The word ‘Sport’ is derived from an old combination of words that literally meant “to carry away from work”. Sport also signifies diversion by way of physical amusement.[1] Sports and games form an integral part of the growing up of children and help in toning and strengthening the various muscles and bones. They keep the individual physically fit along with the recreation.[2] Sports practice is beneficial and healthy, although some practices can increase the risk of traumatic injuries to dental and oral tissues.[3] With the current interest in fitness and sports, an ever-increasing number of individuals are participating in a wide range of sporting activities. While fast moving contact sports such as football, rugby, ice hockey, martial arts and basketball are considered the highest risk for facial and head injuries. Soccer, field hockey, baseball, racquetball, and squash also have the potential to cause dento-facial or temporomandibular injuries.
According to the International Academy for Sports Dentistry-‘Sports Dentistry’ is the branch of dentistry that involves prevention of oral sports injuries and treatment of dental athletic injuries. It also involves the collection and dissemination of information on dental athletic injuries and encourages research in the prevention of such injuries.[4] Due to high prevalence of dental trauma in sports, the sports dentistry needs to be established for preventive and therapeutic care of the sports person and especially for paediatric population which is more vulnerable to such injuries. They are liable for more complications owing to growing age and immature bone.
Need For Sports Dentistry:
According to Scott J et al. (1996), dental injuries are the commonest type of orofacial injuries sustained during participation in sports.[5] Types of orofacial injuries commonly observed in sports include injuries to the dentition, namely fractured or avulsed teeth and injuries to the periodontium. Due to direct impact on jaws, injuries resulting in dislocation or fracture of jaws may be incurred. The National Youth Sports Foundation for the prevention of athletic injuries estimates that during each session of play, athletes have a 10 percent chance of sustaining an injury to the face or mouth.[6] Separate studies showed that from 13 to 39 percent of all dental injuries were sports-related and of all sports-related accidents reported, 11 to 18 percent were maxillofacial injuries. Males were affected twice as often as females, with the maxillary central incisor being the most commonly injured tooth.[7],[8] According to Mc Nutt et al in 10-18 years old players, observed oro-facial injuries were 32%, 21.6% & 18.6% in football, basketball and baseball, respectively.[9]
Prevention and adequate preparation are the key elements in minimizing injuries that occur in sports. In recent times, preventive dentistry has emerged as the major focus of dentistry. Awareness amongst sportsperson and various international sports organizations have recognised the need of preventive dentistry in sports. Prevention of such injuries can be achieved through proper patient education, diagnosis, treatment of existing dental problems and designing custom made mouthguards. Contact sports and non-contact sports should be supplemented with protective appliances like mouthguards.
Role of Sports Dentistry or Responsibilities involved in Sports Dentistry:
1. Risk Evaluation
2. Preventive Management
3. Therapeutic Management of Oral and Dental Injuries
1. Risk Evaluation: Risk of dental injury to a sports person should be evaluated in a particular sport to prevent sports related dental injuries. Risk evaluation is based on various extrinsic and intrinsic factors[10]:
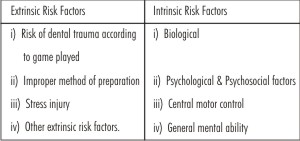 |
 |
a) Extrinsic Risk Factors:
Extrinsic risk factors are independent of the individual and are essentially the injury predictors of that particular sport e.g.
i) Risk of dental trauma according to game played[1]:
High risk sports- football, rugby, ice hockey, martial arts and basketball are considered the highest risk for facial and head injuries.
Moderate Risk Sports - soccer, field hockey, baseball, racquetball, and squash also have the potential to cause dento-facial or temporomandibular injuries.
Low risk sports - non contact sports
ii) Improper method of preparation[11]:
Improper method of preparation for competition such as training errors can be responsible for upto 60% of injuries.
iii) Stress injury[1]:
Chances of stress injury are more in running and jogging as compared to contact sports i.e. football and boxing.
iv) Other extrinsic risk factors[1]:
Other extrinsic risk factors include quality of the playing surface, status of the equipment to be used or worn, climatic conditions as ice rain and the quality of supervision of the participants.
b) Intrinsic Risk Factors[10]:
Intrinsic risk factors are the predisposing characteristics present in the individual sports participant. These are:
I) Biological :
a) Age: Majority of sports injuries occur in adolescents and young adults and that the risk of injury decreased with increasing age.
