Introduction:
“No person should be overlooked for treatment. because of a disability”.
Everyone has the right to a standard of living adequate for the health and well being of himself and his family, including medical care and necessary social services. (The United Nations universal declaration of human rights (1948)). The above declaration makes it very clear that everyone has equal right to good health and well being, including persons with disability.
British Disability Discrimination Act (BDDA) defines Disability as a physical or mental impairment, which has a substantial and long term adverse effect on his/her ability to carry out normal day to day activities.
Children with disabilities often have a high and unmet need for dental treatment [1],[2],[3]. Linked to this need is the inescapable fact that many children with disabilities may live below the poverty margin and also have additional medical impairments that deteriorating oral health can exacerbate, or can exert an effect on the child’s quality of life [4],[5]. For many children with profound disabilities the only option for dental care is when a crisis occurs and they are hospitalized for an in-patient general anaesthetic and dental treatment is carried out[6]. Oral health care for disabled children is a health care area that has received scant attention. It is estimated that one out of two persons with a significant disability cannot find a professional resource to provide appropriate and necessary dental care. Lack of access to dental services for this growing segment of our population is reaching critical levels and is a national dilemma. [7]
Prevalence of disabled children is on the rise and is increasing at an alarming rate. In India, there are 21.9 million disabled people, which constitutes about 2.13 percent of the total population.[8] Data indicate that people who have some or other disability have more untreated caries and a higher prevalence of gingivitis and other periodontal diseases than the general population. [9],[10],[11],[12] Understanding the oral health of children with disabilities, and barriers to access of care, is of growing interest because of the significant increase in the population of children. Hence this study was undertaken with the aim of identifying various barriers by the parents which hinders them from seeking oral health care and problems of service providers in providing care to the disabled children.
Methodology:
The study was conducted in Spastics society of India, Bangalore, which is a rehabilitative institution for the disabled children. 484 children of various disabilities are being trained to cope with their disability. The institution has a medical set up to provide basic medical care facilities, but has no dental supervision. Ethical clearance was obtained from the Oxford Dental college and research centre, Bangalore. Informed consent was obtained from the caregivers before participation in the study.
The study was conducted in two parts- collection of oral data on all children was done in the first part. Dental caries were recorded in accordance with the AAPD criteria.[13] According to the AAPD Caries Risk Assessment Tools (CAT), children with disability/ special needs are considered in the high risk category. Both cavitated and non-cavitated (white spot) lesions were included. Dental caries was recorded as either present or absent. The presence of even a single carious lesion was also considered as dental caries present. The examiner was trained and calibrated in the department for recording the disease. Intra examiner diagnostic calibrations were performed for 10% of the sample and the kappa score was over 90% which was adequate.
The second part was assessing the barriers to access dental care by the parents of disabled children and dental professionals using questionnaires. A purposive sampling of 150 disabled children and their caregivers were chosen for this. For analysis, dental caries was coded as 1= caries present and 0= caries absent. Caregivers of the children with disability were interviewed on a one to one basis.
In addition, 158 dental professionals were interviewed for their difficulties in providing care to the disabled. A pretested questionnaire was constructed to evaluate the access barriers faced caregivers in getting their children’s dental needs fulfilled. The questionnaire was validated prior to the study and was administered by the investigator herself as it had the advantage of clarifying any unclear questions by respondents.
The questionnaire assessing Access problems of the caregivers were elicited , which included variables on location of the dental practice, spatial dimension, affordability, availability, dentist’s not accepting to provide treatment, acceptance of services by the parents of child, communication with the dentist and accommodation in terms of opening hours, emergency visits, late night clinics, waiting times and ease of getting an appointment.
The second section of the study encompassed interviewing dental professionals working in the nearby vicinity for their difficulties in providing dental health care to the disabled children. Questions on staff shortage, time pressure, non availability of medical management in the clinics, communication problems / availability of interpreters for them using sign language, consent issues, co-operation of patients, and lack of training during undergraduate or postgraduate courses were asked.
The data obtained was entered in an MS-Excel spreadsheet and analysed using the SPSS version 14.0. A logistic model was developed to assess this lack of perceived oral health care in the disabled children. All analysis was performed using a level of 0.05 for statistical significance.
