Introduction
An adequate amount of bone, in both width and height is required for successful implant placement[1]. Volume & density of bone are crucial factors for implant success[2]. One of the most common anatomical limitations in oral implantology is bone atrophy of the upper maxilla[3]. In maxilla, bone width is lost primarily in facial region because the labial plate is thin as compared to the palatal plate[4]. Residual ridge shifts palatally in maxilla, at the expense of buccal cortical plate. 25% decrease in facio-palatal width occurs within first year of tooth loss and rapidly evolves into a 30% and 40% decrease within 3 years[4]. Narrow alveolar crests make implant bed preparation difficult, with the appearance of fenestrations & dehiscence of the cortical layers[3]. Depending upon the morphology of the defect various procedures for Bone Augmentation can be used like expansion osteotomes, ridge splitting, bone spreading, onlay grafts, interstitial grafts etc[1].
Expansion technique mainly consists of expanding atrophic bone crests in order to secure sufficient bone width for dental implant placement. Expansion osteotomes are used in atraumatic or indirect maxillary edentulous situations & they separate the cortical plates. This technique restores bucco-palatal dimensions without the use of grafts, with simultaneous insertion of implant at the same time. The expansion osteotomes exerts lateral compression, thereby increasing bone density and thus primary implant stability. Moreover it affords superior manual control in determining the implant axis there by contributing to avoid fenestrations & dehiscence. There is also less peri implant bone warming & less bone loss is produced during expansion[3].
The purpose of the study is to evaluate the success of the dental implants placed using bone expansion technique in bucco- palatally compromised maxilla, with the objective of studying the clinical performance of implants from baseline to nine months information in specified population of Modinagar, India.
Aim & Objectives:
To evaluate efficacy and success of implants placed with bone augmentation technique in maxilla.Implants will be evaluated clinically, radiographically and periodically.
Methodology:
This study was carried out in the department of Prosthodontics and Oral Implantology, D.J. College of Dental Sciences and Research, Modinagar. The study population comprised of total number 13 subjects comprising of 11 males and 2 females subjects aged between 20yrs to 60yrs.Total number of 20 dental implants were placed at different sites in maxilla. The participants were first informed in detail about the study, and a written informed consent was obtained from all the participants.
Subjectsfree of any pathology or deformities and with good periodontal and dental health status within the above mentioned age group were included in the study. Exclusion criteria consisted of poor oral hygiene, systemic diseases that contraindicate implant placement, chronic tobacco chewers and smokers, parafunctional habits,insufficient occlusal clearance & close proximity to vital anatomic structure . A pre-operative examination was carried out with careful evaluation of the soft and hard tissue.Assessment of interocclusal space, mesiodistal, faciopalatal, bone height and inter dental papilla was done.
Pretreatment planning included preparation of study and working cast models to record occlusal relationship as well as wax up for proposed prosthesisaAll selected patients were subjected to radiographic examination. Imaging modalities used were -Intraoral periapical radiography (IOPA), Panoramic Digital radiography (OPG) and CBCT. Radiographs revealed mesiodistal and apico-coronal dimensions of the available bone at the implant site as well as the trabecular pattern of the bone and diameter and length of the implant.
The various parameters used were as follows: Amount of Expansion achieved, Bone loss & Implant Quality Scale.
Bone expansion:Changes in the bucco-lingual width of the alveolar ridge before osteotomy preparation, at the time of implant insertion, and implant uncovery surgery using a surgical caliper were evaluated. Measurement of the width of the edentulous was taken at approximately 1 mm below the crestal margin. to the nearest 0.5mm. Alveolar ridge width measurements were repeated at uncovery (e.g. second surgery) The following parameters were evaluated: (a) preoperative width of the edentulous alveolar ridge (time to); (b) width of the alveolar ridge at the end of expansion and implant placement (time t,); (c) width of the alveolar ridge at the time of abutment connection (time t2); (d) width of the alveolar ridge 3 months after prosthetic loading (time t3). The measurements were performed with open flaps at times t0, and t1. Measurements at t3 were performed through the mucosa. to avoid reopening of the sites. with minimal patient discomfort. after the application of a local anesthetic.
