth affected by molarincisor enamel hypomineralisation (MIH): A systematic review. Eur Arch Paediatr.2010; 11(2):65-74
10. Alaluusua S. et.al. Polychlorinated dibenzo-pdioxins and dibenzofurans via mother’s milk may cause developmental defects in the child’s teeth. Environ Toxicol Pharmacol 1996; 1:193–197.
11. Weerheijm KL, Groen HJ, Beentjes VEVM, Poorterman JHG. Prevalence of cheese molars in 11-year-old Dutch. J Dent Child 2001; 68:259– 262.
12. Jalevik B. Prevalence and Diagnosis of Molar-incisor-hypomineralization (MIH): A systematic review. Eur Archs Paediatr Dent. 2010; 11(2):59-64.
13. Martínez Gómez TP, et. al. Prevalence of molar incisor hypomineralization observed using transillumination in a group of children from Barcelona (Spain). Int J Paediatr Dent. 2012; 22:100-9.
14. Willmott N. Molar incisor hypomineralization. Dent Nursing. 2011; 7(3):132-7.
15. Mahoney EK, Morrison DG. The prevalence of Molar-Incisor Hypomineralization (MIH) in Wainuiomata children. N Z Dent J. 2009; 105(4):121-7.
16. Crombie F, Manton D, Kilpatrick N. Aetiology of molar-incisor hypomineralization: a critical review. Int J Paediatr Dent. 2009; 19(2):73-83.
17. Preusser SE. et. al. Prevalence and severity of molar incisor hypomineralization in a region of Germany—a brief communication. J Public Health Dent. 2007; 67(3):148-50.
18. Cho SY, Ki Y, Chu V. Molar incisor hypomineralization in Hong Kong Chinese children. Int J Paed Dent. 2008;18(5):348–52.
19. William V., Messer LB., Burrow, MF. Molar-Incisor-hypomineralisation: Review and recommendations for clinical management. Pediatr Dent. 2006; 28(3):224-232.
20. Jalevik B., Noren JG. Enamel hypomineralisation of permanent first molars: a morphological study and survey of possible aetiological factors. Int J Paed Dent 2000; 10: 278-289
21. Brook AH., Smith JM. Aetiology of developmental defects of enamel: a prevalence and family study in East London, UK. Connect Tissue Res. 1998; 39:151-156.
22. Leppäniemi A., Lukinmaa PL., Alaluusua, S. Nonfluoride hypomineralizations in the permanent first molars and their impact on the treatment need. Caries Res 2001; 35: 36–40.
23. Jalevik B., Klingberg G. Dental treatment, dental fear and behaviour management problems in children with severe enamel hypomineralization in their permanent first molars. Int J Paed Dent 2002; 12: 24–32.
|