Introduction
In the past, various treatment modalities have been attempted to enhance the periodontal regeneration. Recently, a synthetic biomimetic hydroxyapatitexenograft, PEPGEN-P15®*,has been demonstrated to promote the bone formation. It is one among the many materialsto mimic autogenous bone,as 15 amino acid sequence of Type I collagen(P-15 peptide) coats the surface of anorganic bone mineral (ABM).[1] P-15 peptide has steric similarities to the cell binding site of type-I collagen present in the bone.
Another recent approach, for periodontal regeneration is the use of polypeptide growth factors, known to promote proliferation and migration of periodontal ligament cells, synthesis of extracellular matrix as well as differentiation of cementoblasts and osteoblasts.Platelet-rich fibrin (PRF), a second-generation platelet concentrate (PC), originally described by Choukroun et al,[2] is a safe and convenient approach to deliver high concentrations of polypeptide growth factors. PRF can beobtained by gentle centrifugation of peripheral blood, not requiring the addition of any anticlotting agent, which renders its preparation less chaotic. Dohan Ehrenfest et al[3] showed that approximately 97% of platelets and 50% of leukocytes of the original blood volume were concentrated and three dimensionally distributed in the PRF clot, that is believed to release polypeptide growth factors, such as transforming growth factor-β1, platelet- derived growth factor, vascular endothelial growth factor and matrix glycoproteins (such as thrombospondin- 1), in a sustained fashion for at least 7 days, as shown in vitro.3 PRF also shows positive effects like “Jump-starts” the cascade of osteogenesis in a bone graft, facilitates graft stabilization, promotes early consolidation of the graft, speeds up mineralization and finally improves trabecular bone density.[2]
Hence, the present case series, reveals a clinical and radiographic evaluation of, PEPGEN-P 15,when used in combination with PRFin the treatment of periodontal intrabony defects with the primary outcome variables being the linear bone growth and defect volume gain, as evaluated using a high resolution spiral computed tomography (CT) scan.
Clinical Presentation
Three patients (two male and one female, aged 25 to 35 years) diagnosed with generalized chronic periodontitis, having intrabony defects at teeth sites #20 mesial ,#21distal and #30 mesial, with radiographic evidence of bone loss (Fig.2), were treated in the Department of Periodontology & oral Implantology, Maharishi Markandeshwar College of Dental Sciences & Research, Mullana, Haryana, India from January 2012 to March 2012. The patients were systemically healthy,nonsmokersand reported no known drug allergies and no current medications. Phase I therapy was performed. Volumetric analysis of the defect sites was done, by acquiring three-dimensional CT scan images, using a multidetector 64-slice CT scan machine†, aided by Dentascan software. Clinical parameters in all three patients, including: 1) pocket probing depth (PD) >5mm; 2) Relative clinical attachment levels (RAL) >10mm; and 3) Relative position of gingival margin (PGM) (mid-facial), were recorded immediately before surgery (as baseline), at 6 and 9 month intervals. A millimeter graded periodontal probe‡with acrylic stent as reference point was used for measurements. (Fig.1a)
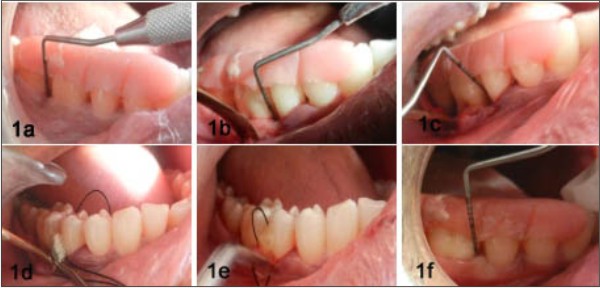 | Figure 1. Surgical procedure A: Preoperative #30; B, C: Intraoperative measurements taken at intrabony defect site #30 after Open-flap debridement; D: Placement of PEPGEN P-15 graft; E: Placement of PRF; F: 9 month postoperative PD was reduced to 3 mm
 |
 | Figure 2. Intraoral periapical rediographs #30; A: Preoperative (baseline); B: 6 months postoperative; C: 9 months postoperative
 |
Case Management
Prior to the procedures, written informed consent was obtained from all patients. The procedures followed were in accordance with the ethical standards of the University Ethical committee on human experimentation and with the Helsinki Declaration of 1975, as revised in 2000. A conventional open flap debridement surgery in the respective quadrant, along with placement of Pepgen-P15 in combination with PRF within the intrabony defect sites was done(intrabony component of >3mm, Fig. 1b through 1e). Interrupted sutures were given and a periodontal pack was placed. The patients were given postsurgical instructions and advised to rinse with 0.12% Chlorhexidine mouth rinse twice daily for 1 week. A prescription of systemic antibiotics (500 mg amoxicillin, every 8 hours for 5 days), and analgesics (400 mg ibuprofen, every 8 hours for 5 days) was provided.
