Introduction
Odontogenic cysts can be of inflammatory or odontogenic origin[1].Till 1971 classification of World Health Organization, jaw cyst of inflammatory origin included only one variety which was radicular cyst.[2] But in 1970 Main reported a new variant of inflammatory jaw cyst which he referred to as “Inflammatory Collateral cyst”.[3] He reported eight cases of same out of which seven were related to mandible third molar, which was also descried by Conklin as “hidden cyst.”[4] Later in 1976 Craig also reported a similar cyst and named as “Paradental cyst”. He reported a series of 49 cysts which he said were found on the buccal & distal aspect of partially erupted mandibular third molar associated with pericoronitis.[2] In 1983 Stoneman & Worth described a new variety of inflammatory jaw cyst which he referred as “ mandible infected buccal cyst-molar area”. These lesions were generally found on the buccal surface of mandibular first molar in young children.[2] Eventually, second edition of WHO classification of odontogenic tumours included these cysts as separate entity .The nomenclature given to such cyst was “Paradental cyst” (Inflammatory Collateral, Mandibular Infected Buccal ) cyst.[5]
Pathogenesis of these cysts is uncertain but still it is believed that they have a strong inflammatory component. Small enamel projection into the bifurcation area of roots on the buccal aspect of the teeth has been considered as the culprit for the same by many authors.[6],[7],[8] Extension of the enamel into the bifurcation area may be instrumental in the development of the cyst by acting as stagnation area which triggers bone destruction.[9] The origin of the lining is believed to be from the reduced enamel epithelium over the cell rests of malassez as the source of epithelium.[4]
Radio graphically they usually presented as well defined radiolucency’s super imposed on the roots of affected teeth.[5] Clinically most of the lesion were found on the buccal and distal aspects of partly erupted mandibular 3rd molars the history of pericoronitis.[2] Clinically the cyst is usually infected although the tooth is vital.[1]
Here we present two cases of patients with partially erupted mandibular 3rd molars with the diagnosis of atypical odontogenic cyst and histological features of paradental cyst.
Case Report
In our first case, a 23 year old female reported with the chief complaint of pain and swelling with respect to her right mandibular 3rd molar for past few days for which she was under medication from a local dentist. On clinical examination firm ovoid swelling of approximately 5cm diameter was seen on right mandibular angle region extra-orally & intra-orally a partially erupted tooth with pericoronitis was seen. The orthopantomogram (OPG) showed a well defined ovoid radiolucency extending from the cervical region of the distal root of the 3rd molar up till the distal cusp (FIGURE 1.). The radiolucency was about 12mm x 6mm.
 | Figure 1. Panormic Radiograph Shows Unilateral Radiolucency Associated With Lower Right Third Molar.
 |
Patient underwent the surgical treatment under local anaesthesia. Buccal mucoperiosteal flap was raised with Ward’s I incision, after a little buccal bone cutting tooth was elevated out. On doing so, a cystic lesion was found attached to the distobuccal surface of the tooth which was also enucleated and sent for histopathological examination.
Histopathological examination of the lining revealed a scanty, distrupted, non-keratinized stratified squamous epithelium. The superficial cystic capsule was densely infiltrated with chronic inflammatory cells. The deeper cystic capsule was made up of condensed collagen and exhibited numerous chronic inflammatory cells (FIGURE 2).
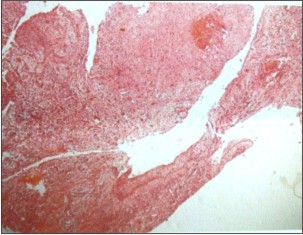 | Figure 2. Histologic Features Of The Cystic Lining Showing Non-keratinized Stratified Squamous Epithelium With Chronic Inflammatory Cells.
 |
Our second case a 25 year old female, presented with the history of swelling on left side of her mandible since past 6 months which usually subsided after taking medications. When the patient reported to us she had swelling in the same region with superadded infection due to which she had trismus.
On extra-oral examination an ovoid swelling of approximately 3cm x 4cm was seen which was tender on palpation on the left mandibular angle region.
