Introduction
Restoration of the severely broken down dentition is one of the most demanding procedures in dentistry.The steps involved in treatment of these patients include a comprehensive examination, diagnostic mounting and diagnostic wax-up, careful planning and sequencing of various steps, discussion with the patient of the different treatment alternatives and careful execution of the treatment plan[1],[2],[3].
In order to successfully restore and maintain the teeth, one must gain insight into how the teeth arrived at this state of destruction Tooth wear can result from caries, abrasion, attrition, and erosion. While all occlusions wear to some degree over the lifetime of the patient, normal physiological wear usually does not require correction. Severe or excessive wear due to any of the reasons results into tooth destruction that requires restorative intervention[4],[5]. Once a complete recognition of the etiology of present state of dentition is made, a treatment plan can be formulated, based on the number of teeth to be treated, condylar position, space availability, the occlusal vertical dimension of occlusion (OVD), and the choice of restorative material.
The etiology of loss of vertical dimension for this patient was primarily dental decay in the upper arch, because of lack of oral hygiene maintenance due to blindness; however, it can be hypothesized that the blind patient also had a history of stress which may have led to parafunctional occlusal habit and started grinding her anterior teeth. Once the anterior teeth got shorter, the patient lost anterior guidance and further developed posterior interferences [6].The posterior interferences in lateral excursions activated the masseter and temporalis muscles, generating more forces on the teeth. Therefore it was paramount to adopt an occlusal scheme that prevented the future destruction of the new restorations at the increased vertical dimension - a mutually protected occlusal plan was implemented [7].
The present case demonstrates the restoration of masticatory efficiency &esthetics of a blind elderly patient with endodontics & metal free restorations of the maxillary arch alone while also raising the collapsed occlusal vertical dimension(OVD) of the patient along with. As anatomy & physiology of the mandibular teeth, mandibular plane of occlusion & the cervicoincisal length of the lower anteriors appeared satisfactory it wasn’t deemed necessary to fiddle with the lower arch as well. Therefore, a minimally invasive treatment plan was formulated & executed through a combination of dental occlusion, dental balance, and functionality with dental esthetics while, keeping in mind the patients needs & also preserving the sanctity of the entire stomatognathic system[8],[9].
Clinical Report
A 64 yr old blind female patient reported with the chief complaint of inability in mastication & her relatives complained of foul smelling & an unaesthetic mouth. Clinical examination revealed severely carious & broken down anterior and posterior maxillary teeth (Fig. 1, 2). Intraoral examination revealed over closure due to generalized caries & subsequent breakdown of maxillary teeth, however mandibular teeth appeared normal (Fig. 3). Extraoral examination revealed no facial asymmetry or muscle tenderness. The mandibular movements were normal, TMJ evaluation was unremarkable with normal jaw opening and range of motion, no joint sounds, signs or symptoms of instability. Facial appearance showed wrinkles, and drooping commissures at the corner of the mouth indicating loss of vertical dimension .Facial measurements showed increased interocclusal distance far beyond the normal (2–4 mm) due to carious breakdown of upper dentition. Phonetic examination revealed —the S sound altered to F due to increased interocclusal space.
 | Fig. 1 Preoperative extra oral view
 |
 | Fig. 2 Preoperative extra oral view
 |
 | Fig. 3 Preoperative intraoral view
 |
Impressions for study casts were made with irreversible hydrocolloid material along with a centric relation occlusal record.The patient’s casts were mounted on a fully adjustable articulator (Stratos300-Ivoclar Vivadent) using face bow (Fig. 4) and the centric relation record. After studying & mounting the diagnostic casts, it was observed that because of the destruction of upper teeth, maxillary occlusal plane was nonexistent; however the lower teeth were normal without any significant signs of wear or decay & exhibited a regular harmonious occlusal plane.
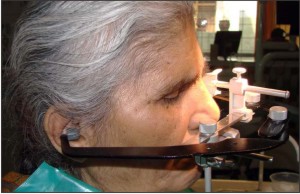 | Fig. 4 Facebow recording
 |
From all the aforesaid assessments, it was decided that apart from restoration of maxillary teeth to normal health & function, the vertical dimension of the patient had to be increased to a proper comfortable position which is called the physiological neuromuscular rest position. The findings were explained to the patient & her relatives, and treatment options were presented. The treatment goals were to restore function, lost occlusal vertical dimension (OVD), to correct the maxillary occlusal plane, and to restore the esthetics of the patient’s dentition.