Bone loss Marginal bone loss around implants after placement and loading at specific defined time intervals was assessed with peri-apical radiographs with grid. The radio graphs were repeated throughout the study and compared to detect the presence or absence of continuous peri-implant radiolucency and to determine the location of alveolar bone levels around the implants.
Implant Quality Scale (Table 1)
 | Table 1 : Implant Quality Scale, This scale was first presented by James later modified by Misch. Implants were evaluated at baseline, 3 months, 6 months ,9 months & 12 months.
 |
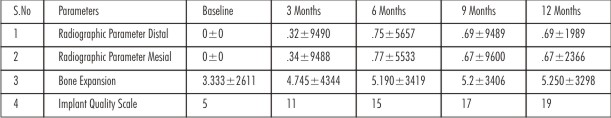 | Table 2 : mean & S.D. Of Different Dental Parameters At Different Time Points
 |
Results
The various parameters assessed were - peri implant bone levels, implant quality scale, amount of expansion achieved, an. All implants were considered for statistical analysis.
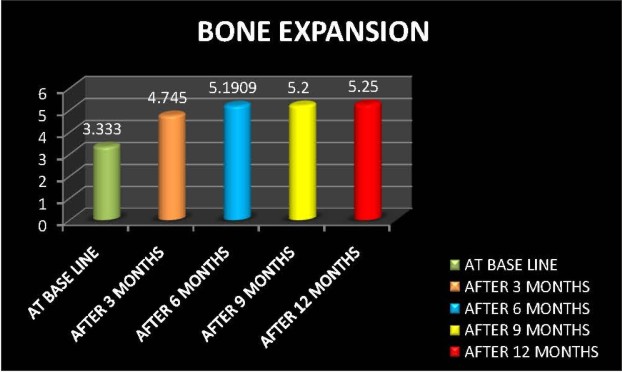
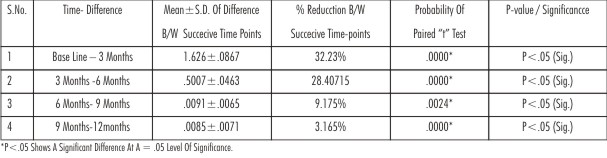
All clinical & radiographic parameter values, so obtained, were entered in the Standard performa draw for the study & subjected to statistical analysis. The arithmetic mean & standard deviations were calculated for the requisite assessment intervals & for intra & inter group comparisons. All the values of different dental parameters at different time points are expressed in terms of mean±S.D. respectively (Table 2) (Graph 1, 2A, 2B & 3). The difference from baseline to 3 months, 3 months to 6 months, 6 months to 9 months and 9 to 12 months was measured and its significance was assessed by paired‘t’ test. It showed that significant improvement /difference was observed for bone expansion and at 5%level of significance. However all the other parameters were not significant at 5%level of significance (P>.05).The application of one way ANOVA shows a significant difference among all different time points ,Further it was observed that bucco-lingual expansion of the ridge was continuously improved for different implant sites in all patients at successive time intervals.