b) Gender: Injury incidence for men and boys may be due to differences in aggression between the sexes when competing. Men and boys are more likely to participate both in vigorous exercises and sports competitions than are women and girls.
c) Injury history: Certain individuals with injury- prone biologic characteristics may remain at higher risk for a particular injury.
d) Body size: Excessive height and weight predispose athletes to injury.
e) Local anatomy & abnormal biomechanics in any joint: The young athlete who presents with protrusive maxillary permanent central incisors must be considered at substantial risk for dental trauma, “Accident Prone Profile” (Fig.1).
f) Aerobic Fitness: Physical fitness can lessen the onset or symptoms of fatigue. Unfit sports participants would be more prone to injury.
g) Muscle strength, imbalance & tightness: Localized weakness, muscle imbalances or tightness appear to predispose an individual to sports injury.
 | Fig. 1 – Fracture Due To Trauma Prone Dentition
 |
ii) Psychosocial factors:
No significant predictive value for psychological factors has been evaluated despite studies using personality inventories, and measurements of locus of control, trait anxiety and self concept. Any psychological factor that would reduce the participant’s attention to the challenges of the sport and /or increase the possibility of fatigue may be an etiologic factor in sports injury.
iii) Central motor control:
Beginners are at a greater risk of injury in many types of sports than are veterans. Physically handicapped populations, which display central motor disabilities, are probably at a greater potential risk for injuries associated with physical endeavors such as sports, than might be true for those without impaired coordination.
iv) General mental ability:
There is a correlation between sports injuries and lower scores on intelligence tests, suggesting that intelligence may be predictive of injury proneness.
2. Preventive Management: After risk assessment, preventive management of the player should be done to decrease the chances of dental injury. The use of mouthguards, helmets and facemasks has reduced substantially both the number and severity of craniofacial and intra-oral football-related traumatic injuries among amateur adolescent athletes who have been required to use these protective devices while participating in practice sessions as well as in game situations.
Preventive solutions for orofacial injuries are[12]:
- Routine checkups should be done for any physical or mental condition that might cause an unexpected problem during athletic event.
- Completion of any ongoing dental treatment e.g. orthodontic treatment should be done for correction of proclined anterior teeth.
- Use of preventive devices like mouthguards, helmets and face masks should be done under professional guidance.
a) Mouthguard:
Mouthguard is used to protect against bruising of the lips and cheeks, intra-oral soft tissue lacerations, tooth fractures and dislocations, and fractures of the jaws, as well as providing support for edentulous spaces for those athletes who wear removable partial dentures. It also aids in reducing the likelihood of neck injuries, concussion, cerebral hemorrhage, unconsciousness, serious central nervous system damage, and death[13]. Any impact to the lower jaw reduces the possibility of direct impact of head of condyle to the glenoid fossa, thereby decreasing impact and forces to the entire temporal region.
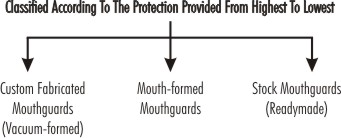 |
 |
 |
 |
Mouthguard is a readymade or custom made device fabricated in such a way so as to provide maximum coverage of overall teeth and is adapted over maxillary teeth unless indicated on mandibular teeth. Materials used have shock absorbing properties and is ethylene vinyl acetate.
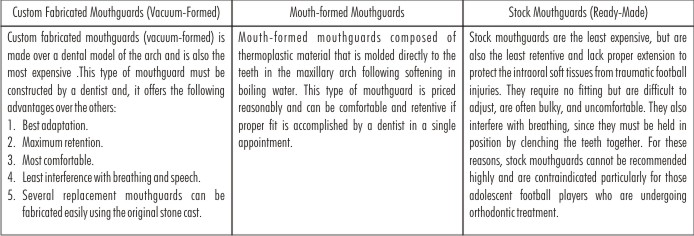
Types of athletic mouthguards:
(According to American Society for Testing and Materials[14])
Maintenance of mouthguard for proper fitting is very important and should be stored in hard, perforated case and should never be kept in warm place or in hot water. It should be cleaned with toothbrush and water, when signs of wearing out are evident, replace it. Parents should always encourage their young kids to wear mouthguards in sports participation. Sports bodies should also make it mandatory to wear protective device in events in contact as well as non-contact sports, as dental injuries unfortunately, are a negative aspect of participation in these sports.
b) Helmet[13]:
Helmets are designed to protect the skin, skull, brain, central nervous system, and ears of the athlete from abrasion, contusion, laceration, fracture, concussion, unconsciousness, cerebral hemorrhage, brain damage, paralysis, and death.
