Introduction
The gradual wear of the occlusal surfaces of the teeth is a normal process during the lifetime of a patient. However, excessive occlusal wear can result in pulpal pathology, occlusal disharmony, impaired function, and esthetic disfigurement.[1] It has been recognized that tooth wear is becoming increasingly important in the aging population.[2] This may be due to increasing dental awareness, with increased interest in retaining teeth as opposed to having them extracted.[3] Data from prevalence studies have demonstrated high level of tooth wear in adults[4], adolescents[5] and children[6], indicating that tooth wear is a clinical finding in all age groups.
Smith and Robb, in a cross sectional study observed that tooth wear is common in adults, with upto 97% of the study cohort experiencing some tooth wear.[4] However, only 5-7% of the 1007 adults in the study exhibited severe tooth wear, for which interventive restorative treatment was justified.
In a study from United Kingdom, the prevalence of tooth wear was high (57%) in adolescents aged between 11 and 14 years, but dentin involvement was rare.[5] A recent systemic review on the prevalence of in children and adolescents has indicated has indicated that the prevalence of tooth wear leading to dentin exposure in deciduous teeth increases with age, while wear of permanent teeth in adolescents does not correlate with age. It was emphasized that tooth wear is a lifelong cumulative process and should be recorded in both primary and permanent dentitions.
The aim of this review is to provide an insight to etiology and management of worn dentition.
Etiology
Four types of surface loss have been identified, distinguished by the differing causes of loss.[7] Attrition describes mechanical wear resulting from mastication or parafunction, and is limited to the contacting surfaces of teeth.[8] Abrasion denotes the wearing away of structure through some unusual or abnormal mechanical process other than tooth-to-tooth contact.[8] Erosion indicates the progressive loss of tooth structure through chemical processes that do not involve bacterial action producing defects that are sharply defined, wedge-shaped depressions often in facial and cervical areas.[8] Abfraction connotes the pathologic loss of tooth structure attributed to biomechanical loading and resulting in wedge-shaped defects in the cervical areas.[9],[10] These terms describe clinical outcomes of a number of underlying events.[11],[12] (Table 1)
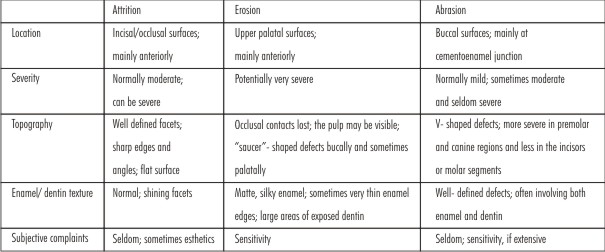 | TABLE 1. Characteristics of Different Wear Mechanisms
 |
Simply the surface loss can be mechanical (attrition & abrasion), chemical (erosion) or biomechanical (abfraction by Grippo)[9] The etiology of pathologic wear resulting from mechanical or chemical causes can be determined by co-relating the location of wear, other signs and symptoms, and information obtained during the patient interview.[7] (Table 2) (Figure 1)
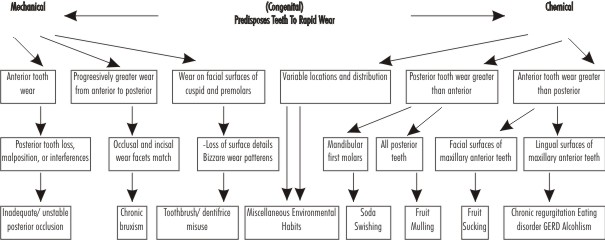 | TABLE 2. Etiology of pathologic wear
 |
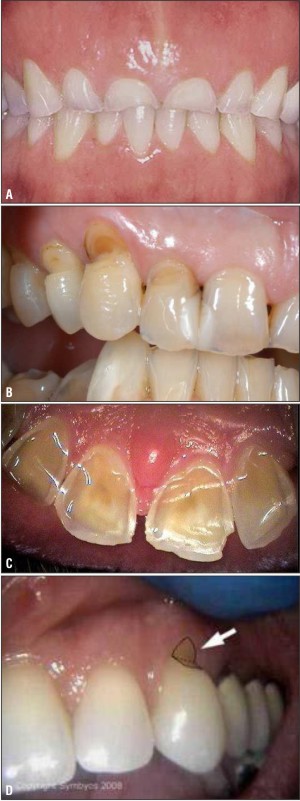 | Figure 1. A. Attrition, B. Abrasion, C. Erosion, D. Abfraction ; Lesions Of Teeth
 |
