Introduction
The use of antiplatelet therapy has reduced the mortality and morbidity of cardiovascular disease significantly. A considerable number of patients presenting to dentist give a history of antiplatelet therapy. When patients have to undergoinvasive dental or maxillofacial treatment, dentists, oral and maxillofacial surgeons, physicians, and patients have to decide whether to continue the use of theantiplateletor to stop it temporarily to minimizethe bleeding risk associated with the surgical procedure. However, stopping this medication may lead thromboembolic events to recur, thus creating potentially hazardous situations, such as myocardial infarction, stroke, or even death. Although the recent shift from practice-based dentistry toward evidence-based dentistryhas led to the development of numerous practice guidelines to improve the delivery of health care,unfortunately this has not resultedin a practice guideline for the dental management ofpatients using antiplateletmedication.
Current indications for dual antiplatelet are twelve month post drug- eluting stent (DES) and post myocardial infarction. Risk benefit ratio is skewed toward stent thrombosis as compared to bleeding risk. In a pooled analysis of 6 trials and registries from the 1990s, the incidence of death or MI associated with angiographically documented stent thrombosis was found to be 64.4%.[1],[2] Mortality rates due to presumed or documented stent thrombosis range from 20% to 45%.[3],[4],[5] In a large observational cohort study of patients treated with DES, stent thrombosis occurred in a striking 29% of patients in whom antiplatelettherapy was discontinued prematurely.[6] In a single-site study of 652 patients treated with sirolimus DES, premature discontinuation of clopidogrel was associated with an 30-fold greater risk of stent thrombosis, with >25% of patients who discontinued clopidogrel therapy within the first month suffering stent thrombosis.[7] Park et al[8] reported on 1911 consecutive patients with DES followed up for a median of 19.4 months. Five (7.8%) of 64 patients with premature interruption of aspirin, clopidogrel, or both experienced stent thrombosis.
Despite the risk of stent thrombosis, there is still apprehension about using antiplateletin dental procedure. In our own survey physician and dentist disapproved of using antiplateletduring surgery. Despite general recommendation of continuing with antiplateletin dental procedure, risk of bleeding prelude their usage. Thus, our study aims to explore bleeding risk in patients on antiplatelet.
Material And Method
Ours was a prospective study involving 60 consecutive patients who were using single or dual antiplatelet, requiring tooth extraction. The exclusion criteria included:
1. multiple number of teeth (> 3 teeth were excluded)
2. patients with renal, haematological or liver disease
3. patients on oral anticoagulants, NSAIDS
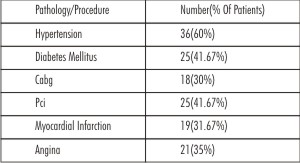 | Table 1. : Pathology or post-procedure for which the patients were taking antiplatelet therapy.
 |
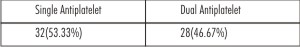 | Table 2. : Single/Dual Antiplatelet Usage
 |
 | Table 3. : Method To Stop Bleeding
 |
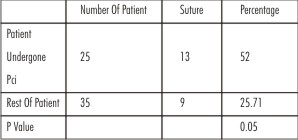 | Table 4. : Table Showing Whether Pci Subgroup Has More Bleeding Complication
 |
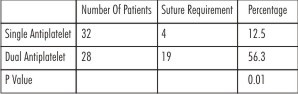 | Table 5. : Risk Of Excess Bleeding And Usage Of Antiplatelet Single Or Double
 |
The mean age was 63.48±10.67 years. 41 patients were male (68.33). A complete dental and medical history, clinical & radiographical examination were recorded. Indications for extractions were periodontitis, radicular lesion, pain, mobility and severe decay. Dental extractions were done under local anaesthesia using xylocaine. Local infiltrations and regional blocks were used in the maxilla and mandible as appropriate. Dental extraction for various etiologies were performed in all patients with a mean extraction rate of 1.65±0.55 per patient. The protocol for controlling post-operative bleeding consisted of local pressure pack for 30 minutes, sutures and medicated pressure pack. During extractions, sharp bony edges and granulation tissue were removed to make it as atraumatic as possible. A pressure gauze was then applied to the extraction site and a dry gauze was pressed down on top. The patient was monitored for 10 minutes and was then sent home with a gauze pad on the wound and the usual post-extraction written instructions (hold the gauze in place with firm pressure for ½ an hour, no mouth rinsing, liquid or soft cold diet for the first 24 hours, no spitting, warm saline rinses after 24 hours etc). For first 24 hours, the patient was asked to contact for progress and a record was made as to whether the patient had experienced any problems and, if so, the particular problems were recorded. If the bleeding did not stop with pressure gauze the decision of using medicated gauze or sutures was left to the discretion of operator.
The following was recorded in the data collection notebook: professional performing the treatment, patient’s details; age, gender, medical condition for which the antiplatelet therapy was prescribed, antiplatelet brand name and dose level, number of teeth extracted.
Results
Of the 60 patients enrolled, 41 were male (68.33%), mean age was 63.48±10.67. Majority of them had co-morbidities. Usage of double antiplatelet was in 28 patients (46.67%) implying higher risk subset.