The first step in this case was to determine how much to increase the patients vertical dimension. Although there is more than one way to find this physiologic position, in this case we used the esthetic & phonetic method to determine the correct resting position of mandible where the muscles are at rest. The facial measurements showed an increase by 4mm of the existing OVD in order to have a comfortable phonetics & pleasing esthetics. The new OVD was set by 4mm increase in incisal guidance pin of the articulator .Diagnostic wax up (Fig. 5) of the upper arch was performed at the new VD & a putty index in poly vinyl siloxane was made from it.
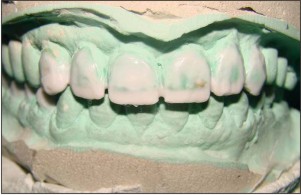 | Fig. 5 Diagnostic wax up
 |
Following this endodontic treatment was performed on all the remaining maxillary teeth & composite build up done in order to lengthen & reinforce them to receive & retain the crowns. Thereafter crown preparations for all ceramic crowns was performed on all the upper teeth A full-arch polyether impression (3M ESPE, Impregum) of the prepared upper arch was then taken, & along with the registered bite (Fig. 6), sent to the laboratory for the fabrication of temporaries. Then using the indirect technique, the putty index made from the diagnostic wax up was used to fabricate provisionals on this cast with the with Temp Bond auto polymerizing resin (3M ESPE, Germany). The temporaries were then tried in the mouth for fit, esthetics & comfort. Necessary adjustments were made in the centric & eccentric movements. After the required reshaping in the mouth to achieve ideal contour, temporaries were cemented using eugenol free temporary luting cement (Rely X Temp NE, 3 M ESPE, Germany).
Once the provisional restorations were equilibrated and the aesthetics and phonetics were deemed satisfactory, the adaptation of the patient to increased VD was evaluated during 6-week period. No muscle tenderness or discomfort in TMJ was noted during this period. Once the occlusal adjustments, speech and esthetics appeared satisfactory, an occlusal bite record was taken with the provisionals against the mandibular naturals. Casts were mounted on the articulator with facebow transfer and the occlusal bite record taken in centric and eccentric relations. These records along with digital photographs of the preparations and provisional restorations were sent to the ceramist so that he had all the information necessary to fabricate the definitive restorations. The provisional restorations were removed & an impression of the maxillary preparations made in putty wash technique using 3M ESPE rubber base Express XT Putty soft & Express XT light body (Germany) & model poured in TypeIV die stone (Kalabhai).The mandibular model was next mounted against the maxillary preparation model with the first set of bite records (Fig. 7). Definitive Zirconia based restorationsin the form of individual crowns were fabricated for each crown preparation (Fig. 8). The Zirconia copings were first tried in the oral cavity for fit & clearance (Fig. 9). The definitive restorationswere then tried in the oral cavity in both centric & eccentric contacts.The scheme of occlusion given to the patient was mutually protected occlusion & was checked for canine disclusion on both sides in laterotrusion & disclusion of posteriors during protrusion.Then arch was evaluated for aesthetics, occlusion, and phonetics (Fig. 10, 11). Since the ceramist followed the guidelines of the provisional restorations, minimal adjustments were necessary at this stage. Final equilibration of the case was accomplished with a leaf gauge.