Results
At 6 and 9 month follow-up examination, it was observed that PD reduced in range of 3 to 5 mm with 1 to 2 mm coronal shift in PGM and again in CAL of 2 to 5 mm (Table 1).
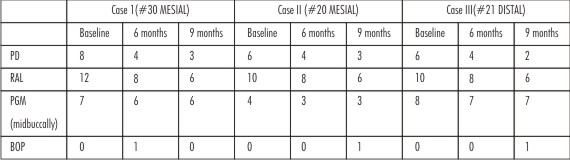 | TABLE 1 Clinical Parameters at Baseline and 6 and 9 months postoperative (mm)
 |
A three-dimensional (3D) reconstructed Dentascanimages acquired at 9 month interval, confirmed positive changes in the defect morphology, with a linear bone growth of 1.5-3mm( 33 to 37 %).The volumetric analysis showed a bone fill of 55 to 81% at the defect sites (Table 2, Figs. 3 through 4).
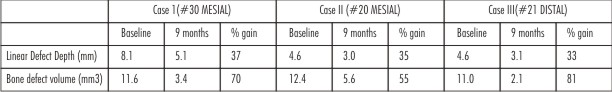 | TABLE 2 Radiographic Parameters at Baseline and 9 months postoperative
 |
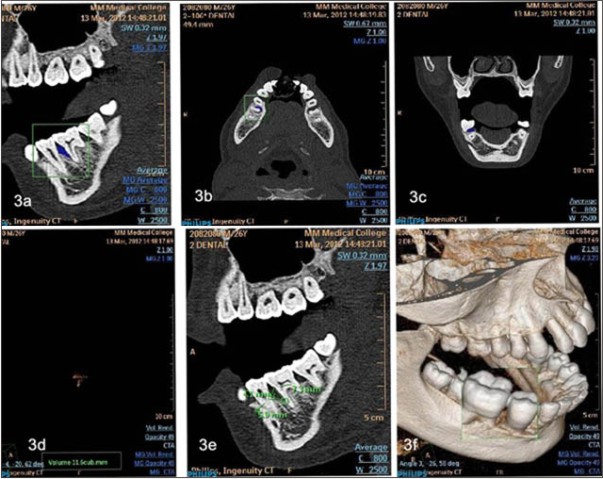 | Figure 3. Preoperative Dentascan Images. A: saggital section; B: axial section; C: coronal section; D: defect volume obtained; E: linear bone defect measurements; F: 3D Reconstructed model
 |
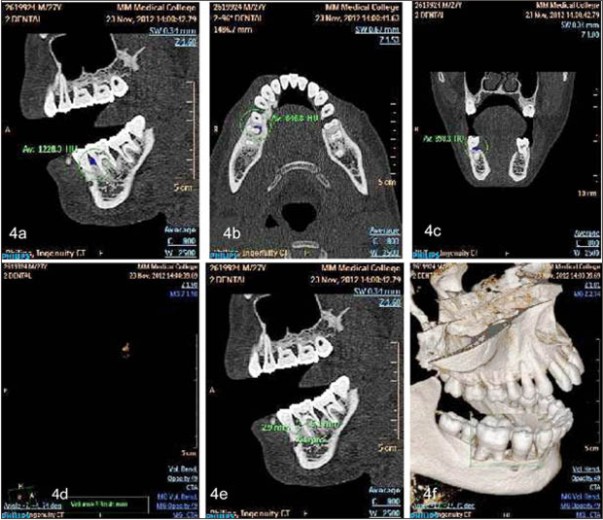 | Figure 4. Postoperative (9 months) Dentascan Images. A: saggital section; B: axial section; C: coronal section; D: defect volume obtained; E: linear bone defect measurements; F: 3D Reconstructed model
 |
Discussion
The in vitro studies by Bhatnagar et al [1], Yuan et al[4] and in vivo studies by Yukna et al [5] have shown the efficacy of ABM/P-15(Pepgen-P15) to promote attachment of periodontal ligament fibroblasts and provide better bone healing than ABM alone.