Number of teeth extracted was 1.65±0.55%. Pressure pack was the most common 32(53.33%) modality to stop bleeding. Primary suturing was done in 21 patients with only one patient requiring suturing after 24 hours. Further analysis showed that dual antiplatelets and PCI(Per cutaneous intervention) was linked to statistically significant use of sutures. No case of re bleed, hospitalization or requiring blood transfusion was reported.
Discussion
Over the last few years, the recommendation has been to continue with the antiplatelet therapy during dental extractions[9],[10],[11],[12],[13],[14] and we have worked along these lines in our study. Patients came to the clinic of their own free will (or were referred by the primary care doctor, or by their private dentist) for a dental extraction for any type of pathology.
Patients in our study had a mean age of 63.48 years. They were having antiplatelet and we did not stop them in view of dental extraction after consultation with their physician and cardiologist. There was significant difference in bleeding that occurred during tooth extraction between the two groups. Pressure pack in most of the cases was more than sufficient to stop bleeding. Suturing was required in 36.67% of patients. Re-bleed, hospitalization and requirement of blood transfusion was nil. This alleviates our preconceived notion or fear factor for continuation of antiplatelet during operative procedure. Patient in PCI Group (52%) and on dual antiplatelet (56.3%) were more likely to require suturing but subsequent re bleed was nil. Antiplatelet are cornerstone of preventing stent thrombosis or graft occlusion in day to day practice and our study will further enforce their usage during dental procedure. The risk of post-operative bleeding complications in these patients is low , and that use of local perioperative and postoperative measures are sufficient.
Conclusion
Patients on antiplatelets requiring less than 3 tooth extractions can be safely carried out and there is no risk of re-bleed, re-admission and blood transfusion. Invasive dental procedures can be done without altering the dosage or stopping the antiplatelets. If excessive bleeding occurs, it can be controlled by local hemostatic measures. Consultation with the treating physician and cardiologist is a must. Majority of the patients on dual antiplatelets require suturing for better haemostasis to prevent re-bleed. There is a greater need for creating awareness to the dental management of this group of patients to avoid unnecessary and preventable complications.
References
1. Cutlip D.E., Baim D.S., Ho K.K.; et al. Stent thrombosis in the modern era: a pooled analysis of multicenter coronary stent clinical trials, Circulation 103 2001 1967-1971.
2. Moussa I., Di Mario C., Reimers B., Akiyama T., Tobis J., Colombo A.; Subacute stent thrombosis in the era of intravascular ultrasound-guided coronary stenting without anticoagulation: frequency, predictors and clinical outcome, J Am Coll Cardiol 29 1997 6-12
3. Spertus J.A., Kettelkamp R., Vance C.; et al. Prevalence, predictors, and outcomes of premature discontinuation of thienopyridine therapy after drug-eluting stent placement: results from the PREMIER registry, Circulation 113 2006 2803-2809
4. Pfisterer M., Brunner-LaRocca H.P., Buser P.T.; BASKET-LATE Investigators et al. Late clinical events after clopidogrel discontinuation may limit the benefit of drug-eluting stents, J Am Coll Cardiol 48 2006 2584-2591
5. Eisenstein E.L., Anstrom K.J., Kong D.F.; et al. Clopidogrel use and long-term clinical outcomes after drug-eluting stent implantation, JAMA Dec 5 2006 E1-E10
6. 6. lakovou I., Schmidt T., Bonizzoni E.; et al. Incidence, predictors, and outcome of thrombosis after successful implantation of drug-eluting stents, JAMA 293 2005 2126-2130
7. Park D.W., Park S.W., Park K.H.; et al. Frequency of and risk factors for stent thrombosis after drug-eluting stent implantation during long-term follow-up, Am J Cardiol 98 2006 352-356
8. Jeremias A., Sylvia B., Bridges J.; et al. Stent thrombosis after successful sirolimus-eluting stent implantation, Circulation 109 2004 1930-1932
9. Brennan MT, Wynn RL, Miller CS. Aspirin and bleeding in dentistry:an update and recommendations. Oral Surg Oral Med Oral Pathol Oral Radiol Endod. 2007;104:316-23.
10. Ardekian L, Gaspar R, Peled M, Brener B, Laufer D. Does lowdose aspirin therapy complicate oral surgical procedures? J Am Dent Assoc. 2000;131:331-5.
11. Madan GA, Madan SG, Madan G, Madan AD. Minor oral surgery without stopping daily low-dose aspirin therapy: a study of 51 patients. J Oral Maxillofac Surg. 2005;63:1262-5.
12. Valerin MA, Brennan MT, Noll JL, Napeñas JJ, Kent ML, Fox PC, et al. Relationship between aspirin use and postoperative bleeding from dental extractions in a healthy population [abstract]. Oral Surg Oral Med Oral Pathol Oral Radiol Endod. 2006;102:326.
13. Aframian DJ, Lalla RV, Peterson DE. Management of dental patients taking common hemostasis-altering medications. Oral Surg Oral Med Oral Pathol Oral Radiol Endod. 2007;103 Suppl:S45.e1-11.
14. Morimoto Y, Niwa H, Minematsu K. Hemostatic management oftooth extractions in patients on oral antithrombotic therapy. J Oral Maxillofac Surg. 2008;66:51-7.
|