Two basic types of soft protective helmet linings are available:
- One type is known as the suspension helmet which is lined with soft plastic-covered foam that absorbs traumatic forces and possesses the capacity to spring back to the original shape.
- The other is the so-called air helmet, which has the added safety feature of an inflatable bladder to enhance protection.
c) Face mask:
Facemasks are designed to protect against facial injuries to the mouth, nose, eyes, nasal pyramid, and zygomatic arches, depending upon the style of facemask used[15]. One major disadvantage of the facemask is that it presents a protruding object within the ready grasp of an opposing player. When the facemask is pulled or twisted by an opponent during the course of a play, serious physical consequences such as muscle, neck, or spinal column damage can result[13].
3. Therapeutic Management of Oral and Dental Injuries:[16]
Any deviation in the respiratory, cardiac, or vascular function in the athlete must be attended to and may include initiation of cardiopulmonary, respiration, haemorrhage control, and prevention of shock.
a) Soft Tissue Injuries
b) Hard Tissue Injuries
i) Le Fort Fracture I, II, III
ii) Mandibular Fractures
iii) Mandibular Dislocations
iv) Tooth Fractures
v) Tooth Luxations
vi) Tooth Avulsions
a) Soft Tissue Injuries:
Management priorities include controlling haemorrhage and cleaning the wound from foreign materials to permit visibility of the region. Injury to underlying tissues and structures must be determined as well to permit proper management of the entire region. Fractures to the zygomatic, maxillary, and mandibular regions should be ruled out based on the mechanism of the injury, clinical findings, and in some cases radiographs are required ,once the athlete is transported to a medical facility. Assessment of the oral cavity should include ruling out tooth, tongue, vascular and nerve involvement before closure of the superficial lacerations is performed.
b) Hard tissue injuries
I) Le Fort Fracture I, II, III:
These are relatively uncommon in sports. Immediate attention is required to ensure and maintain an airway prior to stabilizing the athlete. It is necessary to control haemorrhage using gentle pressure to the region followed by nasal packing[17]. A complete neurologic examination should be performed to assess the degree of concussion that has occurred and the athlete should be treated for shock and transported to a hospital.
ii) Mandibular Fractures:
Mandibular fractures are relatively common sports-related facial injuries comprising approximately 10% of all injuries to this region[18]. The area most frequently fractured is the supra-condylar region followed by fracture to the body of the mandible. Immediate management include ensuring an appropriate airway because of the potential for respiratory compromise with mandibular pathology. This should include stabilization of the fracture site, assessment for potential concussion, and treatment for shock. Stabilization of the mandibular fracture is easily accomplished using a circumferential compression bandage known as a Barton bandage[17],[19]. Consistent with most injuries resulting from direct trauma to the head, the athlete will likely experience a degree of concussion that must be monitored because of the risk of intercranial hemorrhage. Finally, pain and hemorrhage may induce shock and every effort to prevent this insidious state should occur.
iii) Mandibular Dislocations:
Optimally, management of all dislocations is immediate reduction. Mandibular dislocations present similar problems as the masticatory muscles spasm and stabilize the mandible in its luxated position. Reduction is accomplished by placing the hands bilaterally on the mandible with the thumbs on the anterior region of the mandible and the index and middle finger grasping the mandibular eminence[19].
iv) Tooth Fractures:
Fractures to the crown of the tooth can occur either independently or combined with fractures to the root. Root fractures generally present hyper mobility or can be displaced[20]. These fractures usually require alignment and stabilization by internal fixation[21],[22]. Acute management of a suspected root fracture requires stabilization that can be accomplished by gentle biting on a towel or handkerchief during transport. If the tooth is malaligned or displaced, gentle realignment should be attempted using finger pressure, followed by similar stabilization techniques during transport.In case tooth turns non vital, it needs endodontic treatment (Fig. 4).
 | Fig. 4 - Sequel Of Trauma- 21 Turned Non Vital Tooth
 |
v) Tooth Luxations: (Fig. 2)
Tooth luxation refers to a tooth that has been displaced in one of three positions; extrusively, laterally, or intrusively[23]. Extruded and laterally luxated teeth present a degree of instability and immediate care should be taken for repositioning and stabilization of tooth[23]. An intruded luxation is the only tooth luxation where manipulation should not be encouraged. The evaluation often results in no immediate treatment, but rather the tooth is allowed to re-erupt to reposition itself in several weeks time[20].