Results
Out of 150 caregivers interviewed, responses of 149 were evaluated. 1 caregiver didn’t show keen interest in answering few questions and hence had to be excluded. Amongst the barriers to access care by the disabled, 104 (69.79%) of them felt it was very far to travel to the nearest dental practice. 48 (32.21%) of them found it difficult to physically access the clinic premises because of having to climb stairs or had to pass through a busy market area to reach the dental clinic. The social stigma of having to accompany a disabled child made the matter even worse. 113 (75.83%) caregivers experienced that having to pay for dental treatment posed as a greatest barrier to use dental services. That apart from the routine medical consultation and treatment, the dental treatment was a burden to the parents. What was of concern was during the study, caregivers were tensed that apart from the direct costs of dental treatment, there were some indirect costs which parents included in the equation about whether it was worth getting the dental treatment 72% of parents often complained that they had to take time off work regularly and the treatment was not given at single visit. Having to visit the dentist at frequent intervals made it even more difficult to access dental care. Getting them ready on time and to get them at the fixed time was also tedious. Non availability of the dentist made it difficult to access care for 37.58% of the disabled children. Improper communication with the dentist was also expressed as a constraint by 65(43.62%) of the population.
A logistic regression model was developed with disability as the independent variable and taking dental caries, location, place, expenses, availability of dentist, and willingness to treat as the covariates. Location, expensive treatment and availability of the dentist were statistically significant (p<0.05) with disability as depicted in Table 1.
158 dentists were questioned about their problems in delivering oral health care to the disabled. All professionals opined that it was very difficult to provide dental care to the disabled child in the clinic. Fear of treating uncooperative patients coupled with apprehensive parents was the main reason to not provide dental care to the disabled by most dentists (74.05%). 108( 68.35%) dentists opined that there was no adequate training to treat this section of the population. 98 ( 62.02%) reported there was staff shortage in managing these children. Non availability of medical management within the clinic or close to the patient’s home was another hindrance in rendering dental care, as reported by 52 dental professionals. 84 (53.16%) dentists reported that problems arose during treating disabled children who understood only sign language. Non availability of interpreters with them made it impossible to handle these patients. The Socio economic status of caregivers was another factor which stopped 87 (55.06%) dentists to provide oral health care to the disabled children. Table 2 depicts a model with years of practice of dentist as an independent variable developed against other variables. Lack of training, need for hospitalization, shortage of staff and lack of communication was found statistically significant with years of practice. (p<0.05).
There was a statistical difference for treating or not treating disabled children according to the time of practice. The longer the dentist practiced, the likely it was to provide active treatment. (p<0.05).
 | Table 1 : Showing Logistic Regression Model With Disability As Independent Variable Against Other Factors.
 |
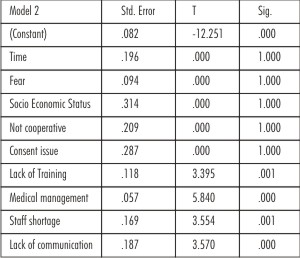 | Table 2 : Showing logistic regression model with years of practice of dentist as independent variable against other factors.
 |
Discussion:
The study was conducted in Spastics Society of India; Bangalore.150 caregivers were questioned about the access problems for dental care to the disabled children.
All caregivers expressed their difficulties in accessing dental service which is similar to studies conducted by Vignesha et al, Russell GM et al, Owens.J et al [1],[14],[15].
Amongst the caregivers interviewed, factors like cost of dental treatment as constraint was reported in 75.83% which is in accordance to Dinesh Rao etal, Doris.J.Stiefel[16],[17]. Difficulty in transportation of the children to the clinic posed as a barrier in 69.79% similar to studies of Doris.J.Stiefel[17],[18],[19].
Many of the factors identified as barriers in the present study by the caregivers such as inability to take time off employment, difficulty in accessing public transportation for the disabled were reported in previous studies [19].
Out of the 158 dental professionals who responded to the interview, 108 of them expressed lack of training and experience as a difficulty while rendering dental care to the disabled children which is in accordance to studies of Dinesh Rao,[20],[21],[22]. Insufficient time (58.22%) posed as a significant barrier in the study was also reported in Dinesh Rao [20],[21].
Because India is a male dominated society, more male children were found in institutions than their female counterparts. An effort has to be made to get these unfortunate female children to the rehabilitation centre and to provide health and oral health care.