Intra-orally a partially erupted third molar with pericoronitis with pus oozing out. Patient was put on I.V antibiotics and was operated for her impacted third molar on the third day after mouth opening improved. The orthopantomogram (OPG) showed a well defined ovoid radiolucency of approximately 2cm x 3cm, extending from apical third of the distal root of the 3rd molar involving angle region up to the mesial cusp of the involved tooth (FIGURE 3).
 | Figure 3. Panormic Radiograph Shows Radiolucency Associated With Left Mandibular Third Molar Region.
 |
Patient underwent the surgical treatment under local anaesthesia. Buccal mucoperiosteal flap was raised with Ward’s I incision, after a little buccal bone cutting tooth was elevated out. On doing so, a cystic lesion was found attached to the mesiobuccal surface of the tooth involving both the roots also which was also enucleated and sent for histopathological examination.
Histopathological examination of the lining consisted of a lumen lined with non-keratinized stratified squamous epithelium. Focal aggregates of chronic inflammatory cells were observed in adjacent fibrous connective tissue. (FIGURE 4).
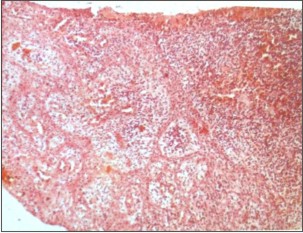 | Figure 4. Histologic Features Of The Cystic Lining Showing Numerous Chronic Inflammatory Cells.
 |
Discussion
The review of literature showed that paradental cyst is accepted inflammatory odontogenic cyst that arises in association with partially erupted vital mandibular 3rd molars with history of pericoronotis.[9] the most common site of paradental cyst is the area of mandibular molars, generally the 3rd molars.[7],[8],[9]
Many hypothesis has been postulated regarding origin of cyst. Previously it was said that cyst could have originated from 1) dental follicle, 2) cell rests of Malassez, 3) reduced enamel epithelium,4) crevicular epithelium.[1] The most accepted being one proposed by Craig and Robert[10] that reduced enamel epithelium over the enamel spur in furcation of the roots proliferates and undergoes cystic degeneration in response to inflammatory response.
The literature showed that a positive electric pulp test as a diagnostic criteria for paradental cyst. If the associated tooth is nonvital the diagnosis could be lateral radicular cyst.[2],[11],[12] However, the electric pulp testing was not done in all the cases reported. The vitality of the tooth should not be the diagnostic criteria for paradental cyst.[1]
The relation between paradental cysts and dentigerous cysts is worth discussion, because these lesions may be confused when seen in radiographs. Shear described different radiological variation of dentigerous cyst : a circumferential type where the entire tooth appears to lie within the cyst ; a central type enveloping the crown of the affected tooth symmetrically; a lateral type commonly seen when an impacted mandibular 3rd molar is partially erupted so that its superior aspect is exposed.[13] The presence of Colgan’s sign which is the preservation of the distal follicular space in a radiograph is useful diagnostic feature to distinguish paradental cyst from dentigerous cyst.[4] In our case report the paradental cysts appeared as a well- delineated radiolucency associated with the root of the affected teeth extending up the crown area.
The relation between angulation of tooth impaction and location of cyst has also been given significant criteria in the development of the cyst. It is believed that food is deflected by the occlusal surface of the lower 3rd molar during chewing, so that it is forced into the gingival soft tissues around the crown of the tooth. The direction of deflection is dependent on the angulation of the tooth to the occlusal plane. In mesioangular impacted tooth, food is forced into the space between the distal surface of the 2nd molar and the occlusal surface of the 3rd molar. In contrast to the vertical or distoangular impactions, the vulnerable area for development of a cyst seems to be on the buccal and distal or distobuccal aspects respectively. Other anatomic factors such as crown form, fissure pattern, adjacent teeth, and gingival pattern also influence the location of the cyst.[4]
Most reports agreed with the treatment choice of enucleation of the cyst followed by extraction of the associated tooth if the tooth is 3rd molar.[3],[10],[14],[15] however the tooth involved is 1st or 2nd molar enucleation of the cyst without extraction of the tooth is recommended.[2],[7],[16] Reccurrence of the cyst has not been reported and is not likely to occur provided the cyst has been completely removed.[9]
To conclude, paradental cyst is an inflammatory odontogneic cyst commonly associated with partially erupted vital mandibular 3rd molar with pericoronitis, grossly most commonly attached to the buccal root surface overlying the bifurcation, developmentally arising from the enamel projection seen on the buccal root surface, radiographically distinct from the traditionally described dentigerous cyst.