 | Fig. 2 - Teeth Displaced Because Of Trauma
 |
vi) Tooth Avulsions: (Fig. 3)
Acute management of an avulsed tooth should include immediate reimplantation, which is essential to maintain vitality of the tooth and its structural components[23],[24]. Immediate reimplantation and avoidance of excessive trauma to the tooth while handling usually results in complete recovery of the tooth[25]. If the tooth has been displaced longer than an hour or if reimplantation cannot be achieved, the tooth should be placed under the athlete’s tongue during transport. Following a complete dental evaluation the tooth is generally stabilized for a period of 2 weeks with internal nylon splinting[26] or an acid - etched composite with a stabilizing wire.
 | Fig. 3 - Avulsed 11 Because Of Trauma
 |
Sports Dentistry - A Growing Concern [27]
The Academy for Sports Dentistry was founded in 1983 in San Antonio, Texas, as a forum for dentists, physicians, trainers, coaches, dental technicians, and educators interested in exchanging ideas related to Sports Dentistry and the dental needs of athletes at risk of sports injuries. Activities include the collection and dissemination of information on dental athletic injuries and the encouragement of research on the prevention of dental injuries to athletes. The Academy boasts an international membership of over 600 members, many of whom are former athletes involved in a wide variety of research activities or with a strong interest in this field of study.
One of the Academy’s most important activities is hosting an annual meeting comprised of scientific sessions and a half day course on the fabrication of professionally diagnosed and designed custom made mouthguards. At that time each participant fabricates the different types of custom mouthguards recommended by the Academy. The Academy's mandate is to welcome interested colleagues from all healthcare disciplines to promote the advancement of research/development and education in this field.
Indian Perspective of Sports Dentistry:
It is advisable for sporting community to have the sports dentistry centres identified for a quick approach when needed. Million of rupees are spent every year in treating dental trauma injuries caused due to sporting accidents. However, in India only a very few athletes wear mouth guards to prevent these injuries.
Perceptions of Chandigarh sports coaches regarding oro-facial injuries and their prevention was evaluated by Lehl G. It was observed that 82% injuries were related to non use of protective devices. For 58% coaches in the study, boxing was more likely to produce oro-facial injuries. The coaches observed more injuries in hockey followed by cricket and boxing.[28] In other studies, 63-75% of such injuries occurred when mouthguard was not used.[9], [29]
Team of doctors including a pediatric dentist, Orthodontist, Oral Surgeon, Physician, Orthopaedic Surgeon, and Laboratory technician skilled in making mouthguards is required to start sports dentistry clinic. In India dental procedures regarding Sports Dentistry should be performed at cheaper costs, with best of quality at various dental clinics situated in different cities. Recently the Department of Sport Medicine introduced at Guru Nanak Dev University (GNDU) has launched India’s first Sports Dentistry Clinic in May 2010.[30]
Conclusion:
Lack of proper measure may lead to minor or major damage having a long lasting impact on patient’s oral as well as general health. “Prevention is better than cure”, says an old adage. This holds true for orofacial injuries in sport events. Sport person should understand that oral protection by way of properly fitted mouthguards will not hamper their ability to perform.
Benefits of Sport Dentistry Treatment in India[4]
Quality service at very competitive cost.
Enhanced awareness of international advanced technology in sports dentistry.
Conjunctional dental service to local and international patients.
References
1. Pinkham JR, Kohn DW. Epidemiology and prediction of sports-related traumatic injuries. In: Ranalli DN, editor. Dent Clin N Am. 1991; 35 (4): 609-626.
2. Be Aggressive [homepage online]. [cited 2012 Feb 07]; Available from: URL: http: //www.ccgrser.org/the-advantages-of-sports.htm
3. Mori GG, Janjacomo DMM, Castilho LR, Poi WR. Evaluating the knowledge of sports participants regarding dental emergency procedures. Dent Traumatol 2009; 25: 305-308.
4. Sports dentistry in India. [web page online]. Health aid India; [cited 2012 Feb 07]; Available from: URL: http://www.healthaidindia.com/dental-treatment/sports-dentistry-in-india.html
5. Scott J, Burke FJT and Watts DC. A review of dental injuries and the use of mouthguards in contact team sports. Br Dent J 1994; 176: 310-314.