The present case series demonstrates that platelet rich fibrin, and xenograft Pepgen-P15 enhances the clinical and the radiographic outcome in regeneration of intrabony osseous defects, as observed in the clinical studies by Pradeep AR et al and Lekovic V et al, indicating that PRF in combination with bone grafts like hydroxyapatite or bovine porous bone mineral, can significantly improve the regenerative effects within intrabony periodontal defects.[6],[7] The use of combination of Platelet rich fibrin with bone graft was more beneficial, as two distinct wound healing processes results in their synergistic effect.[8] Also, in present case series, a 3-dimensional volumetric analysis using Computed tomography (CT) has been introduced, to overcome the difficulties caused by the nature of conventional radiography.[9] Recently, multi-slice Spiral tomography has replaced conventional Computed tomography. Dentascan, a dental computed tomography software program, is an extension of Computed tomography technology, which improves specificity and sensitivity over standard imaging.[10] The limitation to the use of CT scan is, it being an expensive mode of radiographic assessment, along with higher amount of radiation exposure than conventional IOPAs.
Conclusions
The autologous mode of obtaining PRF is cost effective and less chaotic.To the best of our knowledge, use of PRF along with PEPGEN P-15 in the regenerative treatment of periodontal intrabony defects in humans, has not been previously reported.Also a new technique of volumetric analysis using DENTASCAN has been introduced here.
Acknowledgments
Authors wish to acknowledge Dr. Amita Aggarwal, MDS, Reader, Dr. Shalu Bathla, MDS, Reader, Dr. Deepak Kochar, MDS, Reader, Dr. Anish Manocha, MDS, Senior Lecturer, M.M.C.D.S.R., Mullana, for their help in manuscript preparation. The authors report no conflicts of interest related to this case series.
References
1. Qian JJ, Bhatnagar RS. Enhanced cell attachment to anorganic bone mineral in the presence of a synthetic peptide related to collagen. J. Biomed. Mater. Res.1996; 31: 545–554
2. Choukroun J, Adda F, Schoeffler C, Vervelle A. Uneopportunite en paroimplantologie : l PRF. Implantodontie 2001; 42:55-62. (French).
3. Dohan Ehrenfest DM, Del Corso M, Antoine D, Mouhyi J, and Baptiste Charrier J. Three-Dimensional Architecture and Cell Composition of a Choukroun’s Platelet-Rich Fibrin Clot and Membrane. J Periodontol 2010; 81:546-555.
4. Yuan K, Huang JS, Hsu CW, Hung IJ. A mineralization-associated membrane protein plays a role in the biological functions of the peptide-coated bovine hydroxyapatite. J Periodont Res 2007; 42: 420–428
5. Yukna RA, Krauser JT, Callan DP, Evans GH, Cruz R, Martin M. Multi-center comparison of combination anorganic bovine-derived hydroxylapatite matrix (AMB)/cell binding peptide (P-15) and ABM in human periodontal osseous defects. J Periodontol 2000; 71:1671-1679.
6. Pradeep A R, Bajaj P, Rao NS et al.Platelet-Rich Fibrin Combined with a Porous Hydroxyapatite Graft for the Treatment of Three-Wall Intrabony Defects in Chronic Periodontitis: A Randomized Controlled Clinical Trial.[published online ahead of print March 16, 2012]. J Periodontol; doi:10.1902/jop.2012.110722
7. Lekovic V, Milinkovic I, Aleksic Z, Jankovic S, Stankovic P, Kenney EB, Camargo PM. Platelet-rich fibrin and bovine porous bone mineral vs. platelet-rich fibrin in the treatment of intrabony periodontal defects. J Periodont Res 2012; 47: 409–417
8. Toffler M, Toscano N, Holtzclaw D ,Del Corso M, Dohan Ehrenfest DM.Introducing Choukroun’s Platelet Rich Fibrin (PRF) to the Reconstructive Surgery Milieu. The Journal of Implant & Advanced Clinical Dentistry;2009,21-32
9. Hoidal MJ, Grimard BA, Mills MP, Schoolfield JD, Mellonig JT, Mealey BL. Clinical evaluation of freeze dried bone allograft with and without enamel matrix derivative for the treatment of periodontal osseous defects in humans. J Periodontol 2008; 79:2273-2280
10. Kumar PG, Kumar JA, Anumala N, Reddy KP, Avula H, Hussain SN.Volumetric analysis of intrabony defects in aggressive periodontitis patients following use of a novel composite alloplast: A pilot study.Quintessence Int 2011;42:375–384
|