Most of the times the tooth wear progress with multifactorial etiology.[13] It is generally found that in both arches anterior teeth (and anterior tooth wear indices) exhibit significantly greater wear than posterior teeth.[12] The precise cause of the higher frequency of worn anterior teeth remains unclear. It is generally held that in earlier populations, the excessive wear of molars resulted mainly from a coarser diet and from the more vigorous masticatory activity required. Wear of anterior teeth also results from nondietary functions such as holding and manipulating.[14] It can be speculated that in contemporary humans, wear-inducing factors are likely to affect the anterior teeth more than the posterior. For example, intrinsic acid and bruxism (which are common in modern humans) primarily affect the anterior teeth, while the absence of a coarse diet is less likely to cause wear of the posterior teeth.[13]
Classification By Turner And Missirlain (1984) : [1]
The patients were classified into three categories
Category 1 Excessive wear with loss of vertical dimension.
Category 2 Excessive wear without loss of vertical dimension of occlusion but with space available.
Category 3 Excessive wear without loss of vertical dimension of occlusion but with limited space available
In a typical Category-1 patient there are few posterior teeth and unstable posterior occlusion. There is excessive wear of anterior teeth. The closest speaking space is more than 1mm and interocclusal distance is more than 4mm. There is some loss of facial contour that results in drooping of the corners of mouth.[15] Patients with dentinogenesis imperfecta with excessive occlusal attrition, around 35 years of age and appearing prognathic in centric occlusion also belongs to this category. There is loss of occlusal vertical dimension with concomitant occlusal wear. The loss of vertical dimension can be carefully evaluated using several techniques.[16],[17],[18],[19],[20],[21],[22] At first, a removable splint or partial denture is placed and observed periodically for 6-8 weeks. This is followed by fixed provisional restorations for another 2-3 months before final cementation.
Patient in category- 2 have adequate posterior support and history of gradual wear.1 Closest speaking space of 1mm and interocclusal distance of 2-3mm. Continuous eruption has maintained occlusal vertical dimension leaving insufficient interocclusal space for restorative material. Manipulation of mandible into centric relation will often reveal significant anterior slide from centric relation to maximum intercuspation. Gingivoplasty may be needed to gain clinical crown length. Enameloplasty of the opposing posterior teeth may provide some space for the restorative material.[23]
In patients of category-3, the posterior teeth exhibit minimal wear but anterior teeth show excessive gradual wear over a period of 20-25 years. Centric relation and centric occlusion are coincidental with closest speaking space 1mm and interocclusal distance 2-3mm.[1] It is most difficult to treat because vertical space must be obtained for restorative material.this can be accomplished by fixed or removable anterior bite planes (Dahl appliance)[24],[25],[26], orthodontic movement, tooth preaparation and surgical repositioning of the segments.
