Introduction
Marginal tissue recession (MTR) is a clinical condition in which the marginal periodontal tissue is located apical to the cemento-enamel junction (CEJ) which can lead to dentinal hypersensitivity, may compromise the width of attached gingiva, vestibular depth and desirable esthetics etc. Routinely, class III MTR is treated by two stage surgical procedure which can lead to inconvenience and certain complications[1]. So, single stage surgical approach has been attempted for treatment of Mahajan’s modification of Miller’s class III MTR of maxillary right lateral incisor by utilizing a synchronized combination of three barrier technique to achieve root coverage associated new attachment.
Case Report
A 15 year old patient visited the outpatient Department of Periodontology , Surendera dental college and research institute with chief complaint of receeded gum with respect to upper right second tooth since 2-3 months. Patient past dental history reveals 6 months back he had pain and swelling w.r.t 11 and 12 for which the root canal treatment was carried out by private practitioner but lesion reoccurred after 2 months and retreatment with periapical curretage was carried out after which he experienced MTR w.r.t 12. Patient was esthetically conscious, feared of loosening the tooth.
Patient was non smoker, having good health with no associated systemic problem. Upon clinical examination, mahajan modification of miller’s[2] class III MTR extending from CEJ to the root apex with lack of attached gingival, with class II and class I papillary height w.r.t 11,12 and 12,13 respectively( Norland and Tarnow 1998 classification) ,with compromised aesthetics on smiling w.r.t 12. MTR extended 10 mm vertically (Fig.1) and 3, 2 and 1 mm horizontally just apical to CEJ, at coronal, mid and apical 1/3rd of buccal surface of 12 respectively (Fig.2). Periodontal probing was 5mm w.r.t mesial aspect of 11,12, 13 .
 | Fig. 1 Pre operative view showing MTR of 10mm
 |
 | Fig. 2 Preoperative view - horizontal MTR of 3mm at coronal 1/3rd
 |
 | Fig. 3 Pre operative IOPA indicates resolved periapical lesion with interdental bone loss in the coronal 1/3rd area.
 |
Radiographic examination revealed radiopaque material in the root canal of 11, 12 with resolved periapical lesion and interdental bone loss limited to the coronal 1/3rd (Fig.3 ).
Patient was instructed to maintain the strict oral hygiene and phase I therapy was performed. The objective of the present surgical procedure was not only to obtained aesthetically acceptable root coverage but also gain in clinical attachment and width of attached gingiva. Therefore , a synchronized combination of chemical (tetracycline root conditioning (TRC)), biological (subepithelial connective graft (SCTG)) and physical barrier (coronally advanced pedicle flap) in one stage surgerywas proposed to be the best and economical option. An written informed consent was procured for the same .
Surgery was performed under strict aseptic conditions under local anesthesia, internal bevel incision (Fig.4) was given w.r.t 12 followed by crevicular incision (Fig.5) w.r.t 11,12,13. Full thickness flap was raised (Fig.6) beyond mucogingival junction and the periosteum was incised to form split thickness flap using sharp dissection with surgical blade no. 15 to facilitate the coronal advancement of pedicle flap without tension. Root planning and root prominence finishing done followed by TRC (Fig.7). After harvesting SCTG measuring approximately 15,11 and 1.5 mm in width, length, thickness using trap door technique(Fig.8,9), suturing was done (Fig.10) over the donor site.
 | Fig. 4 Internal bevel incision given
 |
 | Fig. 5 Crevicular incision given
 |
 | Fig. 6 Full thickness flap reflection with interdental bone loss
 |
 | Fig. 7 During tetracycline root conditioning
 |
 | Fig. 8 SCTG obtained using trap door technique
 |
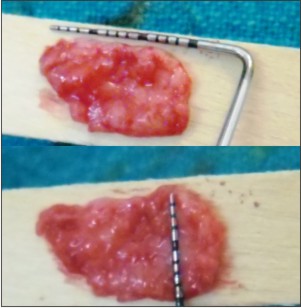 | Fig. 9 SCTG obtained measuring 15mm length and 10mm wide
 |
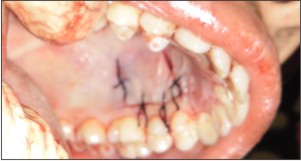 | Fig. 10 Suture at donor site
 |
SCTG was placed (Fig.11) and after recipient vascular bed preparation byperforating interdental bone, in the mid apical area adjacent to the recession as well as from the periosteal connective tissue bed apical to the recession and secured in the recipient site first followed by coronal advancement of pedicle flap sutured together in the apical 1/3 rd area and placed over the graft using catgut 4-0 absorbable sutures (Fig.12) Periodontal dressing was applied. The post operative instructions and medications were advised. Sutures were removed from donor site after 10 days whereas periodontal dressing was changed once at weekly intervals for the next 2 weeks (Fig.13). Maintenance therapy was performed at 15 days interval for 3 months. Post operative follow up was done at 1, 3 (Fig.14) and 9 months interval (Fig.15). 100% root coverage was obtained with gain in 9 mm clinical attachment , 6mm width of attached gingiva at the buccal aspect of 12 (Fig.16) with 1 mm probing depth w.r.t 11,12,13 without clinically visible CEJ . Patient was highly satisfied with aesthetic and functional outcome.