It must be borne in mind that the caregivers of children ranging from 6-15 years were interviewed. A visit to the dentist per se can become traumatic because of different factors such as anxiety related to change in environment; lights, different noises, people, ways of dressing , tactile and sensory issues , a lack of understanding about the purpose of the visit and importance of oral health , and because of the nature of dental treatment (even if it is only a check up) and invasion of body space even in normal children. These children by the virtue of their disability are even more vulnerable.
What seems to be more important is that the literacy of the caregivers has to be improved through health education efforts.[9]. It has been observed that the literacy is low in low income families with disabled children. These struggle with directions for medications, understanding appointment slips, providing permission for informed consent and navigating health care systems to access care. This can worsen if the individual does not understand the importance of oral health and know that these oral diseases are preventable. Further research needs to be conducted in this context to determine the impact of oral health literacy for accessing oral health care.
To address this forgotten issue, the key principles of health promotion as set out in the World Health Organization’s discussion document from the Ottawa Charter [23] namely advocacy, enabling, and mediation become necessary. In this oral health promotion intervention the issue of advocacy (ensuring the creation of conditions favourable to health) is addressed by training non-dental professionals to give oral health advice, but this fails to address the structural, social, and economic inequalities experienced by neither the caregivers, nor it addresses budgetary constraints and professional role ambiguity.
Enabling (creating supportive environments and giving people the skills and information that they need to make healthy choices) is addressed by introducing oral health promoters and giving an oral health pack. This does not take into account the social determinants of health and assumes that by introducing oral health promoters, and producing a pack then inequalities will be reduced. But the greatest drawback is that the caregivers of children with disabilities were not included in building this initiative and this questions empowerment. The reality is that many caregivers of children with profound disabilities are so firmly entrenched in day-to-day living that an oral health pack will have little impact on their existence whereas a one-to-one approach that supports them and adapts approaches takes their needs and wants into consideration, and more crucially can recognize when they have the capacity to incorporate more information and alter their daily lives, but this is idealistic and still does not guarantee a reduction in inequalities. Furthermore, it raises the issue of sustainability for the whole programme.
It questions the whole enterprise of oral health promotion for children with disabilities because those most in need are still least able to respond; reflecting the‘‘Inverse Care Law’’ of Julian Tudor Hart [24]. The Inverse Care Law (Tudor Hart 1971) states that the availability of good medical care tends to vary inversely with the need for it in the population served. Those who need it the most use it the least. This principle is generally found to apply in oral health services.
A few strategies are proposed here to overcome this shortcomings and to address the oral health needs of these children.
1) Enhancing the training of dental professionals: Dental education often does not adequately train dental students to meet the needs of people with disabilities, which affects practicing dentists’ confidence and willingness to care for these patients. Appropriate formal training at both the Undergraduate and postgraduate level is necessary to equip them with necessary skills.
2) Broadening service delivery sites: Dental offices are not the only place that oral health services can be provided. Some oral health services, particularly preventive services, can be provided in settings that are closer to where people live, work, and learn.
3) Training of teachers and caregivers: Caregivers and teachers have to be adequately educated about dental problems, oral hygiene instructions and dietary practice, prevention of oro-facial trauma and first aid.
4) Creating barrier free environments: For the People with Disabilities, to be able to access and utilize oral health care services, it is of utmost importance to create barrier free environment both in the private set up as well as in the Hospitals. Recommended are the use of adjustable dental clinic, open space in clinic for maneuvering wheel chair, stabilizing devices and disable friendly toilets and lifts.
5) Integrating oral health and overall health: The dental delivery system, and oral health in general, is poorly integrated with the rest of the health care system, even though oral health is essential to daily functions of life like eating, breathing, and communicating, and there are established links between oral infections and systemic conditions like aspiration pneumonia and diabetes, and emerging links to conditions like cardiovascular disease, and pre-term and low-birth-weight births.
6) Aligning incentives: Adequate incentives for dental professionals should be provided by the Government who are involved in treatment of these children.
Conclusion:
Children with disabilities are a marginalized group who lack a voice in their own health care. Parents and care givers are children’s advocates and enablers; the more profound the impairment the greater the responsibility of care and demand on the individual learning skills and financial and energy resources of parents and paid carers. Unmet treatment need for disabled groups is universally high. Dental caries prevalence, Levels of periodontal disease tends to be higher and oral cleanliness is poorer in disabled children. Certain barriers exist which contribute to the lack of access to delivery of care; such as parental concerns about supervision and transport, financial constraints and also access to buildings. In addition, a further important barrier exists within the profession itself, as dentists are sometimes reluctant to undertake responsibility for these patients because of concerns about behavioural problems. A combination of appropriate training at both undergraduate and postgraduate level as well as the provision of appropriate secondary care facilities for those whose disabilities prevent them being treated in a general dental practice setting is suggested.