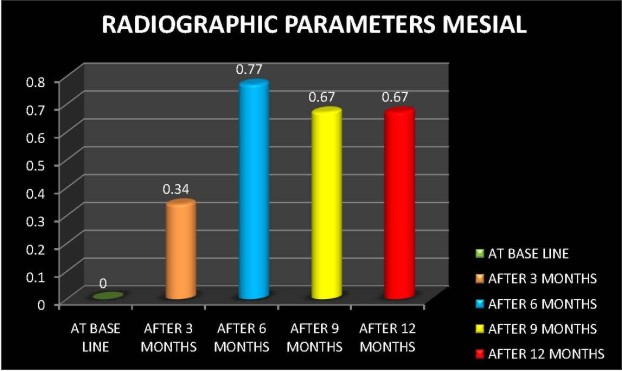
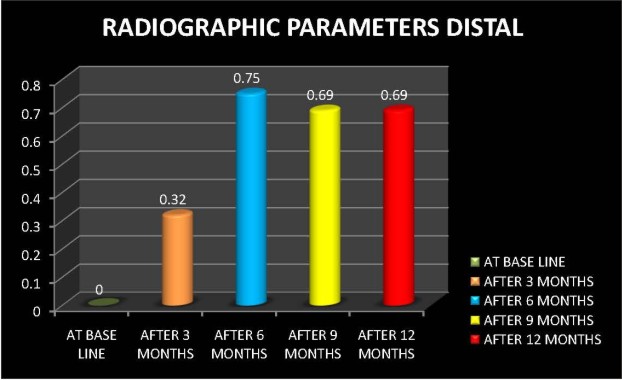
Graph 2A & 2B depicts the average amounts of alveolar marginal bone loss (distal/ mesial) of the implants at defined intervals as measured on peri-apical radiographs. The average marginal bone loss around the implants on distal side was 0±0,. 32±9490,. 75±5657,. 69±9489,. 69±1989 at baseline, 3 months, 6 months 9 months and 12 months respectively The mean differences of bone levels from the baseline to 3rd, 3rd to 6th, 6th to 9th & 9th to 12th months were-.333±1, -0.35±1.148, -0.02±.0808, -0.01±.6759 respectively. The respective ‘p’-values were .3652, .2541, .2987, .3425which were statistically not significant (p>0.05).The average marginal bone loss around the implants on mesial side 0±0, .34±9488, .77±5533, .67±9600, .67±2366 at baseline , 3 months, 6 months, 9 months & 12 months respectively The mean differences of bone levels from baseline to 3rd , 3rd to 6th,6th to 9th & 9th to 12th months were -.333±1, -0.43±1.148, 0.075±.0808, 0.025±.0789respectively. The respective ‘p’-values were .3652,.2541, .2987, .1234which were statistically not significant (p>0.05). This shows that mean bone loss was almost same on both mesial and distal sides at each time interval except for 6th month in which more amount of bone loss was observed. At all time intervals on mesial side and distal side no statistically significant differences (p>0.05) were apparent between base line and 3 months,3 months-6 months, 6 months-9 months & 9 -12 months. Upto 3 months bone loss was minimal but after loading of implants progression of marginal bone loss was observed but this was not significant.
 | Graph 1
 |
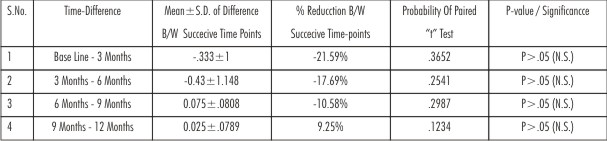 | Table 3(A) - Comparison Of Difference B/W Successive Time Points (By Paired âtâ Test) In Radiographic Parameters (Mesial)
 |
 | Graph 2A
 |
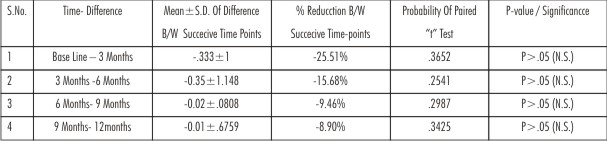 | Table 3(B) - Comparison Of Difference B/W Successive Time Points (By Paired âtâ Test) In Radiographic Parameters (Distal)
 |
The pre-operative and immediate post-surgery buccal/lingual width measurements were made using a surgical calliper(Graph 1depicts mean and S.D of bone expansion at different time points). Table 2 depicts % improvement in bucco-lingual width of ridge b/w successive time points. The average pre-operative buccal/lingual width was 3.333 ± 0.55 mm. The average post-operative buccal/lingual ridge width immediately after the ridge split procedure was 5.250 ± 0.63 mm. There was a mean total gain in buccal/lingual ridge width of 1.917mm. Maximum expansion of ridge was observed to be 83.33%increase in buccolingual width of ridge between t0-t1,t0-t2,t0-t3,t0-t4..Least amount of ridge expansion was observed to be. 42.6% just after implant placement and 57.14% at t2,t3,t4 time interval
Graph 3 and Table 1 depicts implant quality scale. At baseline 5 implants were in optimal health and by the end of 12 months 19 implants were in optimal. At 6 month 9 implants were in optimal health due to motivation of patient towards oral health but 1 implant was in compromised health i.e slight radiolucency around the crestal portion of implant was seen and implant was lost during abutment tightening and ultimately there was clinical and absolute failure of the implant.