 | Fig. 11 SCTG placement at recipient site
 |
 | Fig. 12 SCTG immediately after flap closure
 |
 | Fig. 13 Post operative after 2weeks
 |
 | Fig. 14 Post operative at 3 months
 |
 | Fig. 15 Post operative view at 9 months
 |
 | Fig. 16 Post operative view presenting width of attached gingiva
 |
Discussion
MTR and its corollary, root exposure, may result in several undesirable sequelae but above all undesirable aesthetic seems to be the most common complaint which dictate the patient to seek periodontal treatment. The most commonly used classification system for MTR was proposed by Sullivan and Atkins (1968), Miller’s (1985)[3] but Miller’s classification instead of being comprehensive and simple have few draw backs one of which was it does not mention any objective criteria for assessing the severity of hard tissue or soft tissue loss in the Miller class III and IV recession which was well described by mahajan modification of Miller classification [2].
Various treatment modalities have been proposed for the root coverage in the literature but out of all the SCTG not only provide predictable percentage of root coverage4with excellent esthetic outcome but also enhance new attachment [5].
Multiple research on tetracycline root conditioning histologically demonstrates the exposure of dentin collagen, regulate the absorption of plasma proteins thereby enhancing the adhesion of blood clot[6], facilitating the deposition of cementum by inducing mesenchymal cells in the adjacent tissue to differentiate into fibroblasts[7] and also suppress the epithelial cell attachment and thereby preventing the epithelial down growth[8].
According to the systematic reviews by Rocuzzo et al (2002) and Oates et al (2003)coronally advanced pedicle flaps with connective tissue grafts results in significantly greater root coverage compared to guided tissue regeneration[3]. In the present case report, a synchronized combination of three barrier techniques in single stage surgery was utilized for Mahajan modification of Miller’s class III MTR demonstrate excellent outcome at 9 month post operatively and result isin accordance with previous literature[9] where only partial recession coverage was achieved in Miller class III defects, regardless of the technique performed[10]. Further randomized clinical trials with a larger population must be conducted to further evaluate the success of the technique employed for such defects.
References
1. Allen AL. Use of the supraperiosteal envelope in soft tissue grafting for root coverage. I. Rationale and technique. Int J Periodontics Restorative Dent. 1994 ;14:216–227.
2. Mahajan A. Mahajan modification of miller’s classification for gingival recession. Dental Hypotheses. 2010;1:45–50.
3. Lang N.P, Lindhe J. Clinical periodontology and implant dentistry. 5th ed. Blackwell Munksgard (UK) ; 2008: 958.
4. Caffesse RG, De Larosa M, Garza M, Munneravers A, Mondragon JC, Weltman R. Citric acid demineralization and subepithelial connective tissue grafts. J Periodontol. 2000;71:568-72.
5. Goldstein M, Boyan BD, Cochran DL,Schwartz Z. Human histology of new attachment after root coverage using subepithelial connective tissue graft. J Clin Periodontol. 2001; 28 (7):657-62.
6. George JP, Prabhuji MLV, Shaeesta KB, Lazarus F. Fibrin glue application in conjunction with tetracycline hydrochloride root conditioning and semilunar coronally repositioned flap in the treatment of gingival recession.J Indian Soc Periodontol. 2011; 15(1): 74–79.
7. Wikesjö UM, Baker PJ, Christersson LA, Genco RJ, Lyall RM, Hic S, et al. A biochemical approach to periodontal regeneration: tetracycline treatment conditions dentin surfaces. J Periodontal Res. 1986; 21(4):322-9.
8. Lang N.P, Lindhe J. Clinical periodontology and implant dentistry. 5th ed. Blackwell Munksgard(UK).2008:808.
9. Aroca S, Keglevich T, Nikolidakis D, Gera I, Nagy K, Azzi Ret al. Treatment of class III multiple gingival recessions: a randomized-clinical trial. J Clin Periodontol.2010; 37(1):88-97.
10. Zucchelli G, Cesari C, Amore C, Montebugnoli L, De Sanctis M. Laterally moved, coronally advanced flap:a modified surgical approach for isolated recession-type defects. J Periodontol. 2004;75 (12): 1734– 41.
|