References:
1. Vignesha H, Soh G, Lo GL, Chellapah NK. Dental health of disabled children in Singapore. Aust Dent J 1991;36:151-6.
2. Halberg U, Strandmark M, Klingberg G. ‘Dental health professionals’ treatment of children with disabilities: a qualitative study.’ Acta Odontologica Scandinavica 2004;62: 319–27.
3. Halberg U, Klingsberg G. Medical health care professionals’assessments of oral health needs in children with disabilities: a qualitative study. Eur J Oral Sci 2005;113:363–8.
4. Hollister MC, Weintraub JA. The association of oral status with systemic health, quality of life, and economic productivity. J Dental Educ 1993;57:901–12.
5. Petersen PE. Socio-behavioural risk factors in dental caries –international perspectives. Comm Dentistry Oral Epidemiol 2005;33:247–9.
6. Russell GM, Kinirons MJ. A study of the barriers to dentalcare in a sample of patients with cerebral palsy. Comm Dental Health 1993;19:57–64.
7. Doris J.Stiefel. Dental care considerations for disabled adults. Spec. Care Dentist 2002;22(3):26-39.
8. National Sample Survey Organisation, Disabled Persons in India, NSS Report No. 485 December 2003, 58th round (58/26/1).
9. Mitsea AG, Karidis AG, Donta Bakayianni C, Spyropaulous ND. Oral health status in Greek children and teenagers, with disabilities. J Clin Pediatr Dent 2001;26:111-8.
10. Dinesh RB, Amitha HM, Munshi AK. Periodontal status of disabled children in South Canara, Karnataka. J Indian Dent Assoc 2003;74:559-62.
11. Murray JJ, McLeod JP. The dental condition of severely subnormal children in three London boroughs. Br Dent J 1973;134:380-5.
12. Nunn JH, Murray JJ. The dental health of handicapped children in Newcastle and Northumberland. Br Dent J 1987;162:9014.
13. American Academy of Pediatric Dentistry.Guidelines on caries-risk assessment and management for infants, children and adolescents. Pediatr Dent 2010;32(special issue):101-8.
14. Russell GM, Kinirons MJ. A study of the barriers to dental care in a sample of patients with cerebral palsy. Comm Dental Health 1993;19:57–64.
15. Owens.J. Barriers to oral health promotion in the Republic of Ireland. Scand J of Public Health 2011;39(6):93-97.
16. Rao Dinesh, Amitha Hegde, Munshi.A.K. Oral hygiene status of disabled children and adolescents attending special schools of South Canara, India. Hong Kong Dental Journal 2005;2:107-13.
17. Stiefel DJ, Truelove EL, Mandel LS. Perceived barriers vs. dental care availability for persons with disabilities. J Dent Res 1991;70:337.
18. Jedrychowski JR, Lindemann R. Dental School special patient care program during 1977-1979 and 1987-1989: Comparisons of regional and state disabled populations. Spec Care Dentist 1991;11:184-188.
19. Stephen T. Schultz, Jonathan.DS, Alice.M.Horowitz. Parental perceptions of unmet dental need and cost barriers to care for developmentally disabled children. Pediatr Dent 2001;23:321-325.
20. Zimmer S,Didner B, Roulet JF. Clinical study on the plaque removing ability of a new triple headed toothbush. J. Clin Periodontol 1999;26:281-5.
21. Hallberg U, Stradmark M, Klingberg G. Dental health professionals treatment of children with disabilities: a qualitative study. Acta Odontologica Scandinavica 2004;62:319-27.
22. Stiefel DJ, Truelove EL, Jolly DE. The preparedness of dental professionals to treat persons with disabling conditions in long term care facility and community settings. Spec Care Dentist 1987; 7:108-13.
23. World Health Organization. Ottawa charter for health promotion. Geneva: World Health Organization; 1986.
24. Tudor Hart J. The inverse care law. Lancet 1971;1:405–12
|