 | Fig. 6 Bite-registration at increased vertical dimension
 |
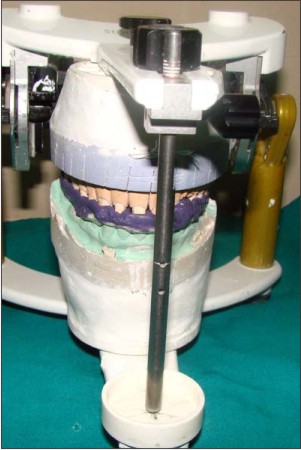 | Fig. 7 Mounting the maxillary preparation model on the articulator with bite at raised vertical dimension
 |
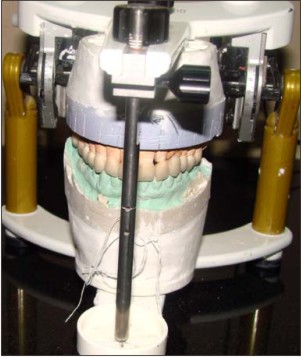 | Fig. 8 Definitive zirconia restorations on the articulator
 |
 | Fig. 9 Tryin of Zirconia copings
 |
 | Fig. 10 Postoperative intra oral view
 |
 | Fig. 11 Postoperative extra oral view
 |
Thereafter, the definitive crowns were temporarily cemented & patient was evaluated for next 48 hrs for any signs of discomfort. Following this period the required minor occlusal corrections were made & after making the needed adjustments, the crowns were glazed and bonded individually to their respective preparations. Bonding involved etching the undersurface of the crowns with hydrofluoric acid for 30 seconds, followed by complete rinsing off the acid with water. 3M silane coupling agent was then applied to the undersurface for 10 seconds & dried off. Then resin bonding was carried out using Relyx U200 (3M Germany). The patient was instructed oral hygiene maintenance and was advised six monthly check-up. A protective splint was fabricated to prevent further damage to the restoration.
Discussion
Complete oral rehabilitation is the combination of dental occlusion, dental balance, and functionality, with dental esthetics. The goal for a clinician is to find a position in which the masticatory function, facial & dental esthetics must be enhanced. Immediate value for the patient is determined by the esthetics of the case, the comfort of the reconstruction and the care in which the dentistry was delivered. Long-term value will be determined by longevity and continuing patient satisfaction [10].
Understanding what determines the VDO and what the effects of altering it have on the temporomandibular joint(TMJ), muscle comfort, bite force, speech, and long term occlusal stability are prerequisites to restoring the worn dentition [11]. Spear clearly outlines the principles of VDO and concludes that patients can function at many acceptable vertical dimensions, provided the condyles are functioning from centric relation and the joint complex is healthy. He states that “vertical is a highly adaptable position, and there is no single correct vertical dimension.” He further concludes that the best vertical dimension is the one that satisfies the patient’s aesthetic desires and the practitioner’s functional goals with the most conservative approach[12],[13].
While increasing the vertical dimension of a dentate patient, a mutually protected occusal scheme is considered most protective to the long term health of the restorations & stomatognathic system as opposed to group function.Studies have shown that in lateral excursive movements, the anterior teeth can best receive and dissipate the forces and posterior contacts in excursions appear to provide unfavorable forces to the masticatory system because of the amount and direction of the applied forces[14]. Posterior simultaneous contacts and canine guidance with posterior disclussion and no anterior posterior discrepancy (centric relation=centric occlusion, CR=CO) should be considered the gold standard for any reorganized approach to the occlusion be it aesthetically or functionally driven.
Anterior guidance plays a very important role in full mouth rehabilitation following centric relation. The anterior guidance forms the anterior control to provide posterior disclusion [6]. The job of anterior guidance is to protect the posterior teeth from lateral or protrusive stresses. The facebow transfer is a must to relate the anterior guidance with the opening and closing axis. It is required to reproduce the arc of closure from the patient to the articulator[15]. The three main things to be taken care of while replacing posterior teeth, are achieving posterior disclusion, establishing the plane of occlusion and deciding the type of occlusal scheme[16]. Disclusion refers to separation of opposing teeth during eccentric movements of mandible, as reported by D’Amico[17]. Posterior occlusion should have equal simultaneous contacts so that it does not interfere with either the TMJs in the back or the anterior guidance in the front. Occlusal interference can be detrimental to the health of the patient. A proper plane of occlusion must permit disclusion of all the teeth on the balancing side when the mandible is moved laterally. The reconstruction of vertical dimension of occlusion should be done at the centric relation and it should be acceptable for the patient at the neuromuscular level [10].
One of the most difficult decisions facing clinicians is related to metal ceramic crowns versus all-ceramic alternatives [18]. Metal-ceramic crowns continue to be the most frequently used full-coverage restoration, and when coupled with the use of porcelain facial margins, proper tooth preparation, and soft tissue management, provides the best combination of decent esthetics and clinical longevity. Although many advances have been made with high-strength all-ceramic crowns, they should continue to be used with caution and only in those patients who demand the ultimate in esthetics or who have a demonstrated allergy to specific metal elements. In this case even though the patient was blind &esthetics wasn’t a major concern, still zirconia restorations were chosen as the material of choice because of reported allergy to some metals [19],[20].