 | Graph 2B
 |
 | Graph 3
 |
 | Table 4-Comparison Of Difference B/W Successive Time Points (By Paired âtâ Test) In Bone Expansion
 |
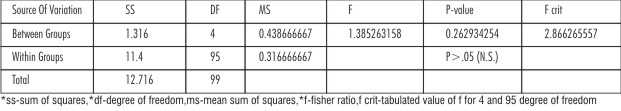 | Table 6(A) - Comparison Of Significant Difference Among Different Time Points For â Radiographic Parameters- Distal (One Way Anova)
 |
 | Table 6(B) - Comparison Of Significant Difference Among Different Time Points For â Radiographic Parameters- Meisal (One Way Anova)
 |
Discussion
Recent longitudinal studies by Behneke et al. 2000[5], Feloutzis et al 2003[6] have raised evidence-supported doubts over established criteria putting forth the observation that crestal bone loss around osseointegrated implants in well- maintained patients may be minimal. Interpretation of intraoral radiographs is one of the most frequently employed diagnostic procedures for monitoring peri-implant conditions. (Fourmousis et al 1994)[7]. Furthermore, the exploits of digital image analysis has been extended to implant dentistry to monitor peri-implant bone healing (Bragger et al. 1988)[8] In this study computer-assisted image analysis Covani U et al[9] was used for interpreting the intraoral periapical radiographs.
The radiographic bone levels were calculated on mesial and distal sites, according to the method of linear measurements, described by Bragger et al 1988[8].This method is reliable for measurements of crestal bone level changes. The implant features with design characteristics of known size facilitate radiographic measurements of crestal bone level at the proximal sites.
In this study, at baseline the mean bone levels on mesial side were 0±0as the recordings were taken one month after prosthesis placement. The mean bone levels at 3rd, 6th & 9th months were .32±.9487, .74 ±.1853&.67 ±.1989respectively. The mean differences of bone levels from baseline to 3rd, 3rd to 6th & 6th to 9th months were -.333±1, -0.42 ±1.149 & 0.07 ±.0707respectively. The respective ‘p’-values were .3434, .8003& .1934 which were statistically not significant (p>0.05).Overall findings of this present study were very similar to the studies done on SLA surface by Behneke et al 2000[5] These results also find agreement with the studies done by Canullo et al 2007.[10]
The ICOI Pisa Consensus Conference has simplified and updated a Health Scale specific for endosteal implants and included categories of success, survival, and failure. In addition, these categories of health may be related to the prognosis of the existing conditions. At baseline 60%of implants quality scale were in optimal health. 40% of implants were in satisfactory. At 3rd month readings were similar to baseline. At sixth month 90%of the implants were in optimal health due to motivation of patient towards oral health but 10% of the implant was in compromised health i.e. slight radiolucency around crestal portion of implant was seen and implant was lost during abutment tightening and ultimately there was clinical and absolute failure of implant.
In the present study the pre-operative and immediate post-surgery buccal/lingual width measurements were made using a surgical caliper. The average pre-operative buccal/lingual width was 3.333 ± 0.55 mm which was very less for implant placement using conventional technique. The average post-operative buccal/lingual ridge width after the osteotome technique was 5.250 ± 0.63 mm. There was a mean total gain in buccal/lingual ridge width of 1.90 mm. Maximum expansion of ridge was observed in 6 subjects with overall 83.33%increase in buccolingual width of ridge between t0-t1,t0-t2,t0-t3,t0-t4..Least amount of ridge expansion was observed in 5 subjects 57.14% at t2,t3,t4 time interval. In subject 14 just after implant placement 66.67%increase in buccolingual width was observed which remained constant up to 3 months but after failure of implant the amount of expansion was reduced to 50%.