6. Padilla R, Balikov S. Sports dentistry: coming of age in the 90s. J Calif Dent Assoc 1993; 21: 27-37.
7. Hayrinen-Immonen R, Sane J, Perkki K,et al. A six-year follow-up study of sports-related dental injuries in children and adolescents. Endod Dent Traumatol 1990; 6: 208.
8. San J. Maxillofacial and dental injuries in contact team sports. Proc Finn Dent Soc 1988; (Supplement VI): 84.
9. McNutt T, Shannon SW Jr, Wright JT, Feinstein RA. Oral trauma in adolescent athletes: A study of mouth protectors. Pediatr Dent 1989; 11: 209-213.
10. Taimela S, Kujala UM, Osterman K. Intrinsic risk factors in athletic injuries. Sports Med 1990; 9: 205-215.
11. McKenzie DC,Clement DB, Taunton JE. Running shoes, orthotics and injuries. Sports Med 1985; 2: 334-347.
12. Gharpure P. Sports Dentistry [home page online]. Smile care 2007. [cited 2012 Feb 07]; Available from: URL: http://www.smilecareindia.com/sports_dentistry.html
13. Ranalli DN. Prevention of craniofacial injuries in football. In: Ranalli DN, editor. Dent Clin N Am 1991; 35(4): 627-645.
14. American Society for Testing and Materials: Standard practice for care and use of mouthguards. Designation: F697-80. Philadelphia, The Society, 1986, p 323.
15. Rontal E, Rontal M. Maxillofacial injuries in football players, an evaluation of current facial protectors. J Sports Med Fitness 1971; 11: 241-245.
16. Lephart SM, Fu FH. Emergency treatment of athletic injuries. In: Ranalli DN, editor. Dent Clin N Am 1991; 35(4): 707-717.
17. Wilson KW. Injuries to the face, ear-nose-throat and airway. In Vinger PF, Hoerner EF (eds): Sports Injuries, ed 2. Littleton, Mass., PSG Publishing, 1986, pp 100-113.
18. Schultz RC: Facial Injuries, ed 2. Chicago, Yearbook Medical Publishers, 1977, pp 231-233.
19. Handler SD: Diagnosis and management of maxillofacial injuries. In Torg JS (ed): Athletic Injuries to the Head, Neck and Face. Philadelphia, Lea and Febiger, 1982, pp 223-244.
20. Greenberg MS, Springer PS: In Torg JS (ed): Athletic Injuries to the Head, Neck and Face. Philadelphia, Lea and Febiger, 1982, pp 245-256.
21. Michanowicz AE, Michanowicz JP, Abou-Rass M. Cementogenic repair of root fractures. J Am Dent Assoc 1971; 82: 569-580.
22. Zachrisson BV, Jacobson I. Long-term prognosis of 66 permanent anterior teeth with root fracture. Scand J Dent Res 1975; 83: 345-354.
23. Bakland LK, Boyne PJ. Trauma to the oral cavity. Clin Sports Med 1989; 8: 25-41.
24. Andreasen JO: Traumatic Injuries of the teeth. St. Louis, CV Mosby, 1972, p 165.
25. Hammartron C, Pierce A, Blomlof L. Tooth avulsion and reimplantation-a review. Endod Dent Traumatol 1986; 2: 1-8.
26. Andreason L, Lindskoy S, Blomlof L. Effects of masticatory stimulation on dentoalveolar ankylosis after experimental tooth reimplantation. Endod Dent Traumatol 1985; 1: 13-16.
27. About the Academy for Sports Dentistry. [home page online]. [cited 2012 Feb 07]; Available from: URL: http://www.academyforsportsdentistry.org/Organization/AboutUs/tabid/94/Default.aspx
28. Lehl G. Perceptions of Chandigarh sports coaches regarding oro-facial injuries and their prevention. J Indian Soc Pedod Prev Dent ; June: 2005.
29. Garon MW, Merkle A, Wright JT. Mouth protectors and oral trauma: A study of adolescent football players. JADA 1986; 112: 663-665.
30. Anon. Varsity starts sports dentistry clinic. The Tribune, Chandigarh, India- Amritsar plus 2010 May 29 [newspaper article online]. [cited 2012 Feb 07]. Available from: URL: http://www.tribuneindia.com/2010/20100529/aplus.htm.
|