The Dahl Concept refers to the relative axial tooth movement that is observed when a localized appliance or localized restorations are placed in supra-occlusion and the occlusion re-establishes full arch contacts over a period of time. The combination of intrusion of the anterior teeth in contact with the appliance and eruption of the separated posterior teeth creates the interocclusal space.[24],[25],[26] (Figure 2) Orthodontic movement usually involves anterior– posterior repositioning of the teeth combined with intrusion, although intrusion is considerably more complex. Tooth prerparation creates the space by reducing the articulating surfaces of the teeth requiring restoration. Surgical repositioning of a segment of teeth and supporting alveolus may be indicated if a dentofacial deformity exists in conjunction with extreme wear.[1]
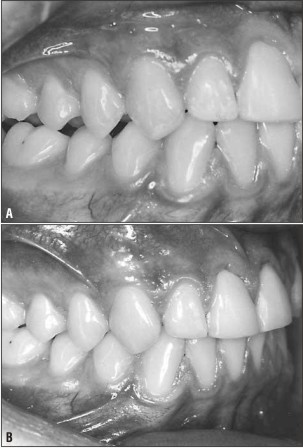 | Figure 2: A. Posterior Teeth Disclusion Immediately After Restoration Of Anterior Teeth With Composite B. Reesthablishment Of Posterior Occlusion After Short Period Of Time
 |
Increasing the OVD to achieve space for restorative materials is seldom advisable; but if deemed necessary, the increase should be minimal and used for restorative needs only.1 Hinge axis location by a kinematic facebow provides greater accuracy in increasing the VDO on the articulator.[27]
Approach Of Restoring Worn Dentition:
A severely worn dentition in the presence of sound periodontium presents unique challenges in patient management, diagnosis, treatment planning, and restorative methodology.
However, a systematic and integrated approach leads to favorable and predictable prognosis. It facilitates development of optimum oral function, comfort, and esthetics, resulting in a satisfied patient.[27] It consists of four logical phases: (I) patient evaluation, (2) comprehensive treatment planning, (3) integrated and systematic reconstruction and (4) postoperative maintenance.
The presenting technique is for restoring the worn dentition at existing vertical dimension of occlusion. But this systematic approach can also be followed for the management of other situations of worn dentition.
Patient Evaluation:
Patient evaluation is subdivided into a preclinical interview and clinical examination. The preclinical interview is conducted during the first appointment. In addition to developing rapport, a thorough general and oral health history is taken. Also the patient's emotional well-being and expectations are noted.[27]
For an assessment of possible causative factors, a systematic history should be taken.[11],[13] (Table 3)
 | TABLE 3: Elements of history to be taken for the individuals with tooth wear
 |
A methodical approach to clinical examination should be followed. Some of the aspects are[11],[13]: (Table 4) Along with this, a thorough examination of the soft tissues and underlying bony contours should be carried out for apparent pathology.
 | TABLE 4: Elements of clinical examination for the individuals with tooth wear
 |
Impressions are taken for two complete sets of diagnostic casts, as well as complete jaw relationship records including a facebow transfer and protrusive and centric relation records are made. Casts are mounted on the semi adjustable articulator of choice. One set of casts is maintained as an unaltered pretreatment record, while the other set is modified during diagnostic treatment planning. The jaw relationship records may not be precise if the patient is suffering from temporomandibular joint dysfunction and/or myofascial pain dysfunction. In those instances, reconstruction should be deferred until these problems are resolved through appropriate therapy. A patient with prolonged occlusal disharmony will often be unable to provide an accurate recording at centric relation as a result of muscle splinting. Effective treatment planning requires the need for comfortable and asymptomatic temporomandibular joints and stomatognathic musculature.[27]
Comprehensive Treatment Planning:
Comprehensive treatment planning is a method of setting goals and then actuating these goals by exercising specific treatment-planning options.[27].
Initially, the progression of wear should be carefully monitored. As the wear normally progresses slowly,the patients seldom have either functional or esthetic complaints. So the need for major restorative work to be routinely carried out is substantially reduced.
Serial investigations should be performed using diagnostic casts at 6 to 12 month intervals (depending on the perceived rate of progression) and recordings compared. Based on an assessment of the rate of wear, (Table 5) it is possible to decide whether intervention is necessary. Usually an interim occlusal splint, especially if bruxism is confirmed, can be provided. This affords some protection while monitoring the progression of wear.[13]
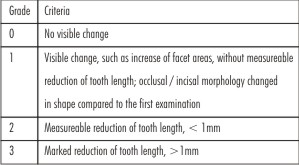 | TABLE 5. Scale used for scoring the progression of occlusal/ incisal wear
 |
When a dominant and active erosive influence has been implicated, rapid deterioration of tooth structures may be expected and serial monitoring is contraindicated. In these cases, reconstructive procedures should be carried out without delay.[11],[13] An integrated treatment plan is first developed on one set of diagnostic casts, properly mounted on a semiajustable articulator using jaw relationship records. This is accomplished by using wax or composite to make reconstructive modifications to the casts. These modified casts become the blueprint for planned occlusal changes and the fabrication of provisional restorations. This blueprint allows for the development of an integrated treatment plan that is properly sequenced and facilitates fabrication of optimal provisional restorations constructed to a new planned functional occlusion.[27]
The treatment goals are[27]: (1) comfortably functioning temporomandibular joints and stomatognathic musculature; (2) adherence to the basic principles of occlusion advocated by Schuyler;[28],[29] (3) anterior guidance that is in harmony with the envelope of function; and (4) restorations that will not violate the patient's neutral zone.