References
1. Lim AA, Peck RH. Bilateral mandibular cyst: lateral radicular cyst, paradental cyst, or mandibular infected buccal cyst? Report of a case. J Oral Maxillofac Surg.2002 Jul; 60(7):825-7.
2. Wolf J, Hietanen J. The mandibular infected buccal cyst (paradental cyst). A radiographic and histological study. Br J Oral Maxillofac Surg. 1990 Oct; 28(5):322-5.
3. Main DMG: Epithelial jaw cysts: A clinicopathological reap-praisal. Br J Oral Surg 8:114, 1970.
4. Colgan CM, Henry J, Napier SS, Cowan CG. Paradental cysts: a role for food impaction in the pathogenesis? A review of cases from Northern Ireland. Br J Oral Maxillofac Surg. 2002 Apr; 40(2):163-8.
5. W.c Ngeow, R.b Zain,W.L Chai.Paradental cyst associated with an unerupted wisdom tooth. Annpl Dent. Univ Malaya 2000; 7: 43-45.
6. Craig GT. The paradental cyst. A specific inflammatory odontogenic cyst. Br Dent J. 1976 Jul 6;141(1):9-14.
7. Gail Ackermann,Mark A. Cohen, M.Dent ,Mario Altini Theparadentalcyst: A clinicopathologic study of 50 cases .Oral Surgery, Oral Medicine, Oral Pathology Vol 64, Issue 3, September 1987, Pages 308–312
8. Poul Vedtofte, Finn Praetorius, The inflammatory paradental cystOral Surgery, Oral Medicine, Oral Pathology Volume 68, Issue 2, August 1989, Pages 182–188
9. 9.raig B. Fowler, MAJ, USAF, DC Robert B. Brannon, COL, USAF, DCThe paradental cyst: A clinicopathologic study of six new cases and review of the literature Surgery, March 1989, Pages 243–248
10. Craig B, Robert BB: The paradental cyst: A clinicopathologic study of six new cases and review of the literature. J Oral Maxillofac Surg 47:243, 1989
11. Stoneman DW, Worth HM: The mandibular infected buccal cyst-molar area. Dent Radiogr Photogr 56:1, 1983
12. Martinez-cone R, Aguirre JM: Paradental cyst of the second molar: Report of a bilateral case. J Oral Maxillofac Surg 53: 1212, 1995
13. Craig GT: The paradental cyst. A specific inflammatory odon-togenic cyst. Br Dent J 141:9, 1976
14. Vedtofte P, Praetorius F: Recurrence of the odontogenic ker-atocyst in relation to clinical and histological features: A 20-year follow-up study of 72 patients. Int J Oral Surg 8:412, 1979
15. Packota GV, Hall JM, Lanigan DT, et al: Paradental cysts on mandibular first molars in children: Report of five cases. Den-tomaxillofac Radiol 19:126, 1990
16. Wolf J, Hietanen J: The mandibular infected buccal cyst (para-dental cyst): A radiographic and histological study. Br J Oral Maxillofac Surg 28:322, 1990
17. Ackermann G, Cohen MA, Altini M: The paradental cyst: A clinicopathologic study of 50 cases. Oral Surg Oral Med Oral Pathol 64:308, 1987.
18. Martinez-cone R, Aguirre JM: Paradental cyst of the second molar: Report of a bilateral case. J Oral Maxillofac Surg 53: 1212, 1995.
|