Introduction
Gingival pigmentation is mostly caused by the physiologic deposition of melanin by melanocytes mainly located in basal & suprabasal cell layer of epithelium. [1],[2] Gingival hyper pigmentation is seen as a genetic trait in some populations irrespective of the age and gender hence termed physiologic or racial gingival pigmentation.[3],[4] The degree of Gingival Melanin Pigmentation varies from individual to individual but directly related to the Melanoblastic activity,[5] High level of oral melanin pigmentation usually is encountered among African, East Asian or Hispanic Ethnicity [6],[7], as well as in certain medical diseases like Addison’s disease, Peutz-jegher’s syndrome ,Neurofibromatosis , Antimalarial therapy, Heama chromatosis, chronic pulmonary diseases etc.[8] In dark skinned individuals, increased melanin production in skin , gingiva & oral mucosa occur as a result of genetically determined hyperactivity of melanocytes as compared to light skinned individuals.Past studies have shown that no significant difference exists in the density of melanocytes between light and dark skinned individuals. However, melanocytes of dark skinned individuals are uniformly highly reactive than the light skinned individuals.[9]
Melanin pigmentation of gingiva most often is physiological rather than pathological. Although patient complains of “black gums” which may pose aesthetic problems & embarrassment, especially in patients who are smile conscious, with a “gummy smile” or with excessive gingival display.[10],[11] Gingival depigmentation is a periodontal plastic surgical procedure where by the gingival hyper pigmentation is removed by various techniques but the results of these techniques are almost similar. One of the earliest & still most accepted techniques is surgical removal of undesired gingival pigmentation with scalpel.[12]
The case series presented here employed surgical (scalpel) excision technique for the management of gingival melanin pigmentation exclusively for esthetic purpose. Technique is simple, versatile & cost effective and does not require sophisticated instrument or apparatus but still providing satisfactory outcome.
Case Report 1
A young female patient age 17 years reported in the department of Periodontics & Oral Implantology, with a chief complaint of “Brownish black gums” that esthetically interfered with her smile (Fig.1). Patient requested for a Cosmetic therapy which will improve the esthetics on smiling. In general, skin pigmentation correlates with gingival melanin pigmentation[13], but in this specific patient gingival melanin pigmentation was observed on the anterior labial surface that moderately predominated over the skin pigmentation. Patient’s clinical & medical history confirmed that the pigmentation was Physiological.On clinical examination, gingiva was found healthy state & free of any visible clinical inflammation. Thus, bearing in mind patient’s chief complaint, a surgical gingival depigmentation procedure with the help of scalpel was planned. The procedure was explained verbally to the patient in clear and simple language, after which the patient signed the informed consent form.
 | Fig.1. Patient With “Brownish Black Gums”
 |
Surgical Procedure:- Thorough medical history was taken & routine investigations were carried outto rule out any surgical contraindication. Following the administration of local anesthetic solution (2 ml of Lignocaine with adrenaline in the ratio 1:100000 by weight)the following surgical steps were carried out.
Step. 1 A Vertical split thickness incision was given from the most apical area of gingival pigmentation i.e 1-2mm coronal to mucogingival junction & directed coronally towards the marginal gingiva 0.5-1mm short of base of gingival sulcus .(Fig.2)
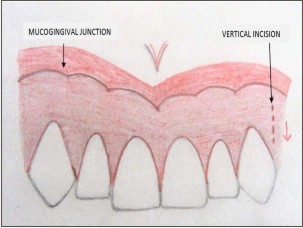 | Fig.2. Vertical Split Thickness Incision
 |
Step. 2 A Horizontal split thickness incision was given from .5 -1mm apical to the base of gingival sulcus following the gingival scalloping meeting the first incision. (Fig.3)
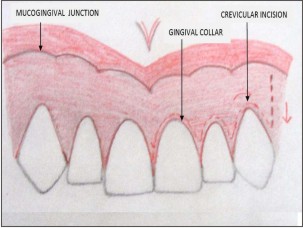 | Fig.3. Horizontal Split Thickness Incision
 |
Step. 3 A split thickness flap was raised to remove entire pigmented gingival epithelium along with a thin part of underlying sub epithelial connective tissue with the help of no. 11 & 12 scalpel blades. This removed the all the remnants of the melanin pigment in the connective tissue to prevent possible relapse of the problem.(Fig.4)
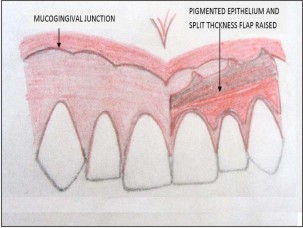 | Fig.4. Periodontal Flap Raised To Remove Epithelium And Part Of Underlying Connective Tissue
 |
Step. 4 Gingival Shaving was carried out around the Preserved gingival colar with the help of Kirkland knife.
Step. 5 Periodontal pack was applied over the surgical site to prevent post operative discomfort as well as excessive granulation tissue formation during healing.
Post operative instruction, including analgesics, antibiotic were prescribed to the patient (Ibubrofen, Amoxycillin 500mg × thrice day for 3 days) . Chlorhexidine mouth rinse (0.2%) was advised to the patients for 2 weeks immediate post operative phase to aid in plaque control.
The surgical site healed well and uneventfully in 1 week without any post operative complication.