The mean total gain in ridge width immediately following the osteotome technique procedure was 1.91mm in this investigation. This increase in width correlates well with other published studies. Vercellotti et al[11]did a similar study and reported averaged a gain of bone width of ~2.0 mm. Blus et al[12] performed ridge expansion in two hundred thirty implants and reported an increase in bone width ranging from 2.5 – 4.0 mm.
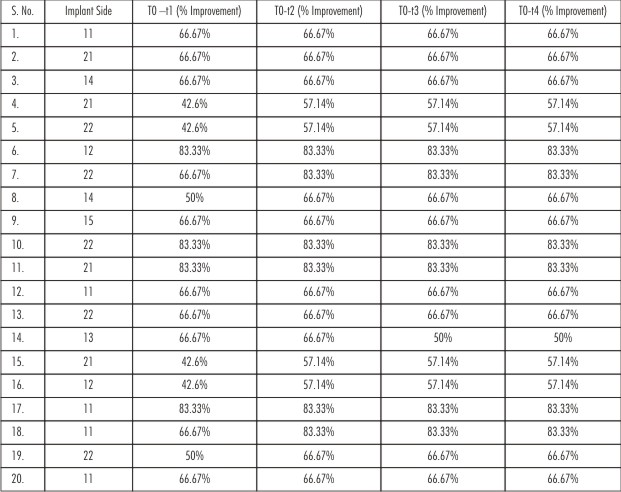 | Table 5 - % Improvement In Bucco-Lingual Width Of Ridge B/W Successive Time Points
 |
 | Fig. 1.1: Pre-operative View
 |
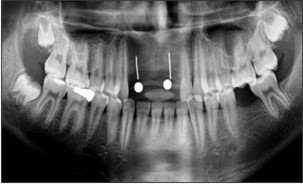 | Fig. 1.2: Pre-operative Opg
 |
 | Fig. 1.3: Elevation Of Flap
 |
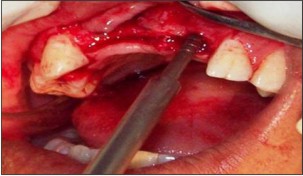 | Fig. 1.4: Expansion Of Bone With Osteotome
 |
 | Fig. 1.5: Implant Placed In 21 Region & Expansion Of Bone With Osteotome In 12 Region
 |
 | Fig. 1.6: Bio-oss Graft Placed On Labial Cortical Plate
 |
 | Fig. 1.7: Sutures Placed
 |
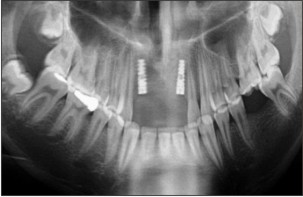 | Fig. 1.8: Post-operative Opg
 |
 | Fig. 1.9: Gingival Former Placed
 |
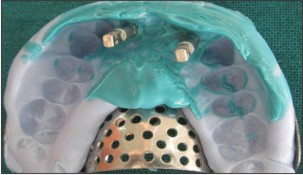 | Fig. 1.10: Putty Imprassion Taken With Transfer Coping
 |
 | Fig. 1.11: Lab Analog Transfered In Mounted Cast
 |
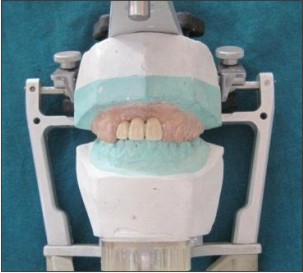 | Fig. 1.12: Final Prosthesis In Mounted Cast
 |
 | Fig. 1.13: Abutment Placed
 |
 | Fig. 1.14: Final Prosthesis Cemented
 |
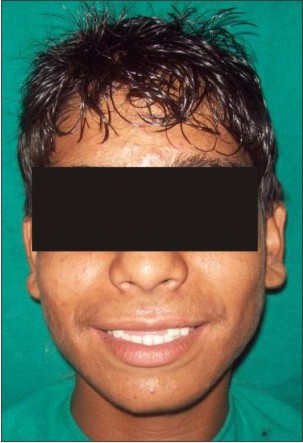 | Fig. 1.15: Pre Treatment View
 |
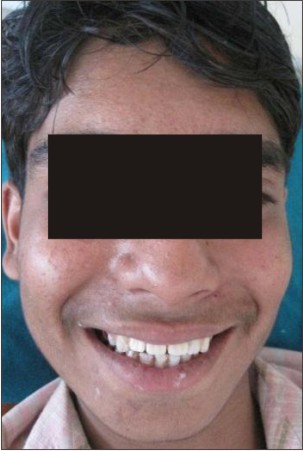 | Fig. 1.16: Post Treatment View
 |
Conclusion:
Within the limitations of this study we concluded that the indications for the use of osteotome technique should be limited to those for which it was introduced, that is, narrow ridge and for bone with less density. More clinical studies with larger samples and longer follow-up are necessary to confirm these findings. A randomized study design would be preferable to compare different augmentation techniques (i.e., guided bone regeneration and the osteotome technique). However, for comparison with conventional implant preparation, a randomized study would be impossible because deficient bone sites are not suitable for conventional implant preparation.