Treatment planning options that may be used to actuate treatment goals are summed up in the "six R's": (1) reshape, (2) restore, (3) remove, (4) reposition, (5) refer in part or totality to another practitioner, and (6) relinquish any action by leaving a tooth alone. These options may be used individually or in any combination to achieve treatment goals[27].
Preoperative treatment planning reconstruction is performed on casts by modification of teeth and the use of diagnostic waxups in the following sequence[27]:
1. Teeth are equilibrated on mounted casts so that centric occlusion and centric relation occlusion are in harmony.
2. Mandibular anterior teeth are modified on diagnostic casts to restore their optimum morphology function, and esthetics.
3. Maxillary anterior teeth are then altered for esthetics and to allow for the function of mandibular anterior teeth at the patient's current vertical dimension of occlusion. Efforts are made to keep the anterior guidance no steeper, and generally shallower, than that with which the patient originally presented.
When dealing with severely worn anterior teeth and very limited interalveolar ridge space, consideration is frequently given to crown lengthening procedures, endodontics, orthodontics, and sometimes extraction and orthognathic surgery.[23],[27],[30]
4. Mandibular posterior teeth are modified to establish the plane of occlusion with the optimum curves of Spee and Wilson using a Broadrick Occlusal Plane Analyzer or “Broadrick Flag”.[31] If necessary, subtle modifications of this optimum plane of occlusion may be made to avoid mutilation of maxillary posterior teeth that might result from strictly following a predetermined occlusal curve.
5. Maxillary posterior teeth are next modified on mounted diagnostic casts so that there is a harmonious cuspal relationship with mandibular dental fossa-receiving areas, free of eccentric interferences and with stable centric stops.
Reconstruction
Integrated and systematic reconstruction of the severely worn dentition is only pursued after a complete and proper comprehensive treatment planning diagnostic waxup has been accomplished on mounted diagnostic casts. Reconstruction is considered to be o four-step process consisting of: (1) fabrication of preparation guides; (2) tooth preparation and provisionalization; (3) fabrication of the final restorations and provisionalization; and (4) final cementation of restorations[27].
Preparation guide, Preparation guides are fabricated from a preoperative treatment planning diagnostic waxup. These generally consist of preparation plane guides made of wax or silicone putty or clear plastic vacuum forms of the newly developed occlusal design. These guides show the amount of occlusal tooth reduction necessary to accommodate planned relationships developed from the treatment planning diagnostic waxup.[27]
Tooth preparation and provisionali zation, Tooth preparation and provisionalization are generally carried out in two stages, with the maxillary and mandibular arches prepared separately on successive days. Tooth preparation should be done meticulously to protect the health and integrity of the periodontium.[32] Acrylic provisional restorations are cemented with temporary cement. A patient is allowed to wear these provisional restorations for an appropriate amount of time to refine and confirm functionality of the occlusal design developed.[27] T-scan technology is a recent advancement which can detect any interference in occlusion. It allows to functionally balance the teeth with high degree of precision.[33] This time period also allows for any additional modifications necessary to enhance esthetics and patient comfort.[27]
Fabrication of final restorations, All final impressions are made with provisional restorations in place, except for those teeth that are the focus of a specific step. In case of an opposing occlusion of tooth enamel, most of the studies prefer metal occlusal surface and preferably one of the high noble content is preferred to minimize the wear of the natural dentition.[27]