Also, whenever there is a wear& breakdown in only one arch & no wearing in the other, then the preparation & rebuilding can be restricted to the same arch to achieve the desired result [10]. This case demonstrates that spectacular functional & cosmetic results can be provided if appropriate diagnosis & treatment planning are done. We should weigh & consider the different treatment modalities available for complete oral rehabilitation & apply the one that is in the best interest of our patient.
Conclusion
Ultimately, complete oral rehabilitation should be a treatment modality that not only focuses on the esthetics and functional aspect of the dentition but at the same time be minimally invasive in nature. The goal for a clinician is to find a position in which the masticatory function, facial & dental esthetics must be enhanced with least amount of intervention. The aim of oral rehabilitation should be make the teeth fit the jaw-to jaw relationship, not vice versa. In fact care should be taken with occlusal philosophies that strictly believe in preparations of all the 28 teeth for full mouth rehabilitation.In the end all treatments should be designed keeping in mind improvement in the health of the entire stomatognathic system.
References
1. Rivera-Moreles WC, Mohl ND. Restoration of vertical dimension of occlusion in the severely worn dentition.Dent Clin North Am 1992;36(3):651-64
2. Dawson P E. Evaluation, diagnosis and treatment of occlusal problems. pp 280-285. St Louis, MO: CV Mosby, 1989.
3. Binkley TK, Binkley CJ. A practical approach to full mouth rehabilitation. J Prosthet Dent 1987;57(3):261-6.
4. Verrett RG. Analyzing the etiology of an extremely worn dentition.J Prosthodont 2001;10(4):224-233
5. Litonjua LA, Andreana S, Bush PJ, Cohen RE. Tooth wear: Attrition,erosion, and abrasion. Quint Int 2003;34(6):435-446.
6. Schuyler CH. The function and importance of incisal guidance in oral rehabilitation, 1963. J Prosthet Dent2001;86(3):219-32.
7. Pokorny PH, Wiens JP, Litvak H. Occlusion for fixed prosthodontics: a historical perspective of gnathologicalinfluence. J Prosthet Dent 2008;99(9):299-313
8. Goldman I. The goal of full mouth rehabilitation. J Prosthet Dent 1952;2(2):246-51
9. Bloom DR, Padayachy JN.Smile lifts — A functional and aesthetic perspective Br DentJ2006;200(4):199203
10. Bloom DR, Padayachy JN. Increasing occlusal vertical dimension- Why, When and How. Br Dent J2006;200(5):251-256.
11. Thompson JR: The rest position of the mandible and it significance to dental science. J Am Dent Assoc 1946;33:151-180.
12. Spear FM. Approaches to vertical dimension. Adv EsthetInterdiscip Dent 2006;2(3):2-12.
13. Sesemann MR. Enhancing facial appearance with aesthetic dentistry, centric relation, and proper occlusal management. Pract Proced Aesthet Dent 2005;17(9):615-620
14. Boos RH: Intermaxillary relation established by biting power. J Am Dent Assoc 1940;27:1192-1199
15. Long JH Jr. Location of the terminal hinge axis by intraoral means.J Prosthet Dent 1970;23(1):11-24.
16. Sanjana nayar et al .Full mouth rehabilitation of severely attritted dentition. Indian Journal of Multidisciplinary Dentistry 2011; 1(3): 157-160
17. D’Amico, A.: The canine teeth - Normal functional relation for the natural teeth of man. JSouthern Calif Dent Assoc 261:198,1958.
18. Donovan TE. Metal-free dentistry: consumer generated or marketing hype?J Esthet Restor Dent 2002; 14:71–73.
19. Donovan TE, Cho GC. Predictable esthetics with metal-ceramic and all-ceramiccrowns: the critical importance of soft tissue management. Periodontol 20002001; 27:121–130
20. Donovan TE, Cho GC. The role of all ceramic crowns in contemporary restorative dentistry. J Calif Dent Assoc 2003;31:565–570
|