References
1. Silverstein LH, kurtzman GM, Moskowitz ME et al Aesthetic enhancement of anterior dental implants with the use of tapered osteotomes and soft tissue manipulation. J Oral Implantol 1999;25(1):18-22.
2. Nowzari H, Molayem S, Chiu CHK,et alCone Beam Computed Tomographic Measurement of Maxillary Central Incisors to Determine Prevalence of Facial Alveolar Bone Width 2 mm.Clinical Implant Dentistry and Related Research 2010.
3. Ferrer JR, Diago MP, Carbo JG Analysis of the use of expansion osteotomes for the creation of implant beds. Technical contributions and review of the literature. Med Oral Patol Oral Cir Buccal 2006;11:E 267-71.
4. Misch CE.Dental Implant Prosthetics. Elsevier Mosby.2005;375
5. Behneke A, Behneke N, d’Hoedt B. The longitudinal clinical effectiveness of ITI solid screw implants in partially edentulous patients: A 5 year follow up report. Int J Oral Maxillofac Implants .2000; 15: 633-645.
6. Feloutzis A, Lang NP, Tonetti MS, et al.IL-i gene polymorphism and smoking as risk factors for pen-implant bone loss in a well-maintained population. Clin Oral Implants Res .2003; 14: 10-17.
7. Fourmousis I, Bragger U, Burgin W, Tonetti M, Lang NP. Digital image processing —I. Evaluation of gray level correction methods in vitro. Clin Oral Impl Res. 1994: 5:37-47.
8. Bragger Uet al Associations between clinical parameters assessed around implants and teeth. Clin Oral Implants Res.1997 ; 8(5):412-21
9. Covani U, Barone A,Cornelini R,Crespi R Clinical Outcome of Implants Placed Immediately After Implant Removal.J Periodontol 2006; 77:722-727
10. Canullo L, Rasperini G. Preservation of periimplant soft and hard tissues using platform switching of implants placed in immediate extraction sockets; a proof of concept study with 12 to 36 month follow up. Int J Oral Maxillofac Implants. 2007:22; 995-1000.
11. Vercellotti T, Nevins ML, Kim DM, et al. Osseous response following respective therapy with piezosurgery. Int J Periodontics Restorative Dent 2005; 25:543–549.
12. Blus C, Szmukler-Moncler S. Split-crest and immediate implant placement with ultrasonic bone surgery: A 3-year life-table analysis with 230 treated sites. Clin Oral Implants Res 2006; 17:700–707
|