1. Mandibular anterior teeth receive provisionally cemented final restorations first.
2. Maxillary anterior teeth are restored next.
After the provisional cementation of mandibular anterior final restoration, anterior guidance is reproduced with a customized anterior guide table on a semiadjustable articulator. Optimal anterior guidance should demonstrate: (1) sound centric stops that fall on flat receiving areas in both centric relation closure and postural closure; (2) immediate protrusive disclusion usually by the central incisors; (3) working disclusion caused by contact of the mesial lingual surface of the maxillary canine against the distal incisal bevel of the mandibular canine; and (4) a smooth parafunctional crossover position that preferably has no eccentric contact on the lateral incisors.
3. When the anterior guidance is found to be satisfactory, mandibular posterior teeth are restored with final restorations cemented provisionally.
4. Finally the maxillary final restorations are provisionally cemented.
Final cementation, Provisionally cemented final restorations are monitored for comfort, stability and optimum function for several weeks and in certain special cases for months or a year or two before final cementation. Many cement bond failures result from cross-arch torque'' as well as from harmful parafunctional and horizontal occlusal forces. These factors are minimized by using the systematized approach and meticulous occlusal adjustment.[27]
Occasionally a provisionally cemented restoration loosens. Upon close examination, a slight dislodging eccentric interference that breaks the temporary cement seal is frequently found. Occlusal adjustment resolves such a situation and further refines final treatment outcomes.
When the reconstructed dentition has been found to fulfill the basic objectives of oral rehabilitation, such as optimum function and stability, easy maintenance and improved esthetics and comfort, the restorations are cemented with a final luting agent.[27] (Figure 3)
 | Figure 3. A. Before Treatment B. After Treatment Of A Patient With Generalized Worn Dentition
 |
Postoperative Maintenance:
Postoperative maintenance may need to include management of parafunctional activity such as bruxism, which is often associated with a severely worn dentition. In addition to making the patient aware of the need to control such a habit during waking hours, the patient should wear an occlusal guard at night. With optimum occlusion the tendency to clench and grind teeth is reduced. Patient behavior modification may also be a necessary adjunctive therapy to control the stress- habit patterns often associated with long-term parafunctional activity.[27]
Patients presenting with combination of short clinical crowns, differential wear and bruxism, etc., increase the risks of cementation failure. Similarly, erosion-induced wear may continue even in the presence of teeth with full coverage crowns and can progress cervical to the crowned tooth if causative factors have not been eliminated. In addition, occlusal splint treatment in combined attrition (bruxism) and erosion cases may not be successful [11],[13]
Patients should be reviewed at least annually; at this time, new study casts, and photographs should be made. A careful clinical and radiographic examination of abutments should be performed: caries, failed retention, wear facets, porcelain integrity, etc., must be checked, recorded, and treated as necessary.[11],[13]
Conclusion:
Tooth wear is a multifactorial process. Its progress is usually slow and generally accompanied by dentoalveolar compensation. In the absence of overwhelming pathology, this process keeps the facial height constant. Continuous apposition of alveolar bone as a tooth erupts to compensate for wear can seriously reduce interalveolar space.
The reconstructive problem of limited interalveolar ridge space can be managed by developing a systematic treatment plan on diagnostic casts. The modified treatment planning diagnostic casts can then be used as guide to dental preparation, provisionalization to an optimum occlusion and final restoration for successful clinical outcome.
References
1. Turner KA, Missirlian DM. Restoration of the extremely worn dentition. J Prosthet Dent 1985; 52:467-74.
2. Mair L, Stolarski T, Vowles R, Lloyd C. Wear: mechanisms, manifestations and measurement. Report of a workshop.J Dent. 1996; 24:141–148.
3. Jagger D, Harrison A. An in vitro investigation into the wear effects of unglazed, glazed, and polished porcelain on human enamel. J Prosthet Dent. 1994;72:320–323.
4. Smith B, Robb N. The prevalence of toothwear in 1007 dental patients. J Oral Rehabil. 1996;23:232–239.
5. Bartlett DW, Coward PY, Nikkah C, Wilson RF. The prevalence of tooth wear in a cluster sample of adolescent schoolchildren and its relationship with potential explanatory factors. Br Dent J. 1998;184:125–129.