(Fig.5)The gingiva appeared pink, firm & healthy after 4 weeks (Fig.6). On follow up at 5 month gingiva represent no reoccurrence of gingival melanin pigmentation. (Fig.7) The Patient was very impressed with pleasing esthetic outcome.
 | Fig.5. Healing After 1 Week
 |
 | Fig.6. Healing After 4 Weeks
 |
 | Fig.7. No Recurrence After 5 Months
 |
Case Report 2
A young male patient aged 20 years complained of dark colour gums.(Fig.8) On clinical examination periodontium was healthy with high frenal attachment. So, after phase I therapy same surgical procedure was carried out initially, followed by a frenectomy. Instructions & medical prescription were given to the patient. Healing was uneventful after 1 week (Fig. 9). Patient was recalled after 2 weeks (Fig.10) and followed upto 5 months with no evidence of Gingival repigmentation. (Fig.11)
 | Fig.8. Patient With Dark Colored Gums
 |
 | Fig.9. Healing After 1 Week Of Surgery
 |
 | Fig.10. Healing After 2 Weeks Of Surgery
 |
 | Fig.11. No Recurrence After 5 Months
 |
Case Report 3
A 22 years young female patient had a chief complaint of unaesthetic gingiva. (Fig.12) Patient’s history was non contributory same surgical depigmentation treatment carried out in this patient. At 5 months follow up patient had a pleasing esthetic outcome without any clinical melanin repigmentation (Fig.13).
 | Fig.12. Patient With Unaesthetic Gingiva
 |
 | Fig.13. Esthetic Outcome After 5 Months Of Surgery
 |
Case Report 4
A Young female patient age 30 years reported to the department with complaint about dark lower & upper gums (Fig.14). Same surgical technique described was carried out in mandibular anterior segment in this patient (Fig.15). Gingival healing was good at 1week post operatively.(Fig.16)
The patient was followed up to 5 months with no evidence of reoccurrence. (Fig.17)
 | Fig.14. Patient With Dark Anterior Gums
 |
 | Fig.15. Surgical Site In Mandibular Anterior
 |
 | Fig.16. 1 Week Post Operative Healing
 |
 | Fig.17. Healing After 5 Months
 |
Discussion
Different gingival depigmentation techniques have been tried in the past but all provide an almost similar outcome. Selection of depigmentation procedure should based on clinical experience & clinician preference. One of the earliest & most popular depigmentation procedure that is still widely used is Scalpel surgery, however it causes unpleasant bleeding during and after procedure. Therefore, it is necessary to apply periodontal dressing for 7-10 days.
Scalpel Gingival Depigmentation procedure not only involve the surgical removal of gingival epithelium but also the part of underlying connective tissue & leave exposed connective tissue for healing by secondary intention. The new epithelium that forms is devoid of melanin pigmentation.
Electrosurgeryhas its own limitations. Repeated & prolong use induces heat accumulation and undesired tissue destruction. Cryo surgery & Chemical cauterization is followed by considerable swelling and it is also accompanied by increased soft tissue destruction as the depth of penetration cannot be controlled.
Free gingival graftcan also be used for elimination of gingival pigmented area.However, it requires an additional surgical site (donor site) and color matching. Furthermore, the presence of a demarcated line commonly observed around the graft in the recipient site may itself pose an esthetic problem.
Nowadays LASER is widely used in Contact & Defocused mode respectively for gingival depigmentation procedure with documented advantages including less bleeding, reduced post operative pain & no requirement of periodontal dressing. Due to this reason LASER is being preferred by some clinician over the scalpel surgery but it is highly expensive, sophisticated equipment & technical expertise is required. No scientific evidence of early wound healing is documented till date with laser.
Among the above mention techniques, we found Scalpel excision technique relatively simple, versatile which required minimum time & effort.
Conclusion
The present Case Series concluded that Surgical (scalpel) excision technique for the treatment of moderate Gingival melanin pigmentation provide excellent results in term of improving esthetic & cosmetic appearance. Patients were satisfied with the outcome, which is the ultimate goal of the any therapy that is carried out. Further, at 5 month follow up no evidence of repigmentation of gingiva observed.
References
1. Dummett CO. Overview of normal oral pigmentations. J Indian Dent Assoc.1980;59(3):13-18.
2. Martini FH, Timmons MJ. Human Anatomy. New Jersey: Prentice Hall Publishers Company, 1995.
3. Dummett, C.O: Oral pigmentation. First symposium of oral pigmentation. J Periodontol 1960;31:356
4. DummetCO, Barens G. Oromucosal pigmentation: an updated literary review. J Periodontol. 1971;42(11):726-36.
5. Perimutter S, Tal H. Repigmentation of the gingiva following surgical injury. J Periodontol. 1986 Jan;57(1):48-50.
6. Fry L, Almeyda JR. The incidence of buccal pigmentation in caucasoids and negroids in Britain. Br J Dermatol1968;80(4):244-247.
7. Tamizi M, Taheri M. Treatment of severe physiologic gingival pigmentation with free gingival autograft. Quintessence Int1996;27(8):555-5
8. Leston JM et.al. Oral mucosa: variation from normalicy, partII. Cutis2002;69(3):215-17.
9. Szako G, Gerald SB, Pathak MA and Fitz Patrick TB. Racial differences in the fate ofmelanosomes in humanepidermis. Nature 1969;222:1081.
10. DummettCO, Sakumura JS, Barens G.The relationship of facial skin complexion & oral mucosa pigmentation and tooth color. J Prosthet Dent 1980;43(4):392-396.
11. Hoexter DL. Periodontal aesthetics to enhance a smile. Dent Today 1999;18(5):78-81.
12. Roshna T, Nandakumar K. Anterior Esthetic Gingival Depigmentation and Crown Lengthening: Report of a Case. J Contemp Dent Pract 2005;(6)3:139-147
|