6. Dugmore CR, Rock WP. The prevalence of tooth erosion in 12-year-old children. Br Dent J. 2004;196:279–282.
7. Verrett RG: Analysis of etiology of an extremely worn dentition. J Pros 2001;10:224-233
8. Glossary of Prosthodontic Terms, ed 8. J Prosthet Dent 2005.
9. Grippo JO: Abfractions: A new classification of hard tissue lesions of teeth. J Esthet Dent 1991;3:14-19
10. Lee WC, Eakle WS: Stress-induced cervical lesions: Review of advances in past 10 years. J Prosthet Dent 1996;75:487- 494
11. Johansson A, Johansson A, Omar R, Carlsoon G. Rehabilitation of the worn dentition. J Oral Rehabil 2008; 35:548-566
12. Johansson A. A cross-cultural study of occlusal tooth wear [PhD thesis]. Swed Dent 1 1992:(suppl e6):1-59.
13. Johansson A, Omar R. Identification and management of tooth wear. Int J Prosthodont 1994; 7: 506-516
14. Varrela J. Effects of attritive diet on craniofacial morphology: A cephalometric analysis of a Finnish skull sample. Eur J Orthod 1990:12:219-223.
15. Rivera-Morales WC, Mohl ND. Restoration of the vertical dimension of occlusion in the severely worn dentition. Dent Clin North Am 1992;36:651-64.
16. Silverman MM: Determination of vertical dimension by phonetics. JPD 1956;6:465-71
17. Shanahan TES: Physiologic vertical dimension and centric relation. JPD 1956; 6:741-747
18. Thompson JR: The rest position of mandible and its significance to dental science. J Am Dent Assoc 1946; 33:151-180
19. Boos RH. Intermaxillary relation established by biting power. J Am dent Assoc. 1940; 27:1192-1199
20. Silverman MM. The speaking method in measuring vertical dimension. J Prosthet Dent 1953;3:193.
21. Atwood DA: A cephalometric study of the clinical rest position of the mandible. J Prosthet Dent 1956;6:504.
22. Heartwell CN, Rahn AO. Syllabus of Complete Dentures (ed 3), Lea & Febiger: Philadelphia; 1980.
23. Krishna M.G., Rao K.S., Goyal K. Prosthodontic management of severely worn dentition: including review of literature related to physiology and pathology of increased vertical dimension of occlusion. J Ind Prostthodontic Society 2005; 5:89-93
24. Dahl B L, Krogstad O, Karlsen K. An alternative treatment of cases with advanced localised attrition. J Oral Rehabil 1975; 2:209–14.
25 Carlsson G E, Ingervall B, Kocak G. Effect of increasing vertical dimension on the masticatory system in subjects with natural teeth. J Pros Dent 1979; 41:284–9.
26 Dahl B L, Krogstad O. Long-term observations of an increased occlusal face height obtained by a combined orthodontic/prosthetic approach. J Oral Rehabil 1985; 12:173–6.
27 Stewart B. Restoration of the severely worn dentition using a systematized approach for a predictable prognosis. Int J Periodont Rest Dent 1998:18:47-57.
28 Schuyler CH. Correction of occlusal disharmony of the natural dentition. N Y State Dent J 1947:13:445-462.
29 Schuyler CH. The function and importance of incisal guidance in oral rehabilitation.. J Prosthet Dent 1963:13:1011-1029.
30 Chu FCS, Siu ASC, Newsome PRH, Chow TW and Smales RJ. Restorative management of the worn dentition: Localized anterior tooth wear. Dent Update 2002; 29: 214-222
31 Dawson PK. Evaluation, Diagnosis, and Treatment of Occlusal Problems, ed 2. St, Louis: Mosby, 1939.
32 Wilson RD, Maynard G. Intercrevicular restorative dentistry, Int J Periodont Rest Dent 1981:1(1 ):35-43
33 Montgomery MW. T- scan dental force analysis for routine dental examination. Dentistrytoday. Com. July 2011.
|